Korean J Physiol Pharmacol.
2013 Apr;17(2):133-137. 10.4196/kjpp.2013.17.2.133.
Ginsenoside Rg2 Inhibits Lipopolysaccharide-Induced Adhesion Molecule Expression in Human Umbilical Vein Endothelial Cell
- Affiliations
-
- 1Department of Pharmacology, College of Medicine, Chungbuk National University, Cheongju 361-763, Korea. hyahn@chungbuk.ac.kr
- 2Department of Pediatrics, College of Medicine, Chungbuk National University, Cheongju 361-763, Korea.
- 3Department of Physiology, College of Medicine, Chungbuk National University, Cheongju 361-763, Korea.
- KMID: 1429384
- DOI: http://doi.org/10.4196/kjpp.2013.17.2.133
Abstract
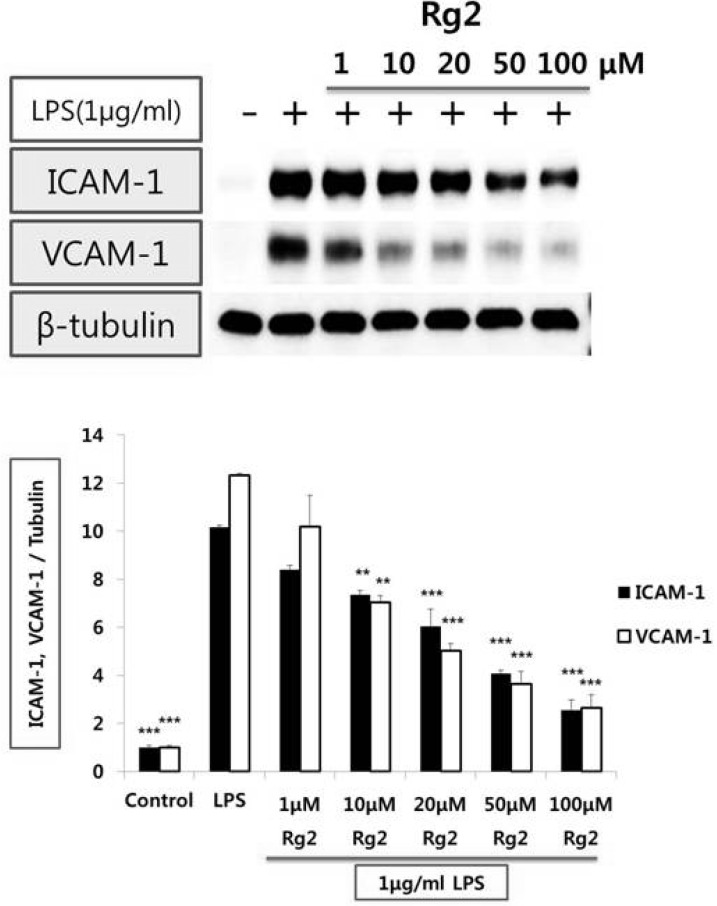
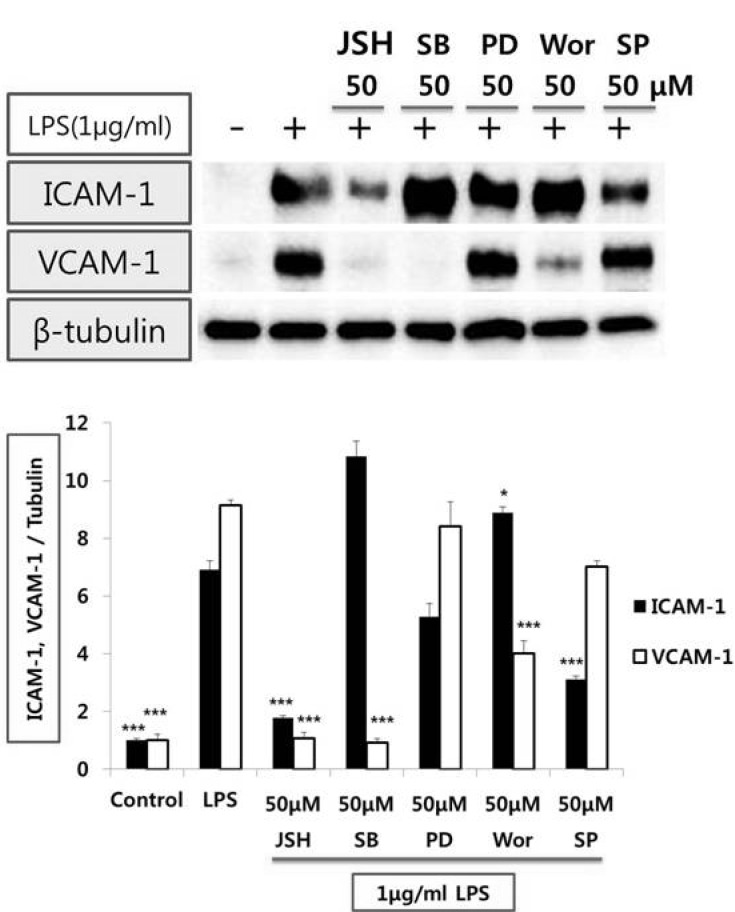
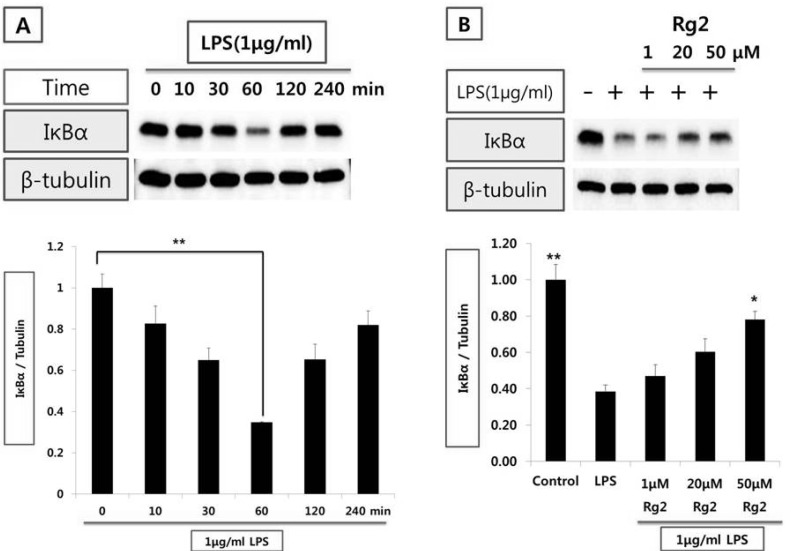
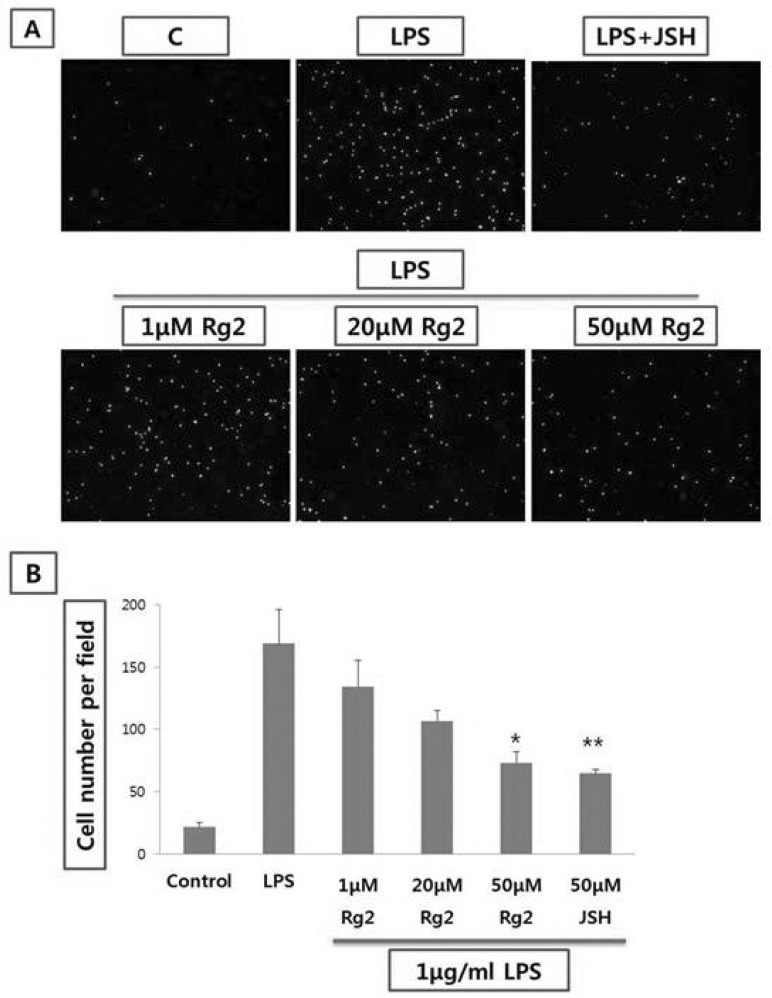
- Vascular cell adhesion molecule 1 (VCAM-1), intercellular adhesion molecule 1 (ICAM-1), P- and E-selectin play a pivotal role for initiation of atherosclerosis. Ginsenoside, a class of steroid glycosides, is abundant in Panax ginseng root, which has been used for prevention of illness in Korea. In this study, we investigated the mechanism(s) by which ginsenoside Rg2 may inhibit VCAM-1 and ICAM-1 expressions stimulated with lipopolysaccharide (LPS) in human umbilical vein endothelial cell (HUVEC). LPS increased VCAM-1 and ICAM-1 expression. Ginsenoside Rg2 prevented LPS-mediated increase of VCAM-1 and ICAM-1 expression. On the other hand, JSH, a nuclear factor kappa B (NF-kappaB) inhibitor, reduced both VCAM-1 and ICAM-1 expression stimulated with LPS. SB202190, inhibitor of p38 mitogen-activated protein kinase (p38 MAPK), and wortmannin, phosphatidylinositol 3-kinase (PI3-kinase) inhibitor, reduced LPS-mediated VCAM-1 but not ICAM-1 expression. PD98059, inhibitor of mitogen-activated protein kinase kinase/extracellular signal-regulated kinase (MEK/ERK) did not affect VCAM-1 and ICAM-1 expression stimulated with LPS. SP600125, inhibitor of c-Jun N-terminal kinase (JNK), reduced LPS-mediated ICAM-1 but not VCAM-1 expression. LPS reduced IkappaBalpha (IkappaBalpha) expression, in a time-dependent manner within 1 hr. Ginsenoside Rg2 prevented the decrease of IkappaBalpha expression stimulated with LPS. Moreover, ginsenoside Rg2 reduced LPS-mediated THP-1 monocyte adhesion to HUVEC, in a concentration-dependent manner. These data provide a novel mechanism where the ginsenoside Rg2 may provide direct vascular benefits with inhibition of leukocyte adhesion into vascular wall thereby providing protection against vascular inflammatory disease.
Keyword
MeSH Terms
-
Androstadienes
Anthracenes
Atherosclerosis
E-Selectin
Endothelial Cells
Flavonoids
Ginsenosides
Glycosides
Hand
Humans
I-kappa B Proteins
Imidazoles
Intercellular Adhesion Molecule-1
JNK Mitogen-Activated Protein Kinases
Korea
Leukocytes
Monocytes
NF-kappa B
Panax
Phosphatidylinositol 3-Kinase
Phosphotransferases
Protein Kinases
Pyridines
Umbilical Veins
Vascular Cell Adhesion Molecule-1
Androstadienes
Anthracenes
E-Selectin
Flavonoids
Ginsenosides
Glycosides
I-kappa B Proteins
Imidazoles
Intercellular Adhesion Molecule-1
JNK Mitogen-Activated Protein Kinases
NF-kappa B
Phosphatidylinositol 3-Kinase
Phosphotransferases
Protein Kinases
Pyridines
Vascular Cell Adhesion Molecule-1
Figure
Cited by 1 articles
-
Expression Profile of Neuro-Endocrine-Immune Network in Rats with Vascular Endothelial Dysfunction
Lujin Li, Zhenghua Jia, Ling Xu, Yiling Wu, Qingshan Zheng
Korean J Physiol Pharmacol. 2014;18(2):177-182. doi: 10.4196/kjpp.2014.18.2.177.
Reference
-
1. Kułdo JM, Ogawara KI, Werner N, Asgeirsdóttir SA, Kamps JA, Kok RJ, Molema G. Molecular pathways of endothelial cell activation for (targeted) pharmacological intervention of chronic inflammatory diseases. Curr Vasc Pharmacol. 2005; 3:11–39. PMID: 15638780.2. Libby P. Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutr Rev. 2007; 65:S140–S146. PMID: 18240538.
Article3. Poston RN, Haskard DO, Coucher JR, Gall NP, Johnson-Tidey RR. Expression of intercellular adhesion molecule-1 in atherosclerotic plaques. Am J Pathol. 1992; 140:665–673. PMID: 1372160.4. Mahmoudi M, Curzen N, Gallagher PJ. Atherogenesis: the role of inflammation and infection. Histopathology. 2007; 50:535–546. PMID: 17394488.
Article5. Schirmer SH, Fledderus JO, van der Laan AM, van der Pouw-Kraan TC, Moerland PD, Volger OL, Baggen JM, Böhm M, Piek JJ, Horrevoets AJ, van Royen N. Suppression of inflammatory signaling in monocytes from patients with coronary artery disease. J Mol Cell Cardiol. 2009; 46:177–185. PMID: 19059264.
Article6. Damnjanović G, Jelić M, Dindić B, Ilić S. Serum concentration of soluble adhesive molecules in patients with different forms of coronary artery disease. Vojnosanit Pregl. 2009; 66:265–270. PMID: 19432291.
Article7. Rubio-Guerra AF, Vargas-Robles H, Serrano AM, Lozano-Nuevo JJ, Escalante-Acosta BA. Correlation between the levels of circulating adhesion molecules and atherosclerosis in type-2 diabetic normotensive patients: circulating adhesion molecules and atherosclerosis. Cell Adh Migr. 2009; 3:369–372. PMID: 19717975.
Article8. Chai H, Wang Q, Huang L, Xie T, Fu Y. Ginsenoside Rb1 inhibits tumor necrosis factor-alpha-induced vascular cell adhesion molecule-1 expression in human endothelial cells. Biol Pharm Bull. 2008; 31:2050–2056. PMID: 18981572.
Article9. Wang N, Wan JB, Chan SW, Deng YH, Yu N, Zhang QW, Wang YT, Lee SM. Comparative study on saponin fractions from Panax notoginseng inhibiting inflammation-induced endothelial adhesion molecule expression and monocyte adhesion. Chin Med. 2011; 6:37. PMID: 21995855.
Article10. Lee YJ, Jin YR, Lim WC, Park WK, Cho JY, Jang S, Lee SK. Ginsenoside-Rb1 acts as a weak phytoestrogen in MCF-7 human breast cancer cells. Arch Pharm Res. 2003; 26:58–63. PMID: 12568360.
Article11. Korivi M, Hou CW, Huang CY, Lee SD, Hsu MF, Yu SH, Chen CY, Liu YY, Kuo CH. Ginsenoside-Rg1 protects the liver against exhaustive exercise-induced oxidative stress in rats. Evid Based Complement Alternat Med. 2012; 2012:932165. PMID: 21941591.
Article12. Zhang G, Liu A, Zhou Y, San X, Jin T, Jin Y. Panax ginseng ginsenoside-Rg2 protects memory impairment via anti-apoptosis in a rat model with vascular dementia. J Ethnopharmacol. 2008; 115:441–448. PMID: 18083315.
Article13. Wan JB, Lee SM, Wang JD, Wang N, He CW, Wang YT, Kang JX. Panax notoginseng reduces atherosclerotic lesions in ApoE-deficient mice and inhibits TNF-alpha-induced endothelial adhesion molecule expression and monocyte adhesion. J Agric Food Chem. 2009; 57:6692–6697. PMID: 19722574.14. Dou L, Lu Y, Shen T, Huang X, Man Y, Wang S, Li J. Panax notogingseng saponins suppress RAGE/MAPK signaling and NF-kappaB activation in apolipoprotein-E-deficient atherosclerosis-prone mice. Cell Physiol Biochem. 2012; 29:875–882. PMID: 22613987.15. Rockel C, Hartung T. Systematic review of membrane components of gram-positive bacteria responsible as pyrogens for inducing human monocyte/macrophage cytokine release. Front Pharmacol. 2012; 3:56. PMID: 22529809.
Article16. Hien TT, Kim ND, Kim HS, Kang KW. Ginsenoside Rg3 inhibits tumor necrosis factor-alpha-induced expression of cell adhesion molecules in human endothelial cells. Pharmazie. 2010; 65:699–701. PMID: 21038849.17. Monaco C, Paleolog E. Nuclear factor kappaB: a potential therapeutic target in atherosclerosis and thrombosis. Cardiovasc Res. 2004; 61:671–682. PMID: 14985064.18. Kim SW, Kim CE, Kim MH. Flavonoids inhibit high glucose-induced up-regulation of ICAM-1 via the p38 MAPK pathway in human vein endothelial cells. Biochem Biophys Res Commun. 2011; 415:602–607. PMID: 22074828.
Article19. Zhang XL, Wen L, Chen YJ, Zhu Y. Vascular endothelial growth factor up-regulates the expression of intracellular adhesion molecule-1 in retinal endothelial cells via reactive oxygen species, but not nitric oxide. Chin Med J (Engl). 2009; 122:338–343. PMID: 19236815.20. Ho AW, Wong CK, Lam CW. Tumor necrosis factor-alpha up-regulates the expression of CCL2 and adhesion molecules of human proximal tubular epithelial cells through MAPK signaling pathways. Immunobiology. 2008; 213:533–544. PMID: 18656701.21. Tang G, Minemoto Y, Dibling B, Purcell NH, Li Z, Karin M, Lin A. Inhibition of JNK activation through NF-kappaB target genes. Nature. 2001; 414:313–317. PMID: 11713531.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Allicin Reduces Adhesion Molecules and NO Production Induced by gamma irradiation in Human Endothelial Cells
- Increased expression of adhesion molecules on human umbilical vein endothelial cells by Orientia tsutsugamushi infection
- Genipin Selectively Inhibits TNF-alpha-activated VCAM-1 But Not ICAM-1 Expression by Upregulation of PPAR-gamma in Human Endothelial Cells
- Effect of VCAM-1 expression in human endothelial cells by proinflammatory cytokines
- Protective Effect of Allium tuberosum Extract on Vascular Inflammation in Tumor Necrosis Factor-α-induced Human Vascular Endothelial Cells