Allergy Asthma Respir Dis.
2015 Sep;3(5):313-319. 10.4168/aard.2015.3.5.313.
Effects of particulate matter in ambient air on the development and control of asthma
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Soonchunhyang University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Eulji University School of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Allergy and Clinical Immunology, University of Ulsan College of Medicine, Seoul, Korea.
- 7Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea.
- 8Department of Pediatrics, Korea University College of Medicine, Seoul, Korea.
- 9Department of Pediatrics, University of Ulsan College of Medicine, Seoul, Korea.
- 10Department of Pediatrics, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 11Department of Pediatrics, CHA University School of Medicine, Pocheon, Korea.
- 12Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- 13Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea. cwkim1805@inha.ac.kr
- KMID: 2218640
- DOI: http://doi.org/10.4168/aard.2015.3.5.313
Abstract
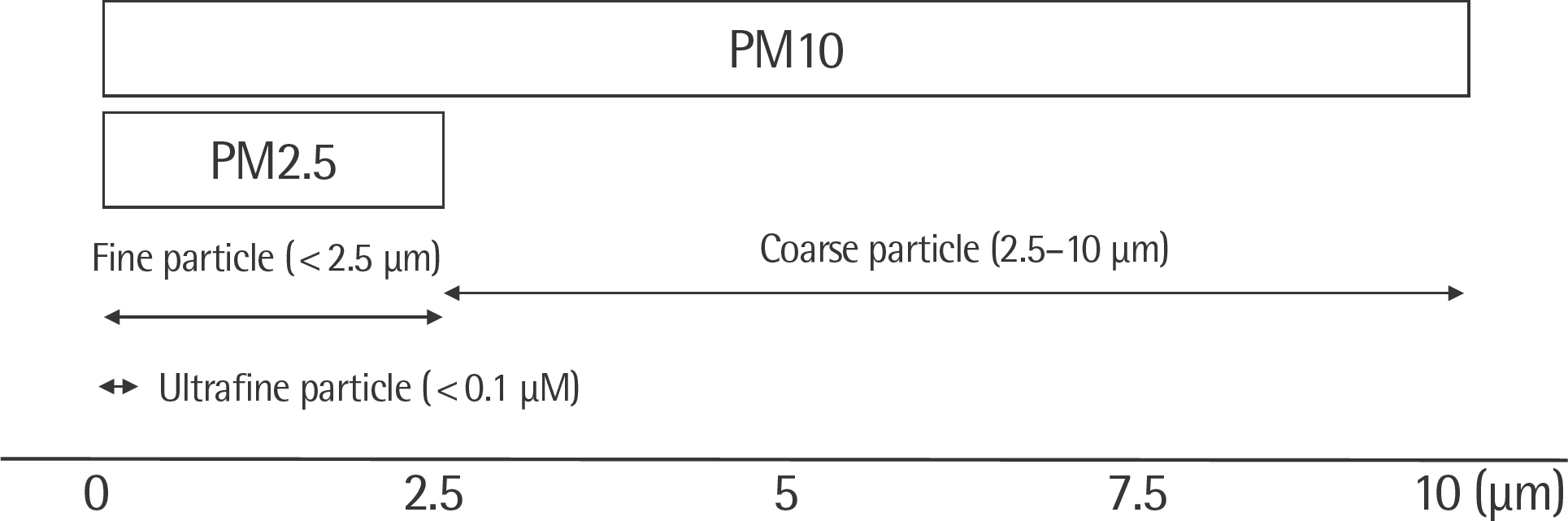
- There has been growing concern regarding the effects of ambient air pollution on asthma. Particulate matter (PM) is one of the major air pollutants affecting both general population and the patients with asthma. This paper reviews the recent evidence of the adverse effects of PM on the inception and morbidity of asthma. Epidemiological studies confirmed that short-term exposure to PM aggravated respiratory symptoms and lung function in asthma patients. Furthermore, PM induces acute exacerbations of asthma with increased risk of hospitalization and death. Long-term exposure to PM is responsible for new onset of asthma and lung function decline in both children and adults. Various mechanisms are involved in the effects of PM on airway including oxidative stress, augmentation of inflammation, promotion of allergen sensitization, induction of airway hyperresponsiveness, aggravation of rhinitis and DNA methylation. Special attention and care is needed for the patients with asthma to prevent the detrimental effects of PM.
MeSH Terms
Figure
Cited by 3 articles
-
Survey on Awareness for Environmental Health Risk of Fetus and Infant in Reproductive-aged Women
Jiyoung Shin, Eunkyo Park, Jungeun Shin, Eun-Hee Ha
Ewha Med J. 2018;41(2):35-43. doi: 10.12771/emj.2018.41.2.35.Relation of Nutritional Intake and Allergic Rhinitis in Infants: Using the Korea National Health and Nutrition Examination Survey (KNHANES) 2013~2016
Eun-Sil Her, Bo-Young Seo
Korean J Community Nutr. 2019;24(4):321-330. doi: 10.5720/kjcn.2019.24.4.321.The impact of indoor air pollution on asthma
Dong Won Park, Sang-Heon Kim, Ho Joo Yoon
Allergy Asthma Respir Dis. 2017;5(6):312-319. doi: 10.4168/aard.2017.5.6.312.
Reference
-
References
1. Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006; 355:2226–35.
Article2. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014; 383:1581–92.
Article3. Ahmed E, Kim KH, Shon ZH, Song SK. Longterm trend of airborne particulate matter in Seoul, Korea from 2004 to 2013. Atmos Environ. 2015; 101:125–33.
Article4. Kim HS, Chung YS, Yoon MB. An analysis on the impact of large-scale transports of dust pollution on air quality in East Asia as observed in central Korea in 2014. Air Qual Atmos Health. 2015 Jan 15. [Epub].http://dx.doi.org/10.1007/s11869-014-0312-5.
Article5. Asgharian B, Price OT, Oldham M, Chen LC, Saunders EL, Gordon T, et al. Computational modeling of nanoscale and microscale particle deposition, retention and dosimetry in the mouse respiratory tract. Inhal Toxicol. 2014; 26:829–42.
Article6. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010; 121:2331–78.7. Utell MJ, Frampton MW. Acute health effects of ambient air pollution: the ultrafine particle hypothesis. J Aerosol Med. 2000; 13:355–59.
Article8. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009; 180:59–99.9. Ostro B, Lipsett M, Mann J, Braxton-Owens H, White M. Air pollution and exacerbation of asthma in African-American children in Los Angeles. Epidemiology. 2001; 12:200–8.
Article10. Tecer LH, Alagha O, Karaca F, Tuncel G, Eldes N. Particulate matter (PM(2.5), PM(10–2.5), and PM(10)) and children's hospital admissions for asthma and respiratory diseases: a bidirectional case-crossover study. J Toxicol Environ Health A. 2008; 71:512–20.
Article11. Samoli E, Nastos PT, Paliatsos AG, Katsouyanni K, Priftis KN. Acute effects of air pollution on pediatric asthma exacerbation: evidence of association and effect modification. Environ Res. 2011; 111:418–24.
Article12. Meng YY, Rull RP, Wilhelm M, Lombardi C, Balmes J, Ritz B. Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. J Epidemiol Community Health. 2010; 64:142–7.
Article13. Mann JK, Balmes JR, Bruckner TA, Mortimer KM, Margolis HG, Pratt B, et al. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environ Health Perspect. 2010; 118:1497–502.
Article14. Lee JT, Kim H, Song H, Hong YC, Cho YS, Shin SY, et al. Air pollution and asthma among children in Seoul, Korea. Epidemiology. 2002; 13:481–4.
Article15. Malig BJ, Green S, Basu R, Broadwin R. Coarse particles and respiratory emergency department visits in California. Am J Epidemiol. 2013; 178:58–69.
Article16. Delamater PL, Finley AO, Banerjee S. An analysis of asthma hospitalizations, air pollution, and weather conditions in Los Angeles County, California. Sci Total Environ. 2012; 425:110–8.
Article17. Silverman RA, Ito K. Age-related association of fine particles and ozone with severe acute asthma in New York City. J Allergy Clin Immunol. 2010; 125:367–73.e5.
Article18. Jang AS, Kim BY, Lee CH, Park JS, Lee JH, Park SW, et al. Hospital visits and admissions in patients with asthma, COPD, and cardiovascular diseases according to air pollutants. Korean J Asthma Allergy Clin Immunol. 2006; 26:233–8.19. Schildcrout JS, Sheppard L, Lumley T, Slaughter JC, Koenig JQ, Shapiro GG. Ambient air pollution and asthma exacerbations in children: an eight-city analysis. Am J Epidemiol. 2006; 164:505–17.
Article20. Kim SH, Son JY, Lee JT, Kim TB, Park HW, Lee JH, et al. Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea: a case-crossover study. Korean J Med. 2010; 78:450–6.21. Peng RD, Chang HH, Bell ML, McDermott A, Zeger SL, Samet JM, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. JAMA. 2008; 299:2172–9.
Article22. Iskandar A, Andersen ZJ, Bonnelykke K, Ellermann T, Andersen KK, Bisgaard H. Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax. 2012; 67:252–7.
Article23. Ko FW, Tam W, Wong TW, Lai CK, Wong GW, Leung TF, et al. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin Exp Allergy. 2007; 37:1312–9.
Article24. Park M, Luo S, Kwon J, Stock TH, Delclos G, Kim H, et al. Effects of air pollution on asthma hospitalization rates in different age groups in metropolitan cities of Korea. Air Qual Atmos Health. 2013; 6:http://dx.doi.org/10.1007/s11869-013-0195-x.
Article25. Schindler C, Kunzli N, Bongard JP, Leuenberger P, Karrer W, Rapp R, et al. Short-term variation in air pollution and in average lung function among never-smokers. The Swiss Study on Air Pollution and Lung Diseases in Adults (SAPALDIA). Am J Respir Crit Care Med. 2001; 163:356–61.26. Lee JT, Son JY, Cho YS. The adverse effects of fine particle air pollution on respiratory function in the elderly. Sci Total Environ. 2007; 385:28–36.
Article27. Son JY, Bell ML, Lee JT. Individual exposure to air pollution and lung function in Korea: spatial analysis using multiple exposure approaches. Environ Res. 2010; 110:739–49.
Article28. Trenga CA, Sullivan JH, Schildcrout JS, Shepherd KP, Shapiro GG, Liu LJ, et al. Effect of particulate air pollution on lung function in adult and pediatric subjects in a Seattle panel study. Chest. 2006; 129:1614–22.
Article29. Liu L, Poon R, Chen L, Frescura AM, Montuschi P, Ciabattoni G, et al. Acute effects of air pollution on pulmonary function, airway inflammation, and oxidative stress in asthmatic children. Environ Health Perspect. 2009; 117:668–74.
Article30. Rice MB, Ljungman PL, Wilker EH, Gold DR, Schwartz JD, Koutrakis P, et al. Short-term exposure to air pollution and lung function in the Framingham Heart Study. Am J Respir Crit Care Med. 2013; 188:1351–7.
Article31. Pope CA 3rd, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE, et al. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med. 1995; 151(3 Pt 1):669–74.
Article32. Romieu I, Gouveia N, Cifuentes LA, de Leon AP, Junger W, Vera J, et al. Multicity study of air pollution and mortality in Latin America (the ES-CALA study). Res Rep Health Eff Inst. 2012; 171:5–86.33. Son JY, Bell ML. The relationships between short-term exposure to particulate matter and mortality in Korea: Impact of particulate matter exposure metrics for sub-daily exposures. Environ Res Lett. 2013; 8:014015.
Article34. Bråbäck L, Forsberg B. Does traffic exhaust contribute to the development of asthma and allergic sensitization in children: findings from recent cohort studies. Environ Health. 2009; 8:17.
Article35. Jacquemin B, Schikowski T, Carsin AE, Hansell A, Kramer U, Sunyer J, et al. The role of air pollution in adult-onset asthma: a review of the current evidence. Semin Respir Crit Care Med. 2012; 33:606–19.
Article36. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007; 29:879–88.
Article37. Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010; 181:596–603.
Article38. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Kramer U, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008; 177:1331–7.
Article39. Kim BJ, Lee SY, Kwon JW, Jung YH, Lee E, Yang SI, et al. Traffic-related air pollution is associated with airway hyperresponsiveness. J Allergy Clin Immunol. 2014; 133:1763–5.e2.
Article40. Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a metaanalysis of birth cohort studies. Allergy. 2015; 70:245–56.
Article41. Jacquemin B, Sunyer J, Forsberg B, Aguilera I, Briggs D, Garcia-Esteban R, et al. Home outdoor NO2 and new onset of self-reported asthma in adults. Epidemiology. 2009; 20:119–26.
Article42. Jacquemin B, Siroux V, Sanchez M, Carsin AE, Schikowski T, Adam M, et al. Ambient air pollution and adult asthma incidence in six European cohorts (ESCAPE). Environ Health Perspect. 2015; 123:613–21.
Article43. McDonnell WF, Abbey DE, Nishino N, Lebowitz MD. Longterm ambient ozone concentration and the incidence of asthma in nonsmoking adults: the AHSMOG Study. Environ Res. 1999; 80(2 Pt 1):110–21.
Article44. Künzli N, Bridevaux PO, Liu LJ, Garcia-Esteban R, Schindler C, Gerbase MW, et al. Traffic-related air pollution correlates with adult-onset asthma among never-smokers. Thorax. 2009; 64:664–70.
Article45. Young MT, Sandler DP, DeRoo LA, Vedal S, Kaufman JD, London SJ. Ambient air pollution exposure and incident adult asthma in a nationwide cohort of U.S. women. Am J Respir Crit Care Med. 2014; 190:914–21.
Article46. Jacquemin B, Kauffmann F, Pin I, Le Moual N, Bousquet J, Gormand F, et al. Air pollution and asthma control in the Epidemiological study on the Genetics and Environment of Asthma. J Epidemiol Community Health. 2012; 66:796–802.
Article47. Bai TR, Vonk JM, Postma DS, Boezen HM. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J. 2007; 30:452–6.
Article48. Rice MB, Ljungman PL, Wilker EH, Dorans KS, Gold DR, Schwartz J, et al. Longterm exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am J Respir Crit Care Med. 2015; 191:656–64.
Article49. Forbes LJ, Kapetanakis V, Rudnicka AR, Cook DG, Bush T, Stedman JR, et al. Chronic exposure to outdoor air pollution and lung function in adults. Thorax. 2009; 64:657–63.
Article50. Downs SH, Schindler C, Liu LJ, Keidel D, Bayer-Oglesby L, Brutsche MH, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med. 2007; 357:2338–47.51. Ghio AJ. Mechanism of asthmatic exacerbation by ambient air pollution particles. Expert Rev Respir Med. 2008; 2:109–18.
Article52. Sierra-Vargas MP, Guzman-Grenfell AM, Blanco-Jimenez S, Sepulveda-Sanchez JD, Bernabe-Cabanillas RM, Cardenas-Gonzalez B, et al. Airborne particulate matter PM2.5 from Mexico City affects the generation of reactive oxygen species by blood neutrophils from asthmatics: an in vitro approach. J Occup Med Toxicol. 2009; 4:17.
Article53. Canova C, Dunster C, Kelly FJ, Minelli C, Shah PL, Caneja C, et al. PM10-induced hospital admissions for asthma and chronic obstructive pulmonary disease: the modifying effect of individual characteristics. Epidemiology. 2012; 23:607–15.54. Reddy P, Naidoo RN, Robins TG, Mentz G, Li H, London SJ, et al. GSTM1 and GSTP1 gene variants and the effect of air pollutants on lung function measures in South African children. Am J Ind Med. 2012; 55:1078–86.55. Chan JK, Kodani SD, Charrier JG, Morin D, Edwards PC, Anderson DS, et al. Age-specific effects on rat lung glutathione and antioxidant enzymes after inhaling ultrafine soot. Am J Respir Cell Mol Biol. 2013; 48:114–24.
Article56. Watanabe M, Kurai J, Tomita K, Sano H, Abe S, Saito R, et al. Effects on asthma and induction of interleukin-8 caused by Asian dust particles collected in western Japan. J Asthma. 2014; 51:595–602.
Article57. Saunders V, Breysse P, Clark J, Sproles A, Davila M, Wills-Karp M. Particulate matter-induced airway hyperresponsiveness is lymphocyte dependent. Environ Health Perspect. 2010; 118:640–6.
Article58. Shadie AM, Herbert C, Kumar RK. Ambient particulate matter induces an exacerbation of airway inflammation in experimental asthma: role of interleukin-33. Clin Exp Immunol. 2014; 177:491–9.
Article59. Kim J, Natarajan S, Vaickus LJ, Bouchard JC, Beal D, Cruikshank WW, et al. Diesel exhaust particulates exacerbate asthma-like inflammation by increasing CXC chemokines. Am J Pathol. 2011; 179:2730–9.
Article60. Hirota JA, Gold MJ, Hiebert PR, Parkinson LG, Wee T, Smith D, et al. The nucleotide-binding domain, leucine-rich repeat protein 3 inflamma-some/IL-1 receptor I axis mediates innate, but not adaptive, immune responses after exposure to particulate matter under 10 μm. Am J Respir Cell Mol Biol. 2015; 52:96–105.
Article61. North ML, Amatullah H, Khanna N, Urch B, Grasemann H, Silverman F, et al. Augmentation of arginase 1 expression by exposure to air pollution exacerbates the airways hyperresponsiveness in murine models of asthma. Respir Res. 2011; 12:19.
Article62. Pénard-Morand C, Raherison C, Charpin D, Kopferschmitt C, Lavaud F, Caillaud D, et al. Longterm exposure to close-proximity air pollution and asthma and allergies in urban children. Eur Respir J. 2010; 36:33–40.63. Brandt EB, Biagini Myers JM, Acciani TH, Ryan PH, Sivaprasad U, Ruff B, et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J Allergy Clin Immunol. 2015; 136:295–303.e7.
Article64. Jang AS, Yeum CH, Son MH. Epidemiologic evidence of a relationship between airway hyperresponsiveness and exposure to polluted air. Allergy. 2003; 58:585–8.
Article65. Wang T, Moreno-Vinasco L, Huang Y, Lang GD, Linares JD, Goonewar-dena SN, et al. Murine lung responses to ambient particulate matter: genomic analysis and influence on airway hyperresponsiveness. Environ Health Perspect. 2008; 116:1500–8.
Article66. Willers SM, Eriksson C, Gidhagen L, Nilsson ME, Pershagen G, Belland-er T. Fine and coarse particulate air pollution in relation to respiratory health in Sweden. Eur Respir J. 2013; 42:924–34.
Article67. Zhang F, Wang W, Lv J, Krafft T, Xu J. Time-series studies on air pollution and daily outpatient visits for allergic rhinitis in Beijing, China. Sci Total Environ. 2011; 409:2486–92.
Article68. Annesi-Maesano I, Agabiti N, Pistelli R, Couilliot MF, Forastiere F. Subpopulations at increased risk of adverse health outcomes from air pollution. Eur Respir J Suppl. 2003; 40:57s–63s.
Article69. Dong GH, Qian Z, Liu MM, Wang D, Ren WH, Fu Q, et al. Obesity enhanced respiratory health effects of ambient air pollution in Chinese children: the Seven Northeastern Cities study. Int J Obes (Lond). 2013; 37:94–100.
Article70. Lee SY, Chang YS, Cho SH. Allergic diseases and air pollution. Asia Pac Allergy. 2013; 3:145–54.
Article71. Sofer T, Baccarelli A, Cantone L, Coull B, Maity A, Lin X, et al. Exposure to airborne particulate matter is associated with methylation pattern in the asthma pathway. Epigenomics. 2013; 5:147–54.
Article72. Baccarelli A, Wright RO, Bollati V, Tarantini L, Litonjua AA, Suh HH, et al. Rapid DNA methylation changes after exposure to traffic particles. Am J Respir Crit Care Med. 2009; 179:572–8.
Article73. Madrigano J, Baccarelli A, Mittleman MA, Wright RO, Sparrow D, Voko-nas PS, et al. Prolonged exposure to particulate pollution, genes associated with glutathione pathways, and DNA methylation in a cohort of older men. Environ Health Perspect. 2011; 119:977–82.
Article