Korean J Physiol Pharmacol.
2015 Jan;19(1):1-7. 10.4196/kjpp.2015.19.1.1.
Berberine Prevents Intestinal Mucosal Barrier Damage During Early Phase of Sepsis in Rat through the Toll-Like Receptors Signaling Pathway
- Affiliations
-
- 1Department of General Surgery, Tianjin Union Medical Center, The Affiliated Hospital of Nankai University, Tianjin 300121, P.R. China.
- 2Department of General Surgery, Nanjing Jinling Hospital, Nanjing University, Nanjing 210002, P.R. China. liningpre@163.com
- KMID: 2071812
- DOI: http://doi.org/10.4196/kjpp.2015.19.1.1
Abstract
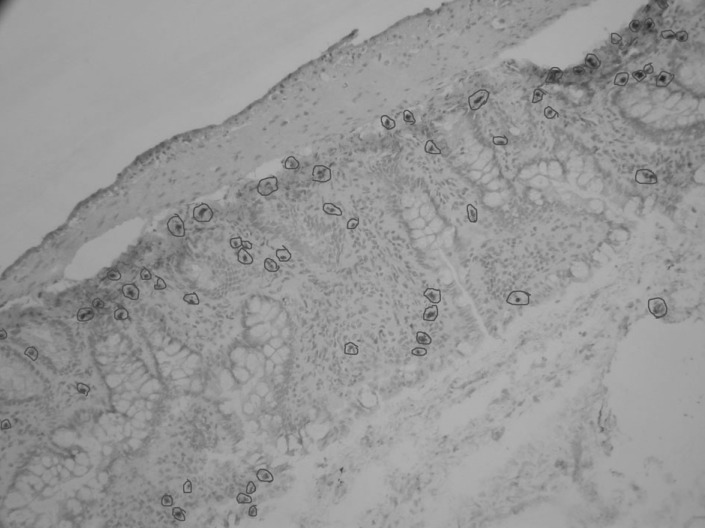
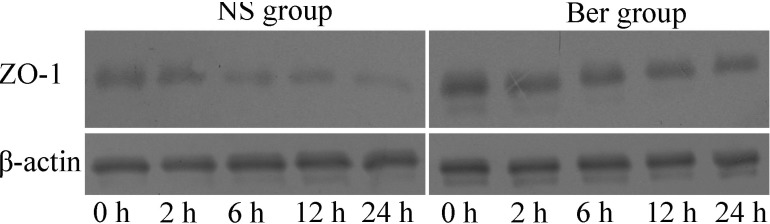
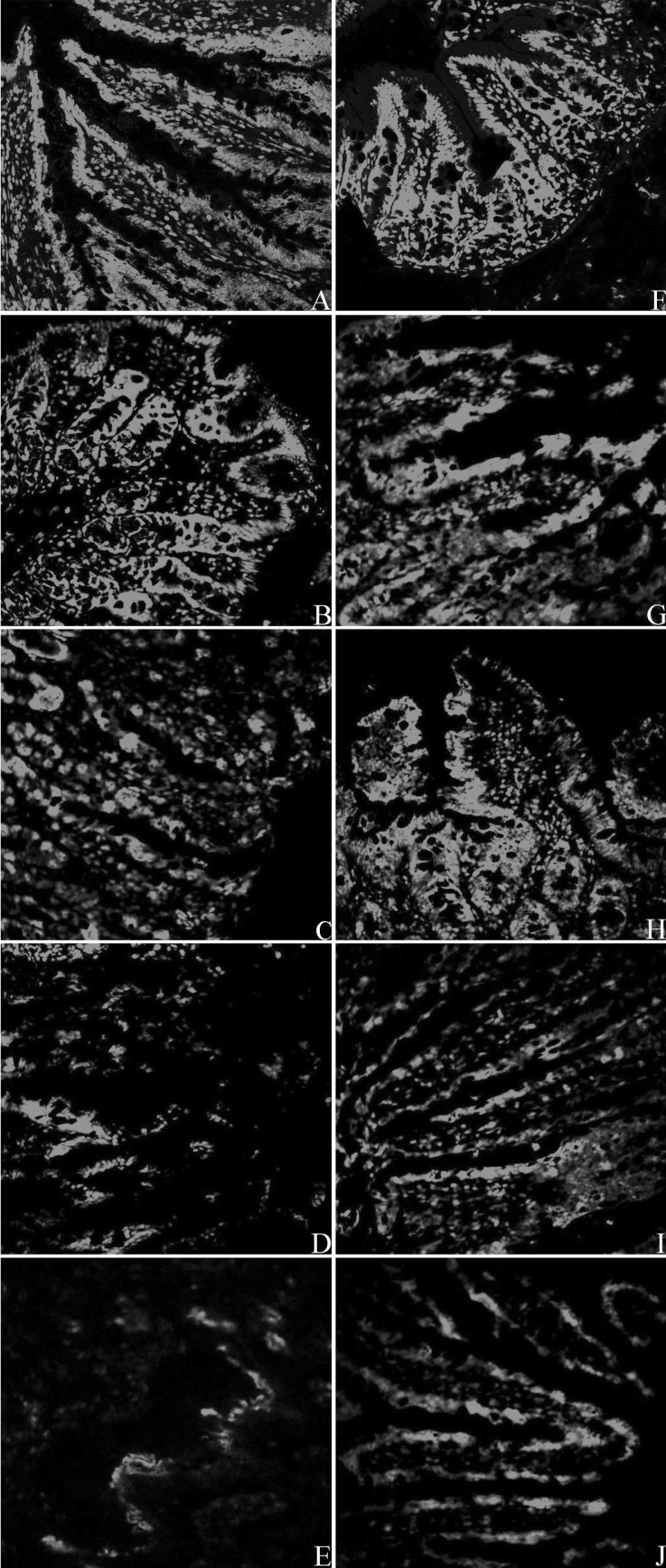
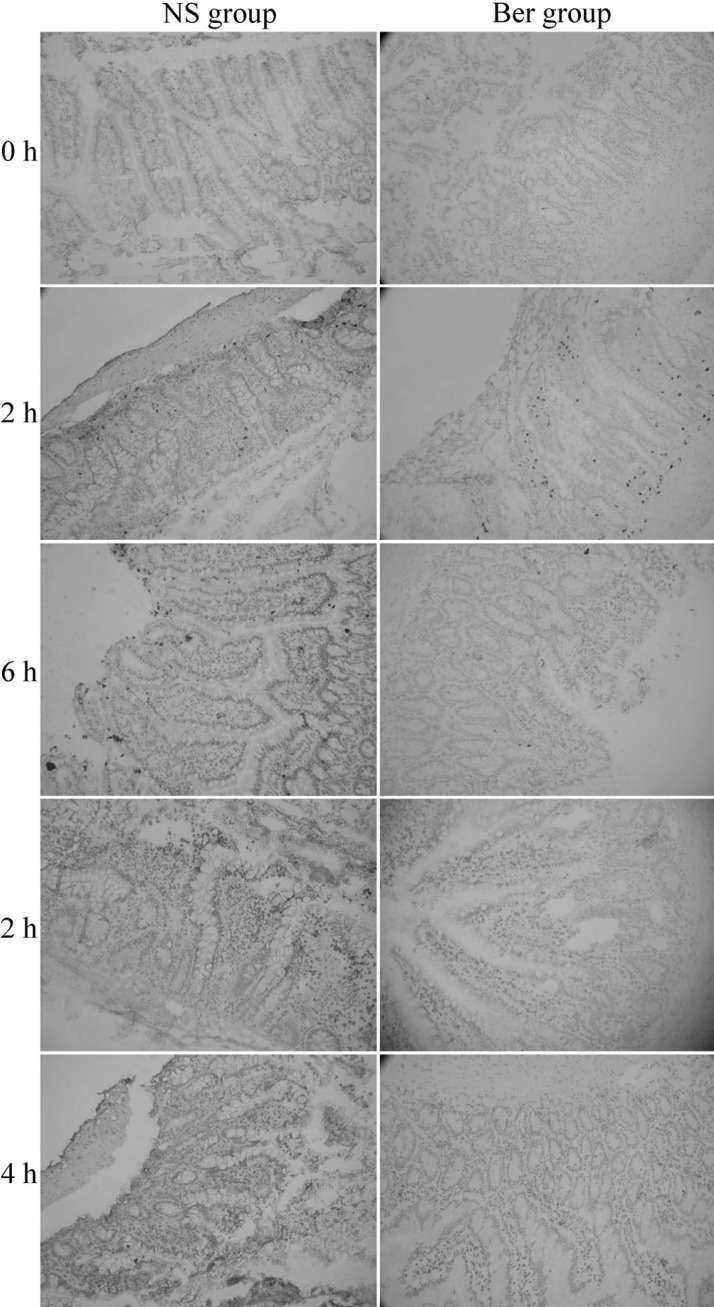
- Our previous study has shown berberine prevents damage to the intestinal mucosal barrier during early phase of sepsis in rat through mechanisms independent of the NOD-like receptors signaling pathway. In this study, we explored the regulatory effects of berberine on Toll-like receptors during the intestinal mucosal damaging process in rats. Male Sprague-Dawlay (SD) rats were treated with berberine for 5 d before undergoing cecal ligation and puncture (CLP) to induce polymicrobial sepsis. The expression of Toll-like receptor 2 (TLR 2), TLR 4, TLR 9, the activity of nuclear factor-kappa B (NF-kappaB), the levels of selected cytokines and chemokines, percentage of cell death in intestinal epithelial cells, and mucosal permeability were investigated at 0, 2, 6, 12 and 24 h after CLP. Results showed that the tumor necrosis factor-alpha (TNF-alpha ) and interleukin-6 (IL-6) level were significantly lower in berberine-treated rats compared to the control animals. Conversely, the expression level of tight junction proteins, percentage of cell death in intestinal epithelial cells and the mucosal permeability were significantly higher in berberine-treated rats. The mRNA expression of TLR 2, TLR 4, and TLR 9 were significantly affected by berberine treatment. Our results indicate that pretreatment with berberine attenuates tissue injury and protects the intestinal mucosal barrier in early phase of sepsis and this may possibly have been mediated through the TLRs pathway.
Keyword
MeSH Terms
-
Animals
Berberine*
Cell Death
Chemokines
Cytokines
Epithelial Cells
Humans
Interleukin-6
Intraabdominal Infections
Ligation
Male
Permeability
Punctures
Rats*
RNA, Messenger
Sepsis*
Tight Junction Proteins
Toll-Like Receptor 2
Toll-Like Receptors*
Tumor Necrosis Factor-alpha
Berberine
Chemokines
Cytokines
Interleukin-6
RNA, Messenger
Tight Junction Proteins
Toll-Like Receptor 2
Toll-Like Receptors
Tumor Necrosis Factor-alpha
Figure
Cited by 3 articles
-
Sepsis induces variation of intestinal barrier function in different phase through nuclear factor kappa B signaling
Ying-Ya Cao, Zhong-Han Wang, Qian-Cheng Xu, Qun Chen, Zhen Wang, Wei-Hua Lu
Korean J Physiol Pharmacol. 2021;25(4):375-383. doi: 10.4196/kjpp.2021.25.4.375.Epigallocatechin-3-Gallate (EGCG) Attenuates Traumatic Brain Injury by Inhibition of Edema Formation and Oxidative Stress
Bo Zhang, Bing Wang, Shuhua Cao, Yongqiang Wang
Korean J Physiol Pharmacol. 2015;19(6):491-497. doi: 10.4196/kjpp.2015.19.6.491.Resveratrol attenuates lipopolysaccharide-induced dysfunction of blood-brain barrier in endothelial cells via AMPK activation
Min Hu, Bo Liu
Korean J Physiol Pharmacol. 2016;20(4):325-332. doi: 10.4196/kjpp.2016.20.4.325.
Reference
-
1. Cribbs SK, Martin GS. Expanding the global epidemiology of sepsis. Crit Care Med. 2007; 35:2646–2648. PMID: 18075373.
Article2. Macdonald J, Galley HF, Webster NR. Oxidative stress and gene expression in sepsis. Br J Anaesth. 2003; 90:221–232. PMID: 12538380.
Article3. De-Souza DA, Greene LJ. Intestinal permeability and systemic infections in critically ill patients: effect of glutamine. Crit Care Med. 2005; 33:1125–1135. PMID: 15891348.
Article4. Doig CJ, Sutherland LR, Sandham JD, Fick GH, Verhoef M, Meddings JB. Increased intestinal permeability is associated with the development of multiple organ dysfunction syndrome in critically ill ICU patients. Am J Respir Crit Care Med. 1998; 158:444–451. PMID: 9700119.
Article5. Yu P, Martin CM. Increased gut permeability and bacterial translocation in Pseudomonas pneumonia-induced sepsis. Crit Care Med. 2000; 28:2573–2577. PMID: 10921597.
Article6. Madara JL. Warner-Lambert/Parke-Davis Award lecture. Pathobiology of the intestinal epithelial barrier. Am J Pathol. 1990; 137:1273–1281. PMID: 2260620.7. Suzuki T. Regulation of intestinal epithelial permeability by tight junctions. Cell Mol Life Sci. 2013; 70:631–659. PMID: 22782113.
Article8. Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009; 9:799–809. PMID: 19855405.
Article9. Cao M, Wang P, Sun C, He W, Wang F. Amelioration of IFN-γ and TNF-α-induced intestinal epithelial barrier dysfunction by berberine via suppression of MLCK-MLC phosphorylation signaling pathway. PLoS One. 2013; 8:e61944. PMID: 23671580.
Article10. Kong DX, Li XJ, Tang GY, Zhang HY. How many traditional Chinese medicine components have been recognized by modern Western medicine? A chemoinformatic analysis and implications for finding multicomponent drugs. Chem Med Chem. 2008; 3:233–236. PMID: 18022980.
Article11. Zeng XH, Zeng XJ, Li YY. Efficacy and safety of berberine for congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 2003; 92:173–176. PMID: 12860219.
Article12. Zhang Q, Piao XL, Piao XS, Lu T, Wang D, Kim SW. Preventive effect of Coptis chinensis and berberine on intestinal injury in rats challenged with lipopolysaccharides. Food Chem Toxicol. 2011; 49:61–69. PMID: 20932871.
Article13. Dvorák Z, Vrzal R, Maurel P, Ulrichová J. Differential effects of selected natural compounds with anti-inflammatory activity on the glucocorticoid receptor and NF-kappaB in HeLa cells. Chem Biol Interact. 2006; 159:117–128. PMID: 16289013.14. Hsiang CY, Wu SL, Cheng SE, Ho TY. Acetaldehyde-induced interleukin-1beta and tumor necrosis factor-alpha production is inhibited by berberine through nuclear factor-kappaB signaling pathway in HepG2 cells. J Biomed Sci. 2005; 12:791–801. PMID: 16132116.15. Jeong HW, Hsu KC, Lee JW, Ham M, Huh JY, Shin HJ, Kim WS, Kim JB. Berberine suppresses proinflammatory responses through AMPK activation in macrophages. Am J Physiol Endocrinol Metab. 2009; 296:E955–E964. PMID: 19208854.
Article16. Kuo CL, Chi CW, Liu TY. The anti-inflammatory potential of berberine in vitro and in vivo. Cancer Lett. 2004; 203:127–137. PMID: 14732220.
Article17. Lee DU, Kang YJ, Park MK, Lee YS, Seo HG, Kim TS, Kim CH, Chang KC. Effects of 13-alkyl-substituted berberine alkaloids on the expression of COX-II, TNF-alpha, iNOS, and IL-12 production in LPS-stimulated macrophages. Life Sci. 2003; 73:1401–1412. PMID: 12850501.18. Amasheh M, Fromm A, Krug SM, Amasheh S, Andres S, Zeitz M, Fromm M, Schulzke JD. TNFalpha-induced and berberineantagonized tight junction barrier impairment via tyrosine kinase, Akt and NFkappaB signaling. J Cell Sci. 2010; 123:4145–4155. PMID: 21062898.19. Cui HS, Hayasaka S, Zhang XY, Hayasaka Y, Chi ZL, Zheng LS. Effect of berberine on barrier function in a human retinal pigment epithelial cell line. Jpn J Ophthalmol. 2007; 51:64–67. PMID: 17295145.
Article20. Ma X, Jiang Y, Wu A, Chen X, Pi R, Liu M, Liu Y. Berberine attenuates experimental autoimmune encephalomyelitis in C57 BL/6 mice. PLoS One. 2010; 5:e13489. PMID: 20976070.
Article21. Cario E. Bacterial interactions with cells of the intestinal mucosa: Toll-like receptors and NOD2. Gut. 2005; 54:1182–1193. PMID: 15840688.
Article22. Williams DL, Ha T, Li C, Kalbfleisch JH, Ferguson DA Jr. Early activation of hepatic NFkappaB and NF-IL6 in polymicrobial sepsis correlates with bacteremia, cytokine expression, and mortality. Ann Surg. 1999; 230:95–104. PMID: 10400042.23. Otero-Antón E, González-Quintela A, López-Soto A, López-Ben S, Llovo J, Pérez LF. Cecal ligation and puncture as a model of sepsis in the rat: influence of the puncture size on mortality, bacteremia, endotoxemia and tumor necrosis factor alpha levels. Eur Surg Res. 2001; 33:77–79. PMID: 11399872.
Article24. Li GX, Wang XM, Jiang T, Gong JF, Niu LY, Li N. Berberine prevents damage to the intestinal mucosal barrier during early phase of sepsis in rat through mechanisms independent of the NOD-like receptors signaling pathway. Eur J Pharmacol. 2014; 730:1–7. PMID: 24530556.
Article25. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001; 25:402–408. PMID: 11846609.26. Takeuchi O, Hoshino K, Kawai T, Sanjo H, Takada H, Ogawa T, Takeda K, Akira S. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity. 1999; 11:443–451. PMID: 10549626.
Article27. Ozinsky A, Underhill DM, Fontenot JD, Hajjar AM, Smith KD, Wilson CB, Schroeder L, Aderem A. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc Natl Acad Sci U S A. 2000; 97:13766–13771. PMID: 11095740.
Article28. Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998; 282:2085–2088. PMID: 9851930.29. Ivory CP, Prystajecky M, Jobin C, Chadee K. Toll-like receptor 9-dependent macrophage activation by Entamoeba histolytica DNA. Infect Immun. 2008; 76:289–297. PMID: 17984204.30. Shang L, Fukata M, Thirunarayanan N, Martin AP, Arnaboldi P, Maussang D, Berin C, Unkeless JC, Mayer L, Abreu MT, Lira SA. Toll-like receptor signaling in small intestinal epithelium promotes B-cell recruitment and IgA production in lamina propria. Gastroenterology. 2008; 135:529–538. PMID: 18522803.
Article31. Gribar SC, Sodhi CP, Richardson WM, Anand RJ, Gittes GK, Branca MF, Jakub A, Shi XH, Shah S, Ozolek JA, Hackam DJ. Reciprocal expression and signaling of TLR4 and TLR9 in the pathogenesis and treatment of necrotizing enterocolitis. J Immunol. 2009; 182:636–646. PMID: 19109197.
Article32. Ghosh S, May MJ, Kopp EB. NF-kappa B and Rel proteins: evolutionarily conserved mediators of immune responses. Annu Rev Immunol. 1998; 16:225–260. PMID: 9597130.33. Wu CF, Bi XL, Yang JY, Zhan JY, Dong YX, Wang JH, Wang JM, Zhang R, Li X. Differential effects of ginsenosides on NO and TNF-alpha production by LPS-activated N9 microglia. Int Immunopharmacol. 2007; 7:313–320. PMID: 17276889.34. Yu M, Shao D, Feng X, Duan M, Xu J. Effects of ketamine on pulmonary TLR4 expression and NF-kappa-B activation during endotoxemia in rats. Methods Find Exp Clin Pharmacol. 2007; 29:395–399. PMID: 17922067.35. Liu H, Li M, Wang P, Wang F. Blockade of hypoxia-inducible factor-1α by YC-1 attenuates interferon-γ and tumor necrosis factor-α-induced intestinal epithelial barrier dysfunction. Cytokine. 2011; 56:581–588. PMID: 21890376.
Article36. Costantini TW, Loomis WH, Putnam JG, Drusinsky D, Deree J, Choi S, Wolf P, Baird A, Eliceiri B, Bansal V, Coimbra R. Burn-induced gut barrier injury is attenuated by phosphodiesterase inhibition: effects on tight junction structural proteins. Shock. 2009; 31:416–422. PMID: 18791495.37. Costantini TW, Deree J, Loomis W, Putnam JG, Choi S, Baird A, Eliceiri BP, Bansal V, Coimbra R. Phosphodiesterase inhibition attenuates alterations to the tight junction proteins occludin and ZO-1 in immunostimulated Caco-2 intestinal monolayers. Life Sci. 2009; 84:18–22. PMID: 18992758.
Article38. Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008; 57:712–717. PMID: 18442638.
Article39. National Toxicology Program. Toxicology and carcinogenesis studies of goldenseal root powder (Hydrastis Canadensis) in F344/N rats and B6C3F1 mice (feed studies). Natl Toxicol Program Tech Rep Ser. 2010; (562):1–188.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nucleic Acid Recognition and Signaling by Toll-like Receptor 9: Compartment-dependent Regulation
- Sepsis induces variation of intestinal barrier function in different phase through nuclear factor kappa B signaling
- TLR/MyD88-mediated Innate Immunity in Intestinal Graft-versus-Host Disease
- Lipopolysaccharide: Basic Biochemistry, Intracellular Signaling, and Physiological Impacts in the Gut
- The inhibition of inflammatory molecule expression on 3T3-L1 adipocytes by berberine is not mediated by leptin signaling