Korean J Physiol Pharmacol.
2010 Oct;14(5):257-263. 10.4196/kjpp.2010.14.5.257.
Neuroprotective Effect of Visnagin on Kainic Acid-induced Neuronal Cell Death in the Mice Hippocampus
- Affiliations
-
- 1Department of Pharmacology, Institute of Natural Medicine, College of Medicine, Hallym University, Chuncheon 200-702, Korea. hwsuh@hallym.ac.kr
- 2Department of Aerospace Medical Research, Aerospace Medical Center, ROKAF (Republic of Korea Air Force), Cheongwon 363-842, Korea.
- 3Department of Anatomy and Neurobiology, and Institute of Neurodegeneration and Neuroregeneration, College of Medicine, Hallym University, Chuncheon 200-702, Korea.
- KMID: 2071691
- DOI: http://doi.org/10.4196/kjpp.2010.14.5.257
Abstract
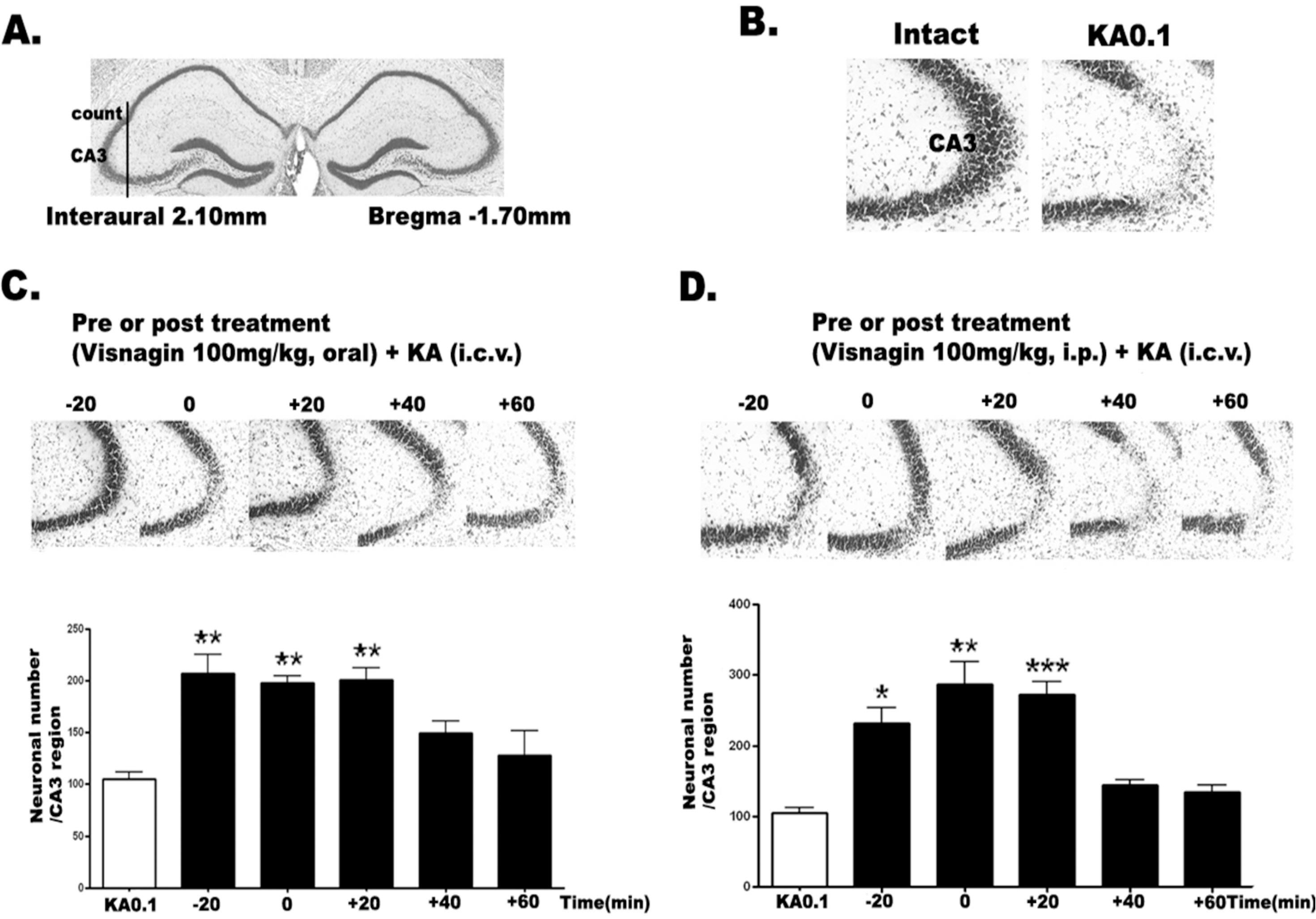
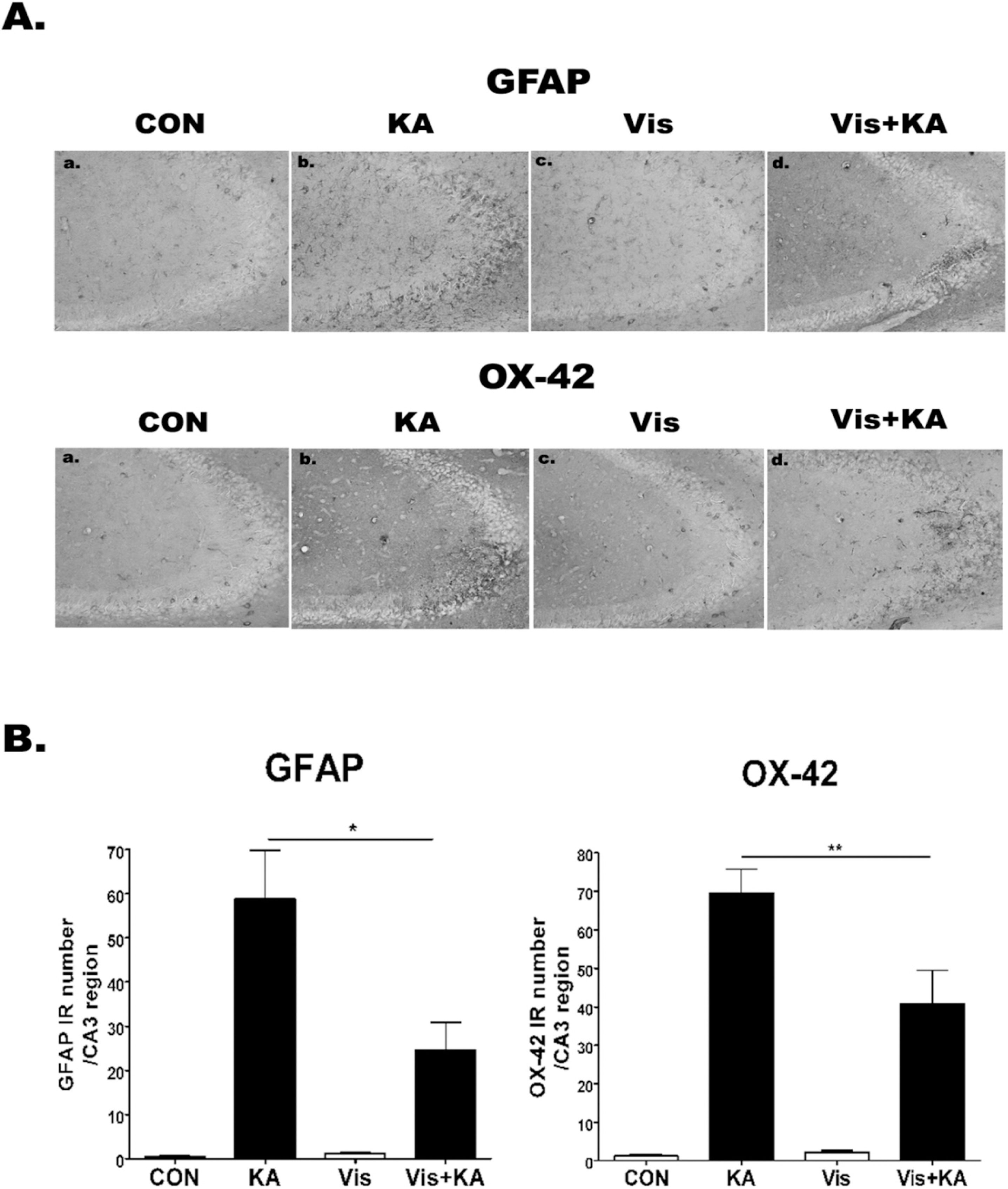
- Visnagin (4-methoxy-7-methyl-5H-furo[3,2-g][1]-benzopyran-5-one), which is an active principle extracted from the fruits of Ammi visnaga, has been used as a treatment for low blood-pressure and blocked blood vessel contraction by inhibition of calcium influx into blood cells. However, the neuroprotective effect of visnagin was not clearly known until now. Thus, we investigated whether visnagin has a neuroprotective effect against kainic acid (KA)-induced neuronal cell death. In the cresyl violet staining, pre-treatment or post-treatment visnagin (100 mg/kg, p.o. or i.p.) showed a neuroprotective effect on KA (0.1 microgram) toxicity. KA-induced gliosis and proinflammatory marker (IL-1beta, TNF-alpha, IL-6, and COX-2) inductions were also suppressed by visnagin administration. These results suggest that visnagin has a neuroprotective effect in terms of suppressing KA-induced pathogenesis in the brain, and that these neuroprotective effects are associated with its anti-inflammatory effects.
Keyword
MeSH Terms
-
Ammi
Animals
Benzoxazines
Blood Cells
Blood Vessels
Brain
Calcium
Cell Death
Contracts
Cytokines
Fruit
Gliosis
Glycosaminoglycans
Hippocampus
Interleukin-6
Kainic Acid
Khellin
Mice
Neurons
Neuroprotective Agents
Tumor Necrosis Factor-alpha
Viola
Benzoxazines
Calcium
Cytokines
Glycosaminoglycans
Interleukin-6
Kainic Acid
Khellin
Neuroprotective Agents
Tumor Necrosis Factor-alpha
Figure
Reference
-
References
1. Sperk G. Kainic acid seizures in the rat. Prog Neurobiol. 1994; 42:1–32.
Article2. Beal MF. Mechanisms of excitotoxicity in neurologic diseases. Faseb J. 1992; 6:3338–3344.
Article3. Rothman SM, Olney JW. Glutamate and the pathophysiology of hypoxic–ischemic brain damage. Ann Neurol. 1986; 19:105–111.
Article4. Jin Y, Lim CM, Kim SW, Park JY, Seo JS, Han PL, Yoon SH, Lee JK. Fluoxetine attenuates kainic acid-induced neuronal cell death in the mouse hippocampus. Brain Research. 2009; 1281:108–116.
Article5. Penkowa M, Florit S, Giralt M, Quintana A, Molinero A, Carrasco J, Hidalgo J. Metallothionein reduces central nervous system inflammation, neurodegeneration, and cell death following kainic acid-induced epileptic seizures. J Neurosci Res. 2005; 79:522–534.
Article6. Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996; 19:312–318.
Article7. Ridet JL, Malhotra SK, Privat A, Gage FH. Reactive astrocytes: cellular and molecular cues to biological function. Trends Neurosci. 1997; 20:570–577.
Article8. Kim JB, Yu YM, Kim SW, Lee JK. Anti-inflammatory mechanism is involved in ethyl pyruvate-mediated efficacious neuroprotection in the postischemic brain. Brain Research. 2005; 1060:188–192.
Article9. Smith E, Pucci LA, Bywater WG. Crystalline Visnagan. Science. 1952; 115:520–521.
Article10. Anrep GV, Barsoum GS, Kenawy MR, Misrahy G. Ammi Visnaga in the treatment of the anginal syndrome. Br Heart J. 1946; 8:171–177.
Article11. Anrep GV, Barsoum GS, Kenawy MR. The pharmacological actions of the crystalline principles of Ammi Visnaga Linn. J Pharm Pharmacol. 1949; 1:164–176.
Article12. Duarte J, Perez-Vizcaino F, Torres AI, Zarzuelo A, Jimenez J, Tamargo J. Vasodilator effects of visnagin in isolated rat vascular smooth muscle. Eur J Pharmacol. 1995; 286:115–122.
Article13. Rauwald HW, Brehm O, Odenthal KP. The involvement of a Ca2+ channel blocking mode of action in the pharmacology of Ammi visnaga fruits. Planta Medica. 1994; 60:101–105.14. Ubeda A, Tejerina T, Tamargo J, Villar A. Effects of khellin on contractile responses and 45Ca2+ movements in rat isolated aorta. J Pharm Pharmacol. 1991; 43:46–48.15. Duarte J, Torres AI, Zarzuelo A. Cardiovascular effects of visnagin on rats. Planta Medica. 2000; 66:35–39.16. Laursen SE, Belknap JK. Intracerebroventricular injections in mice. Some methodological refinements. J Pharmacol Methods. 1986; 16:355–357.17. Sapolsky RM, Krey LC, McEwen BS. Prolonged glucocorticoid exposure reduces hippocampal neuron number: implications for aging. J Neurosci. 1985; 5:1222–1227.
Article18. Franklin KBJ, Paxinos G. The mouse brain in stereotaxic coordinates. 3rd ed.San Diego: Academic Press;1997.19. Kwon MS, Seo YJ, Choi SM, Choi HW, Jung JS, Park SH, Suh HW. The differential effects of single or repeated restraint stress on kainic acid-induced neuronal death in the hippocampal CA3 region: the role of glucocorticoid and various signal molecules. J Neurochem. 2007; 103:1530–1541.
Article20. Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987; 162:156–159.
Article21. Kim SW, Yu YM, Piao CS, Kim JB, Lee JK. Inhibition of delayed induction of p38 mitogen-activated protein kinase attenuates kainic acid-induced neuronal loss in the hippocampus. Brain Research. 2004; 1007:188–191.
Article22. Weiss JH, Sensi SL, Koh JY. Zn(2+): a novel ionic mediator of neural injury in brain disease. Trends Pharmacol Sci. 2000; 21:395–401.23. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007; 87:873–904.
Article24. White BC, Sullivan JM, DeGracia DJ, O'Neil BJ, Neumar RW, Grossman LI, Rafols JA, Krause GS. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci. 2000; 179:1–33.
Article25. Hudson J, Towers GHN. Phytomedicines as antivirals. Drugs Future. 1999; 24:295–300.
Article26. Cho IH, Kim SW, Kim JB, Kim TK, Lee KW, Han PL, Lee JK. Ethyl pyruvate attenuates kainic acid-induced neuronal cell death in the mouse hippocampus. J Neurosci Res. 2006; 84:1505–1511.
Article27. Yoo KY, Hwang IK, Kim JD, Kang IJ, Park J, Yi JS, Kim JK, Bae YS, Won MH. Antiinflammatory effect of the ethanol extract of Berberis koreana in a gerbil model of cerebral ischemia/reperfusion. Phytother Res. 2008; 22:1527–1532.28. Beattie EC, Stellwagen D, Morishita W, Bresnahan JC, Ha BK, Von Zastrow M, Beattie MS, Malenka RC. Control of synaptic strength by glial TNFalpha. Science. 2002; 295:2282–2285.29. Stellwagen D, Beattie EC, Seo JY, Malenka RC. Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J Neurosci. 2005; 25:3219–3228.30. Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M. Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci. 2003; 23:8692–8700.31. Wang S, Cheng Q, Malik S, Yang J. Interleukin-1beta inhibits gamma-aminobutyric acid type A (GABA(A)) receptor current in cultured hippocampal neurons. J Pharmacol Exp Ther. 2000; 292:497–504.32. McGeer PL, Schulzer M, McGeer EG. Arthritis and anti-inflammatory agents as possible protective factors for Alzheimer's disease: a review of 17 epidemiologic studies. Neurology. 1996; 47:425–432.33. Nogawa S, Zhang F, Ross ME, Iadecola C. Cyclo-oxygenase-2 gene expression in neurons contributes to ischemic brain damage. J Neurosci. 1997; 17:2746–2755.
Article34. Nakayama M, Uchimura K, Zhu RL, Nagayama T, Rose ME, Stetler RA, Isakson PC, Chen J, Graham SH. Cyclooxygenase-2 inhibition prevents delayed death of CA1 hippocampal neurons following global ischemia. Proc Natl Acad Sci U S A. 1998; 95:10954–10959.
Article35. Coyle JT, Puttfarcken P. Oxidative stress, glutamate, and neurodegenerative disorders. Science. 1993; 262:689–695.
Article36. Funk CD. Prostaglandins and leukotrienes: advances in eicosanoid biology. Science. 2001; 294:1871–1875.
Article37. Aboul-Enein HY, Kladna A, Kruk I, Lichszteld K, Michalska T. Effect of psoralens on Fenton-like reaction generating reactive oxygen species. Biopolymers. 2003; 72:59–68.
Article38. Buttini M, Appel K, Sauter A, Gebicke-Haerter PJ, Boddeke HW. Expression of tumor necrosis factor alpha after focal cerebral ischaemia in the rat. Neuroscience. 1996; 71:1–16.
Article39. Chao CC, Hu S, Molitor TW, Shaskan EG, Peterson PK. Activated microglia mediate neuronal cell injury via a nitric oxide mechanism. J Immunol. 1992; 149:2736–2741.40. Barger SW, Basile AS. Activation of microglia by secreted amyloid precursor protein evokes release of glutamate by cystine exchange and attenuates synaptic function. J Neurochem. 2001; 76:846–854.
Article41. Piani D, Spranger M, Frei K, Schaffner A, Fontana A. Macrophage-induced cytotoxicity of N-methyl-D-aspartate receptor positive neurons involves excitatory amino acids rather than reactive oxygen intermediates and cytokines. Eur J Immunol. 1992; 22:2429–2436.
Article42. Liang J, Takeuchi H, Doi Y, Kawanokuchi J, Sonobe Y, Jin S, Yawata I, Li H, Yasuoka S, Mizuno T, Suzumura A. Excitatory amino acid transporter expression by astrocytes is neuroprotective against microglial excitotoxicity. Brain Research. 2008; 1210:11–19.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Protective Effect of Etomidate on Kainic Acid-induced Neurotoxicity in Rat Hippocampus
- Kainic Acid Treatment Increases Ca²âº-mediated Neurotoxicity in the Mouse Hippocampus
- Glycyrrhizin Attenuates Kainic Acid-Induced Neuronal Cell Death in the Mouse Hippocampus
- Cilostazol attenuates kainic acid-induced hippocampal cell death
- Effect of Pioglitazone on Excitotoxic Neuronal Damage in the Mouse Hippocampus