Korean J Physiol Pharmacol.
2017 May;21(3):317-325. 10.4196/kjpp.2017.21.3.317.
Endogenous catalase delays high-fat diet-induced liver injury in mice
- Affiliations
-
- 1Graduate School of Pharmaceutical Sciences, College of Pharmacy, Ewha Womans University, Seoul 03760, Korea. hha@ewha.ac.kr
- KMID: 2376960
- DOI: http://doi.org/10.4196/kjpp.2017.21.3.317
Abstract
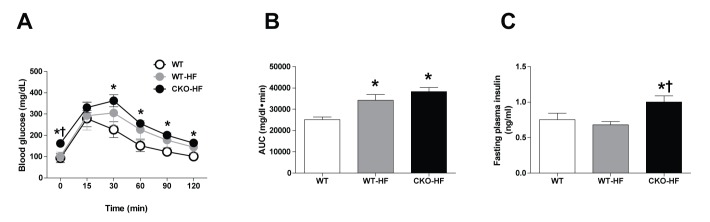
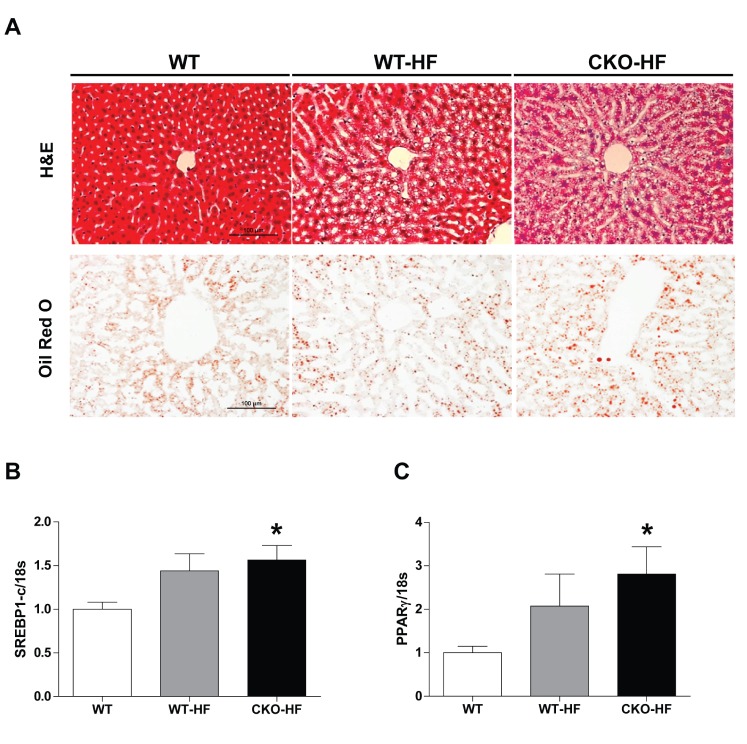
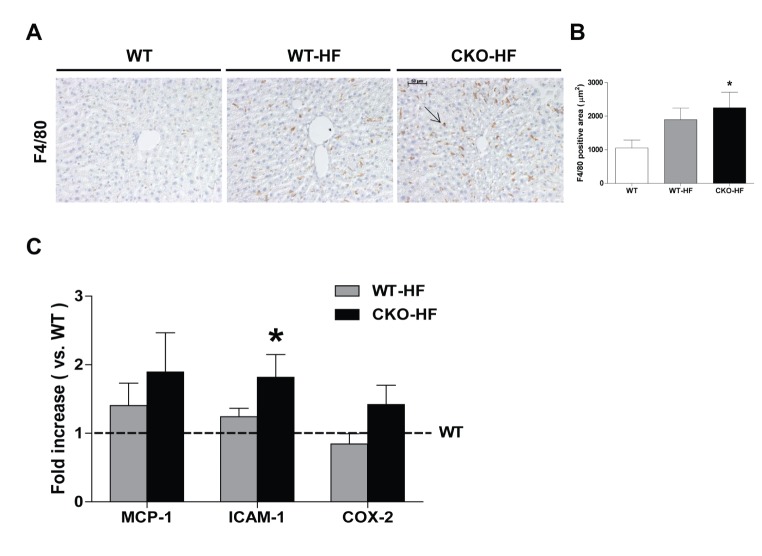
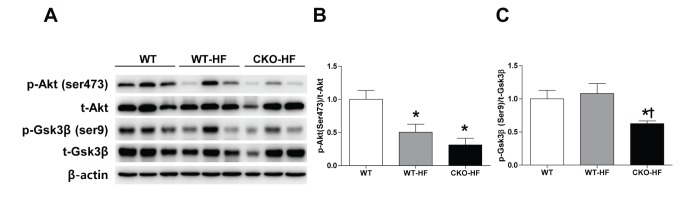
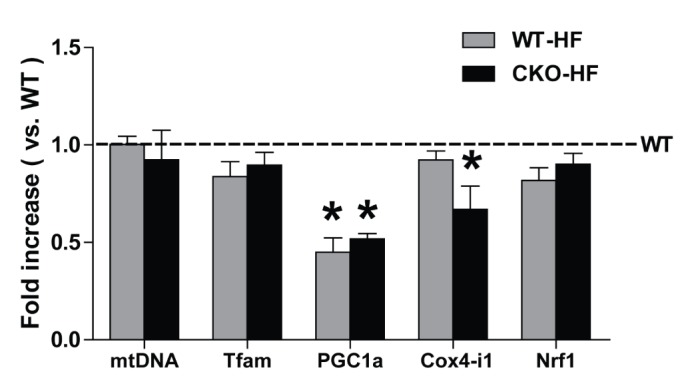
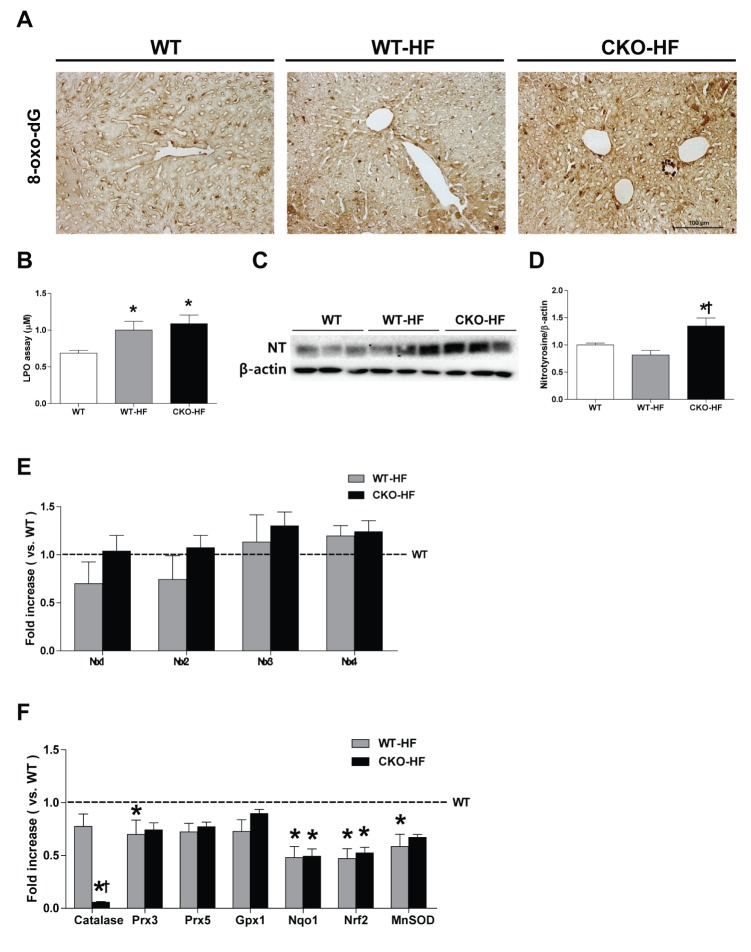
- Non-alcoholic fatty liver disease (NAFLD) has become the most prevalent liver disease in parallel with worldwide epidemic of obesity. Reactive oxygen species (ROS) contributes to the development and progression of NAFLD. Peroxisomes play an important role in fatty acid oxidation and ROS homeostasis, and catalase is an antioxidant exclusively expressed in peroxisome. The present study examined the role of endogenous catalase in early stage of NAFLD. 8-week-old male catalase knock-out (CKO) and age-matched C57BL/6J wild type (WT) mice were fed either a normal diet (ND: 18% of total calories from fat) or a high fat diet (HFD: 60% of total calories from fat) for 2 weeks. CKO mice gained body weight faster than WT mice at early period of HFD feeding. Plasma triglyceride and ALT, fasting plasma insulin, as well as liver lipid accumulation, inflammation (F4/80 staining), and oxidative stress (8-oxo-dG staining and nitrotyrosine level) were significantly increased in CKO but not in WT mice at 2 weeks of HFD feeding. While phosphorylation of Akt (Ser473) and PGC1α mRNA expression were decreased in both CKO and WT mice at HFD feeding, GSK3β phosphorylation and Cox4-il mRNA expression in the liver were decreased only in CKO-HF mice. Taken together, the present data demonstrated that endogenous catalase exerted beneficial effects in protecting liver injury including lipid accumulation and inflammation through maintaining liver redox balance from the early stage of HFD-induced metabolic stress.
Keyword
MeSH Terms
-
Animals
Body Weight
Catalase*
Diet
Diet, High-Fat
Fasting
Homeostasis
Humans
Inflammation
Insulin
Insulin Resistance
Liver Diseases
Liver*
Male
Mice*
Non-alcoholic Fatty Liver Disease
Obesity
Oxidation-Reduction
Oxidative Stress
Peroxisomes
Phosphorylation
Plasma
Reactive Oxygen Species
RNA, Messenger
Stress, Physiological
Triglycerides
Catalase
Insulin
RNA, Messenger
Reactive Oxygen Species
Figure
Cited by 1 articles
-
Peroxisomal Fitness: A Potential Protective Mechanism of Fenofibrate against High Fat Diet-Induced Non-Alcoholic Fatty Liver Disease in Mice
Songling Jiang, Md Jamal Uddin, Xiaoying Yu, Lingjuan Piao, Debra Dorotea, Goo Taeg Oh, Hunjoo Ha
Diabetes Metab J. 2022;46(6):829-842. doi: 10.4093/dmj.2021.0274.
Reference
-
1. Suzuki A, Angulo P, Lymp J, St Sauver J, Muto A, Okada T, Lindor K. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology. 2005; 41:64–71. PMID: 15690483.
Article2. Hamaguchi M, Kojima T, Takeda N, Nakagawa T, Taniguchi H, Fujii K, Omatsu T, Nakajima T, Sarui H, Shimazaki M, Kato T, Okuda J, Ida K. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med. 2005; 143:722–728. PMID: 16287793.
Article3. Basaranoglu M, Basaranoglu G, Sentürk H. From fatty liver to fibrosis: a tale of “second hit”. World J Gastroenterol. 2013; 19:1158–1165. PMID: 23483818.
Article4. Matsuzawa-Nagata N, Takamura T, Ando H, Nakamura S, Kurita S, Misu H, Ota T, Yokoyama M, Honda M, Miyamoto K, Kaneko S. Increased oxidative stress precedes the onset of high-fat diet-induced insulin resistance and obesity. Metabolism. 2008; 57:1071–1077. PMID: 18640384.
Article5. Diehl AM. Lessons from animal models of NASH. Hepatol Res. 2005; 33:138–144. PMID: 16198624.
Article6. Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004; 114:1752–1761. PMID: 15599400.
Article7. Podrini C, Borghesan M, Greco A, Pazienza V, Mazzoccoli G, Vinciguerra M. Redox homeostasis and epigenetics in non-alcoholic fatty liver disease (NAFLD). Curr Pharm Des. 2013; 19:2737–2746. PMID: 23092327.
Article8. Touyz RM, Briones AM. Reactive oxygen species and vascular biology: implications in human hypertension. Hypertens Res. 2011; 34:5–14. PMID: 20981034.
Article9. Knebel B, Hartwig S, Haas J, Lehr S, Goeddeke S, Susanto F, Bohne L, Jacob S, Koellmer C, Nitzgen U, Müller-Wieland D, Kotzka J. Peroxisomes compensate hepatic lipid overflow in mice with fatty liver. Biochim Biophys Acta. 2015; 1851:965–976. PMID: 25790917.
Article10. Park HS, Jang JE, Ko MS, Woo SH, Kim BJ, Kim HS, Park HS, Park IS, Koh EH, Lee KU. Statins increase mitochondrial and peroxisomal fatty acid oxidation in the liver and prevent non-alcoholic steatohepatitis in mice. Diabetes Metab J. 2016; 40:376–385. PMID: 27098507.
Article11. Wei Y, Rector RS, Thyfault JP, Ibdah JA. Nonalcoholic fatty liver disease and mitochondrial dysfunction. World J Gastroenterol. 2008; 14:193–199. PMID: 18186554.
Article12. Van Veldhoven PP, Vanhove G, Assselberghs S, Eyssen HJ, Mannaerts GP. Substrate specificities of rat liver peroxisomal acyl-CoA oxidases: palmitoyl-CoA oxidase (inducible acyl-CoA oxidase), pristanoyl-CoA oxidase (non-inducible acyl-CoA oxidase), and trihydroxycoprostanoyl-CoA oxidase. J Biol Chem. 1992; 267:20065–20074. PMID: 1400324.
Article13. Fransen M, Nordgren M, Wang B, Apanasets O. Role of peroxisomes in ROS/RNS-metabolism: implications for human disease. Biochim Biophys Acta. 2012; 1822:1363–1373. PMID: 22178243.
Article14. Lismont C, Nordgren M, Van Veldhoven PP, Fransen M. Redox interplay between mitochondria and peroxisomes. Front Cell Dev Biol. 2015; 3:35. PMID: 26075204.
Article15. Antonenkov VD, Grunau S, Ohlmeier S, Hiltunen JK. Peroxisomes are oxidative organelles. Antioxid Redox Signal. 2010; 13:525–537. PMID: 19958170.
Article16. Okuno Y, Matsuda M, Kobayashi H, Morita K, Suzuki E, Fukuhara A, Komuro R, Shimabukuro M, Shimomura I. Adipose expression of catalase is regulated via a novel remote PPARgamma-responsive region. Biochem Biophys Res Commun. 2008; 366:698–704. PMID: 18073138.17. Hwang I, Lee J, Huh JY, Park J, Lee HB, Ho YS, Ha H. Catalase deficiency accelerates diabetic renal injury through peroxisomal dysfunction. Diabetes. 2012; 61:728–738. PMID: 22315314.
Article18. Flamment M, Rieusset J, Vidal H, Simard G, Malthièry Y, Fromenty B, Ducluzeau PH. Regulation of hepatic mitochondrial metabolism in response to a high fat diet: a longitudinal study in rats. J Physiol Biochem. 2012; 68:335–344. PMID: 22278845.
Article19. Ho YS, Xiong Y, Ma W, Spector A, Ho DS. Mice lacking catalase develop normally but show differential sensitivity to oxidant tissue injury. J Biol Chem. 2004; 279:32804–32812. PMID: 15178682.
Article20. Stienstra R, Mandard S, Patsouris D, Maass C, Kersten S, Müller M. Peroxisome proliferator-activated receptor alpha protects against obesity-induced hepatic inflammation. Endocrinology. 2007; 148:2753–2763. PMID: 17347305.21. Lee YS, Li P, Huh JY, Hwang IJ, Lu M, Kim JI, Ham M, Talukdar S, Chen A, Lu WJ, Bandyopadhyay GK, Schwendener R, Olefsky J, Kim JB. Inflammation is necessary for long-term but not short-term high-fat diet-induced insulin resistance. Diabetes. 2011; 60:2474–2483. PMID: 21911747.
Article22. Lanthier N, Molendi-Coste O, Horsmans Y, van Rooijen N, Cani PD, Leclercq IA. Kupffer cell activation is a causal factor for hepatic insulin resistance. Am J Physiol Gastrointest Liver Physiol. 2010; 298:G107–G116. PMID: 19875703.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lycopene supplementation suppresses oxidative stress induced by a high fat diet in gerbils
- Effect of Dietary Grape Pomace on Lipid Oxidation and Related Enzyme Activities in Rats Fed High Fat Diet
- The effects of Angelica keiskei Koidz on the expression of antioxidant enzymes related to lipid profiles in rats fed a high fat diet
- Integrative Omics Reveals Metabolic and Transcriptomic Alteration of Nonalcoholic Fatty Liver Disease in Catalase Knockout Mice
- Effect of Dietary Fat and Genistein on Lipid Metabolism and Antioxidant Activity in Hyperlipidemic Male Rats induced High Fat Diet