J Gynecol Oncol.
2015 Jan;26(1):40-45. 10.3802/jgo.2015.26.1.40.
DNA mismatch repair-related protein loss as a prognostic factor in endometrial cancers
- Affiliations
-
- 1Department of Obstetrics and Gynecology, National Defense Medical College Hospital, Tokorozawa, Japan. mastkn@ndmc.ac.jp
- 2Department of Basic Pathology, National Defense Medical College Hospital, Tokorozawa, Japan.
- KMID: 2158801
- DOI: http://doi.org/10.3802/jgo.2015.26.1.40
Abstract
OBJECTIVE
Recent investigations have revealed DNA mismatch repair (MMR) gene mutations are closely related with carcinogenesis of endometrial cancer; however the impact of MMR protein expression on prognosis is not determined. Correlations between MMR-related protein expression and clinicopathological factors of endometrial cancers are analyzed in the present study.
METHODS
A total of 191 endometrial cancer tissues treated between 1990 and 2007 in our hospital were enrolled. Immunoreactions for MSH2, MLH1, MSH6, and PMS2 on tissue microarray specimens and clinicopathological features were analyzed retrospectively.
RESULTS
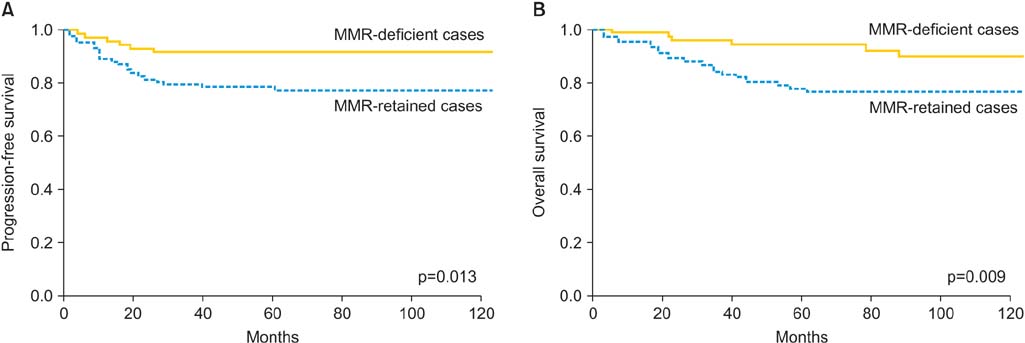
Seventy-six cases (40%) had at least one immunohistochemical alteration in MMR proteins (MMR-deficient group). There were statistically significant differences of histology, International Federation of Gynecology and Obstetrics (FIGO) stage, and histological grade between MMR-deficient group and the other cases (MMR-retained group). Response rate of first-line chemotherapy in evaluable cases was slightly higher in MMR-deficient cases (67% vs. 44%, p=0.34). MMR-deficient cases had significantly better progression-free and overall survival (OS) compared with MMR-retained cases. Multivariate analysis revealed MMR status was an independent prognostic factor for OS in endometrial cancers.
CONCLUSION
MMR-related proteins expression was identified as an independent prognostic factor for OS, suggesting that MMR was a key biomarker for further investigations of endometrial cancers.
Keyword
MeSH Terms
-
Adaptor Proteins, Signal Transducing/deficiency/metabolism
Adenosine Triphosphatases/deficiency/metabolism
Adult
Aged
Aged, 80 and over
Chemotherapy, Adjuvant
*DNA Mismatch Repair
DNA Repair Enzymes/deficiency/*metabolism
DNA-Binding Proteins/deficiency/*metabolism
Endometrial Neoplasms/*diagnosis/drug therapy/genetics/pathology
Female
Humans
Kaplan-Meier Estimate
Middle Aged
MutS Homolog 2 Protein/deficiency/metabolism
Neoplasm Proteins/deficiency/metabolism
Nuclear Proteins/deficiency/metabolism
Prognosis
Retrospective Studies
Tumor Markers, Biological/*metabolism
Adaptor Proteins, Signal Transducing
Adenosine Triphosphatases
DNA-Binding Proteins
DNA Repair Enzymes
MutS Homolog 2 Protein
Neoplasm Proteins
Nuclear Proteins
Tumor Markers, Biological
Figure
Cited by 2 articles
-
Endometrial cancer risk and survival by tumor MMR status
Christina M. Nagle, Tracy A. O'Mara, Yen Tan, Daniel D. Buchanan, Andreas Obermair, Penny Blomfield, Michael A. Quinn, Penelope M. Webb, Amanda B. Spurdle,
J Gynecol Oncol. 2018;29(3):. doi: 10.3802/jgo.2018.29.e39.Trends of uterine cancer incidence: a projection from the past to the future
Siriwan Tangjitgamol
J Gynecol Oncol. 2019;30(2):. doi: 10.3802/jgo.2019.30.e36.
Reference
-
1. Matsuda A, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H, et al. Cancer incidence and incidence rates in Japan in 2007: a study of 21 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2013; 43:328–336.2. Hirai Y, Banno K, Suzuki M, Ichikawa Y, Udagawa Y, Sugano K, et al. Molecular epidemiological and mutational analysis of DNA mismatch repair (MMR) genes in endometrial cancer patients with HNPCC-associated familial predisposition to cancer. Cancer Sci. 2008; 99:1715–1719.3. OECDiLibrary. Health at a glance [Internet]. Paris: OECD;2013. cited 2014 Sep 9. Available from: http://dx.doi.org/10.1787/health_glance-2013-en.4. Japanese Gynecologic Oncology Committee. Annual report of endometrial carcinoma patients in 2006. Acta Obstet Gynaecol Jpn. 2008; 60:1034–1040.5. Brinton LA, Felix AS, McMeekin DS, Creasman WT, Sherman ME, Mutch D, et al. Etiologic heterogeneity in endometrial cancer: evidence from a Gynecologic Oncology Group trial. Gynecol Oncol. 2013; 129:277–284.6. Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, Xiang YB, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013; 31:2607–2618.7. Karamurzin Y, Rutgers JK. DNA mismatch repair deficiency in endometrial carcinoma. Int J Gynecol Pathol. 2009; 28:239–255.8. Garg K, Soslow RA. Lynch syndrome (hereditary non-polyposis colorectal cancer) and endometrial carcinoma. J Clin Pathol. 2009; 62:679–684.9. Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JP, et al. Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci U S A. 1998; 95:6870–6875.10. Boland CR, Koi M, Chang DK, Carethers JM. The biochemical basis of microsatellite instability and abnormal immunohistochemistry and clinical behavior in Lynch syndrome: from bench to bedside. Fam Cancer. 2008; 7:41–52.11. Thibodeau SN, Bren G, Schaid D. Microsatellite instability in cancer of the proximal colon. Science. 1993; 260:816–819.12. Hewish M, Lord CJ, Martin SA, Cunningham D, Ashworth A. Mismatch repair deficient colorectal cancer in the era of personalized treatment. Nat Rev Clin Oncol. 2010; 7:197–208.13. Vilar E, Scaltriti M, Balmana J, Saura C, Guzman M, Arribas J, et al. Microsatellite instability due to hMLH1 deficiency is associated with increased cytotoxicity to irinotecan in human colorectal cancer cell lines. Br J Cancer. 2008; 99:1607–1612.14. Damia G, D'Incalci M. Genetic instability influences drug response in cancer cells. Curr Drug Targets. 2010; 11:1317–1324.15. Benatti P, Gafa R, Barana D, Marino M, Scarselli A, Pedroni M, et al. Microsatellite instability and colorectal cancer prognosis. Clin Cancer Res. 2005; 11:8332–8340.16. Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French AJ, Goldberg RM, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003; 349:247–257.17. Fink D, Nebel S, Aebi S, Zheng H, Cenni B, Nehme A, et al. The role of DNA mismatch repair in platinum drug resistance. Cancer Res. 1996; 56:4881–4886.18. Lindor NM, Burgart LJ, Leontovich O, Goldberg RM, Cunningham JM, Sargent DJ, et al. Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J Clin Oncol. 2002; 20:1043–1048.19. Modica I, Soslow RA, Black D, Tornos C, Kauff N, Shia J. Utility of immunohistochemistry in predicting microsatellite instability in endometrial carcinoma. Am J Surg Pathol. 2007; 31:744–751.20. Garg K, Shih K, Barakat R, Zhou Q, Iasonos A, Soslow RA. Endometrial carcinomas in women aged 40 years and younger: tumors associated with loss of DNA mismatch repair proteins comprise a distinct clinicopathologic subset. Am J Surg Pathol. 2009; 33:1869–1877.21. Shih KK, Garg K, Levine DA, Kauff ND, Abu-Rustum NR, Soslow RA, et al. Clinicopathologic significance of DNA mismatch repair protein defects and endometrial cancer in women 40 years of age and younger. Gynecol Oncol. 2011; 123:88–94.22. Black D, Soslow RA, Levine DA, Tornos C, Chen SC, Hummer AJ, et al. Clinicopathologic significance of defective DNA mismatch repair in endometrial carcinoma. J Clin Oncol. 2006; 24:1745–1753.23. Zighelboim I, Goodfellow PJ, Gao F, Gibb RK, Powell MA, Rader JS, et al. Microsatellite instability and epigenetic inactivation of MLH1 and outcome of patients with endometrial carcinomas of the endometrioid type. J Clin Oncol. 2007; 25:2042–2048.24. Basil JB, Goodfellow PJ, Rader JS, Mutch DG, Herzog TJ. Clinical significance of microsatellite instability in endometrial carcinoma. Cancer. 2000; 89:1758–1764.25. Diaz-Padilla I, Romero N, Amir E, Matias-Guiu X, Vilar E, Muggia F, et al. Mismatch repair status and clinical outcome in endometrial cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2013; 88:154–167.26. Grzankowski KS, Shimizu DM, Kimata C, Black M, Terada KY. Clinical and pathologic features of young endometrial cancer patients with loss of mismatch repair expression. Gynecol Oncol. 2012; 126:408–412.27. Report of gynecologic oncology committee. Committee for frequency of hereditary endometrial cancer and its clinicopathology in Japan. Acta Obstet Gynaecol Jpn. 2009; 61:1540–1542.28. Resnick KE, Frankel WL, Morrison CD, Fowler JM, Copeland LJ, Stephens J, et al. Mismatch repair status and outcomes after adjuvant therapy in patients with surgically staged endometrial cancer. Gynecol Oncol. 2010; 117:234–238.29. Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, et al. Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 2006; 24:36–44.30. Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, et al. Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: a Japanese Gynecologic Oncology Group study. Gynecol Oncol. 2008; 108:226–233.31. Watanabe Y, Kitagawa R, Aoki D, Takeuchi S, Sagae S, Sakuragi N, et al. Practice pattern for postoperative management of endometrial cancer in Japan: a survey of the Japanese Gynecologic Oncology Group. Gynecol Oncol. 2009; 115:456–459.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Loss of ARID1A Expression in Gastric Cancer: Correlation with Mismatch Repair Deficiency and Clinicopathologic Features
- Hereditary Nonpolyposis Colorectal Cancer
- Clinical significance of mismatch repair genes immunohistochemical expression of complex endometrial hyperplasia
- One case of Lynch type II syndrome
- Identification of Target Genes in the Endometrial Carcinomas with Microsatellite Mutator Phenotype