World J Mens Health.
2019 May;37(2):210-218. 10.5534/wjmh.180057.
Comparison of Improving Effects for Diabetic Erectile Dysfunction according to the Anti-Glycemic Agents: Phlorizin and Insulin
- Affiliations
-
- 1Department of Urology, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Urology, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Department of Urology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. swkim@snu.ac.kr
- KMID: 2443236
- DOI: http://doi.org/10.5534/wjmh.180057
Abstract
- PURPOSE
To compare the improving effects of diabetic erectile dysfunction with two anti-glycemic agents; phlorizin and insulin.
MATERIALS AND METHODS
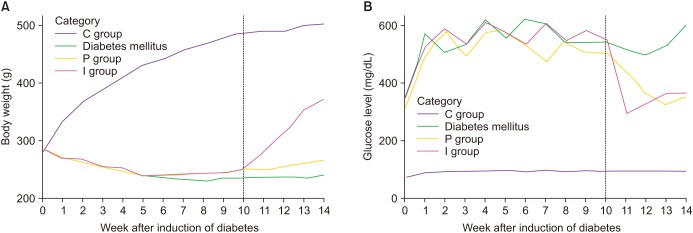
Sixty Sprague-Dawley rats were divided into four groups (n=15 in each group): normal control (C), untreated diabetic rats (D), and diabetic rats treated by phlorizin (P) or insulin (I). Ten weeks after the diabetic induction using an injection of streptozotocin (55 mg/kg), four weeks of diabetic control was conducted. Erectile response, Western blot, and immunohistochemistry were assessed.
RESULTS
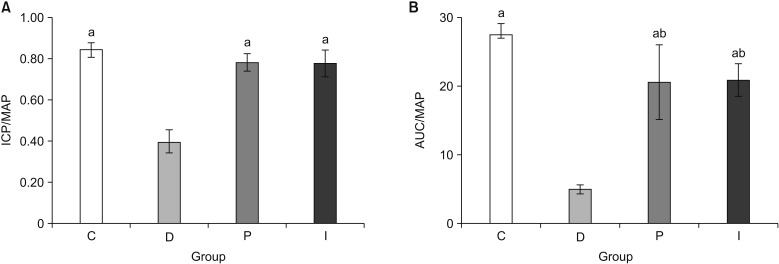
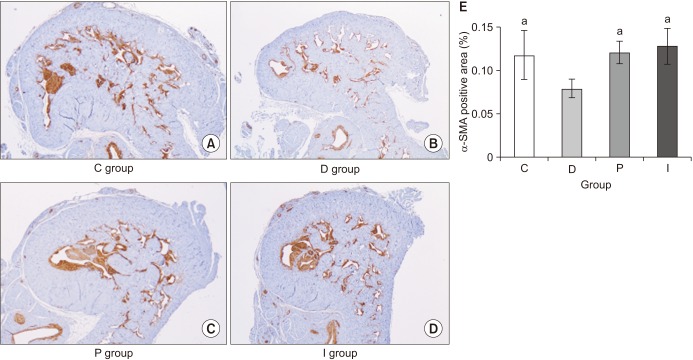
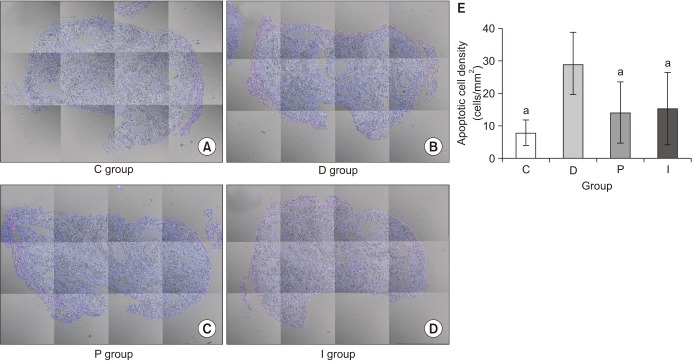
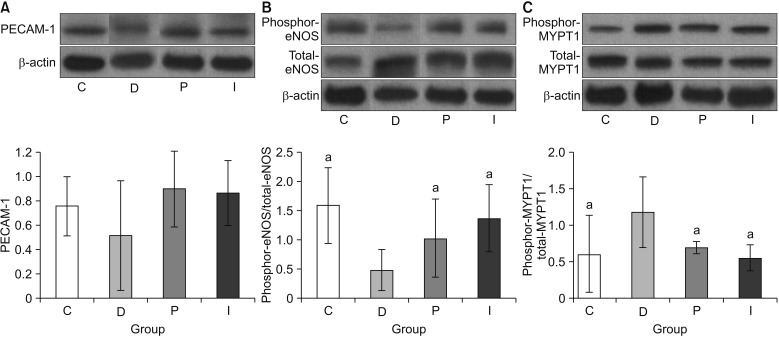
During the experiment, the C-group showed continuous weight gain, while the other groups suffered from weight loss. After start of diabetic control, the body weight of I-group was increased; whereas, there was no meaningful change in the P-group. Meanwhile, comparable blood glucose levels were achieved in the P- and I-groups. The erectile response was markedly decreased in the D-group, whereas the P- and I-groups were similar as good as the C-group. In addition, D-group showed the significant decrease in the cavernosal smooth muscle content and increased apoptosis. Platelet endothelial cell adhesion molecule-1 protein expression, phosphorylation of endothelial nitric oxide synthase and myosin phosphatase target subunit 1 were significantly distorted in the D-group, while the P- and I-groups were comparable with the C-group.
CONCLUSIONS
Phlorizin treatment resulted in the improvement of erectile function as same as insulin despite the lack of anabolic weight gains. These results suggest that control of blood glucose level rather than a type of anti-glycemic agents is more important for the prevention and treatment of diabetic erectile dysfunction
MeSH Terms
-
Animals
Antigens, CD31
Apoptosis
Blood Glucose
Blotting, Western
Body Weight
Diabetes Complications
Erectile Dysfunction*
Immunohistochemistry
Insulin*
Male
Muscle, Smooth
Myosin-Light-Chain Phosphatase
Nitric Oxide Synthase Type III
Phlorhizin*
Phosphorylation
Rats
Rats, Sprague-Dawley
Streptozocin
Weight Gain
Weight Loss
Antigens, CD31
Blood Glucose
Insulin
Myosin-Light-Chain Phosphatase
Nitric Oxide Synthase Type III
Phlorhizin
Streptozocin
Figure
Reference
-
1. Althof SE, Buvat J, Gutkin SW, Belger M, Stothard DR, Fugl-Meyer AR. Sexual satisfaction in men with erectile dysfunction: correlates and potential predictors. J Sex Med. 2010; 7:203–215. PMID: 19845846.
Article2. Moore CR, Wang R. Pathophysiology and treatment of diabetic erectile dysfunction. Asian J Androl. 2006; 8:675–684. PMID: 16892168.
Article3. Cho SY, Park K, Paick JS, Kim SW. Change of erectile function and responsiveness to phosphodiesterase type 5 inhibitors at different stages of streptozotocin-induced diabetes in rats. J Sex Med. 2011; 8:1352–1361. PMID: 21054802.
Article4. Cho SY, Chai JS, Lee SH, Park K, Paick JS, Kim SW. Investigation of the effects of the level of glycemic control on erectile function and pathophysiological mechanisms in diabetic rats. J Sex Med. 2012; 9:1550–1558. PMID: 22489802.
Article5. Castela Â, Costa C. Molecular mechanisms associated with diabetic endothelial-erectile dysfunction. Nat Rev Urol. 2016; 13:266–274. PMID: 26878803.
Article6. Park K, Cho SY, Kim SW. Erectile response to type 5 phosphodiesterase inhibitor could be preserved with the addition of simvastatin to conventional insulin treatment in rat model of diabetes. Int J Androl. 2011; 34:e468–e474. PMID: 21790657.
Article7. Choi WS, Kwon OS, Cho SY, Paick JS, Kim SW. Effect of chronic administration of PDE5 combined with glycemic control on erectile function in streptozotocin-induced diabetic rats. J Sex Med. 2015; 12:600–610. PMID: 25411013.
Article8. Wessells H, Penson DF, Cleary P, Rutledge BN, Lachin JM, McVary KT, et al. Effect of intensive glycemic therapy on erectile function in men with type 1 diabetes. J Urol. 2011; 185:1828–1834. PMID: 21420129.
Article9. McVary K. Lower urinary tract symptoms and sexual dysfunction: epidemiology and pathophysiology. BJU Int. 2006; 97(Suppl 2):23–28. discussion 44-5. PMID: 16507050.
Article10. González-Sánchez JL, Serrano-Ríos M. Molecular basis of insulin action. Drug News Perspect. 2007; 20:527–531. PMID: 18080040.
Article11. Wu G, Meininger CJ. Nitric oxide and vascular insulin resistance. Biofactors. 2009; 35:21–27. PMID: 19319842.
Article12. Rosenwasser RF, Sultan S, Sutton D, Choksi R, Epstein BJ. SGLT-2 inhibitors and their potential in the treatment of diabetes. Diabetes Metab Syndr Obes. 2013; 6:453–467. PMID: 24348059.13. Park J, Kwon OS, Cho SY, Paick JS, Kim SW. Chronic administration of atorvastatin could partially ameliorate erectile function in streptozotocin-induced diabetic rats. PLoS One. 2017; 12:e0172751. PMID: 28245261.
Article14. Freitas HS, D'Agord Schaan B, da Silva RS, Okamoto MM, Oliveira-Souza M, Machado UF. Insulin but not phlorizin treatment induces a transient increase in GLUT2 gene expression in the kidney of diabetic rats. Nephron Physiol. 2007; 105:p42–p51. PMID: 17204838.
Article15. Najafian M, Jahromi MZ, Nowroznejhad MJ, Khajeaian P, Kargar MM, Sadeghi M, et al. Phloridzin reduces blood glucose levels and improves lipids metabolism in streptozotoc-ininduced diabetic rats. Mol Biol Rep. 2012; 39:5299–5306. PMID: 22167331.
Article16. Li WJ, Park K, Paick JS, Kim SW. Chronic treatment with an oral rho-kinase inhibitor restores erectile function by suppressing corporal apoptosis in diabetic rats. J Sex Med. 2011; 8:400–410. PMID: 20233282.
Article17. Kamenov ZA. A comprehensive review of erectile dysfunction in men with diabetes. Exp Clin Endocrinol Diabetes. 2015; 123:141–158. PMID: 25502583.
Article18. Kubin M, Wagner G, Fugl-Meyer AR. Epidemiology of erectile dysfunction. Int J Impot Res. 2003; 15:63–71. PMID: 12605242.
Article19. Kang SY, Lee JA, Sunwoo S, Yu BY, Lee JH, Cho CH, et al. Prevalence of sexual dysfunction and associated risk factors in middle-aged and elderly Korean men in primary care. J Sex Res. 2016; 53:1165–1178. PMID: 27215144.
Article20. Miner M, Nehra A, Jackson G, Bhasin S, Billups K, Burnett AL, et al. All men with vasculogenic erectile dysfunction require a cardiovascular workup. Am J Med. 2014; 127:174–182. PMID: 24423973.
Article21. Vardi M, Nini A. Phosphodiesterase inhibitors for erectile dysfunction in patients with diabetes mellitus. Cochrane Database Syst Rev. 2007; (1):CD002187. PMID: 17253475.
Article22. Francis SH, Corbin JD. PDE5 inhibitors: targeting erectile dysfunction in diabetics. Curr Opin Pharmacol. 2011; 11:683–688. PMID: 21924956.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of phlorizin and acipimox on insulin resistance in STZ-diabetic rats
- Comparison of Erectile Response to Intracavernous Injection Therapy in Diabetic and Non-diabetic Erectile Dysfunction Patients
- Prevalence and Risk Factors of Erectile Dysfunction in Diabetic Men by Self-Reported Questionnaires
- Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
- Glycemic Control in Diabetic Patients with Diabetic Nephropathy