J Rheum Dis.
2013 Apr;20(2):94-102. 10.4078/jrd.2013.20.2.94.
Reciprocal Regulation of TH17 and Regulatory T Cells by Methotrexate and Its Therapeutic Effects in Collagen-induced Arthritis (CIA)
- Affiliations
-
- 1Rheumatism Research Center, Catholic Institutes of Medical Science, Seoul, Korea. rapark@catholic.ac.kr
- 2Immune Tolerance Research Center, Convergent Research Consortium for Immunologic Disease, Seoul St. Mary's Hospital, Seoul, Korea.
- 3Division of Rheumatology, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2223033
- DOI: http://doi.org/10.4078/jrd.2013.20.2.94
Abstract
OBJECTIVE
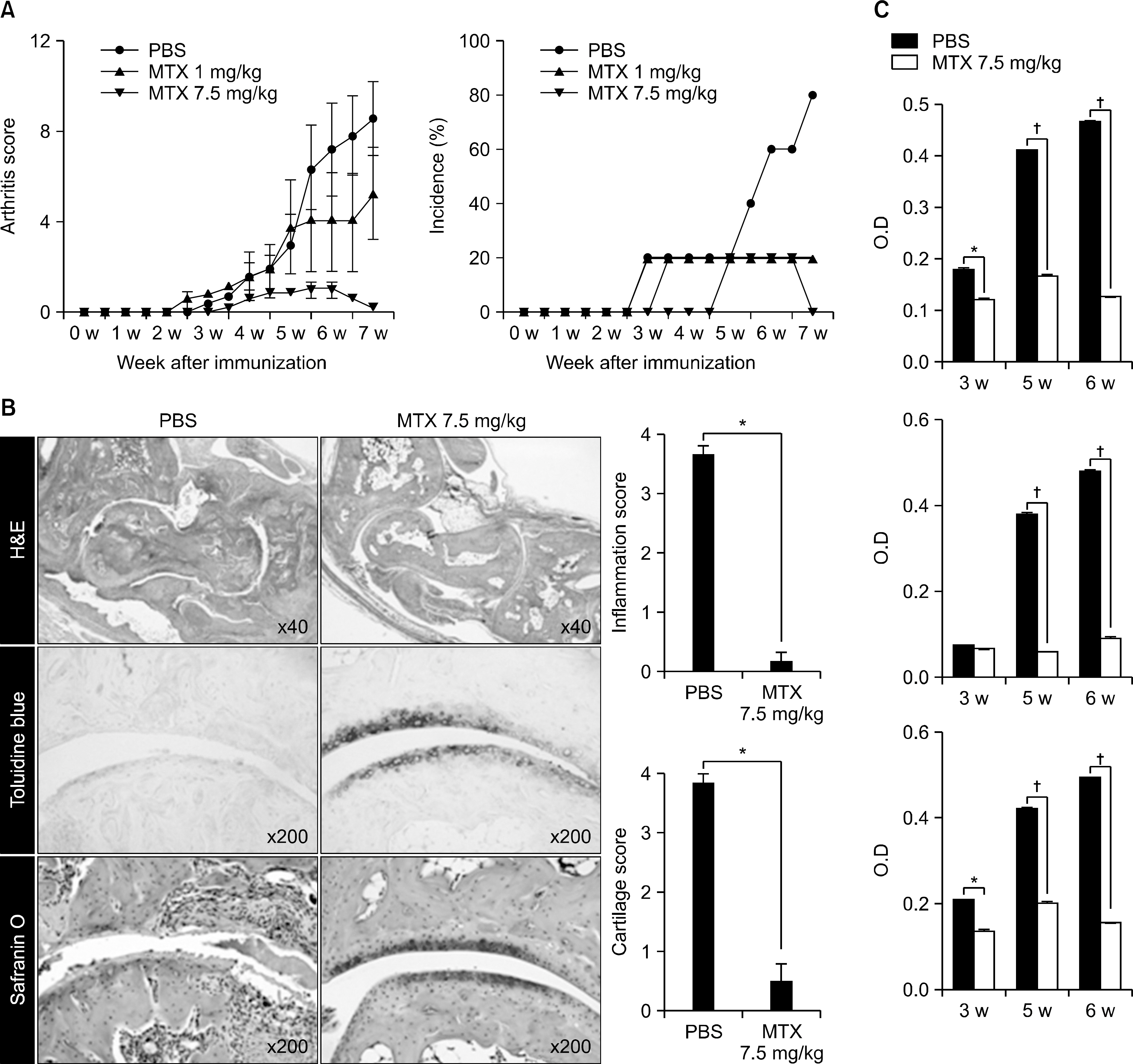
Methotrexate is the first-line drug in treatment of rheumatoid arthritis (RA) exhibiting higher efficacy and better tolerability than most other DMARDs. To have a better understanding of the anti-arthritic mechanism of methotrexate, we investigated the effect of methotrexate on suppressing the autoimmune inflammatory and destructive arthritis in collagen-induced arthritis (CIA) mice.
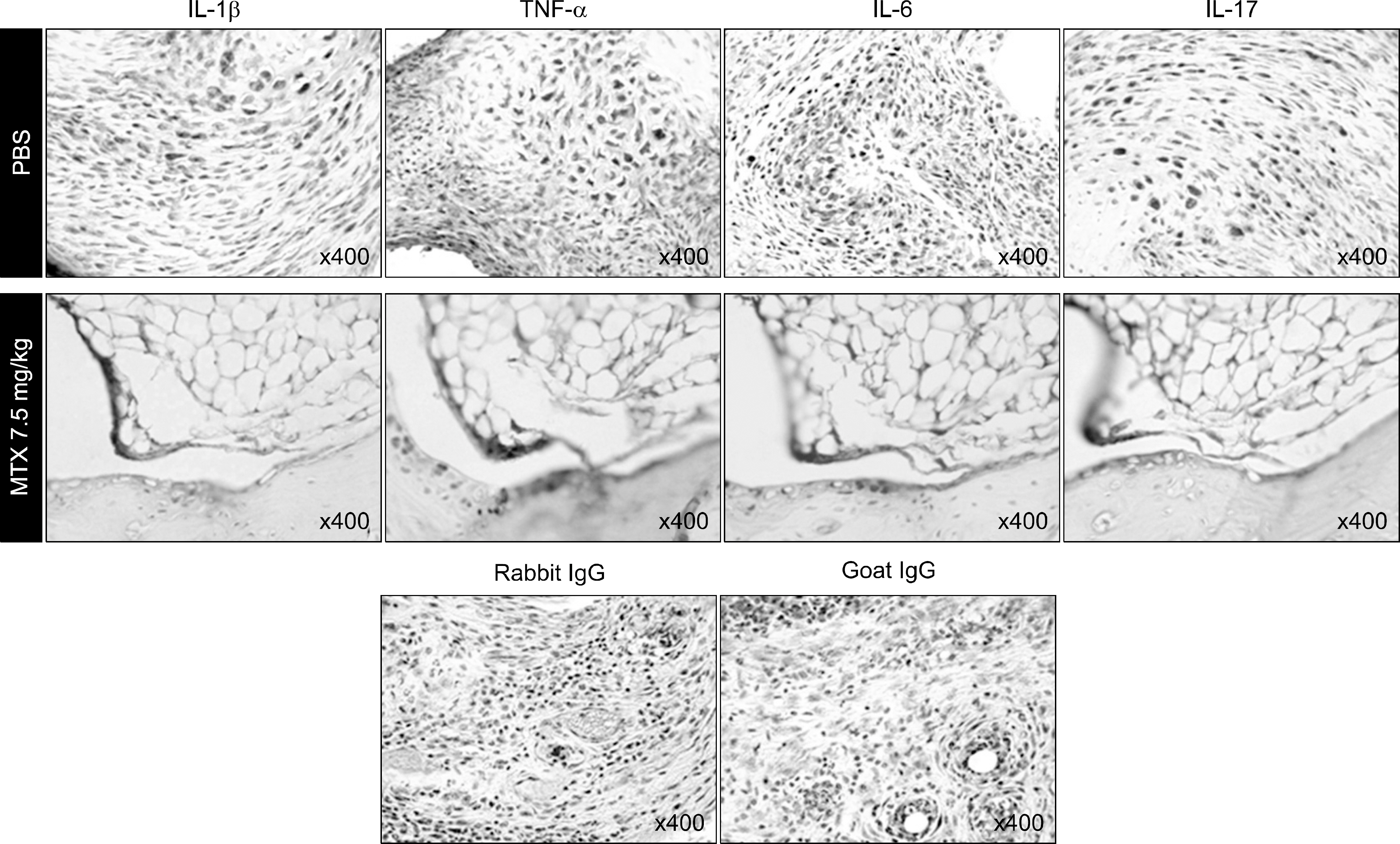
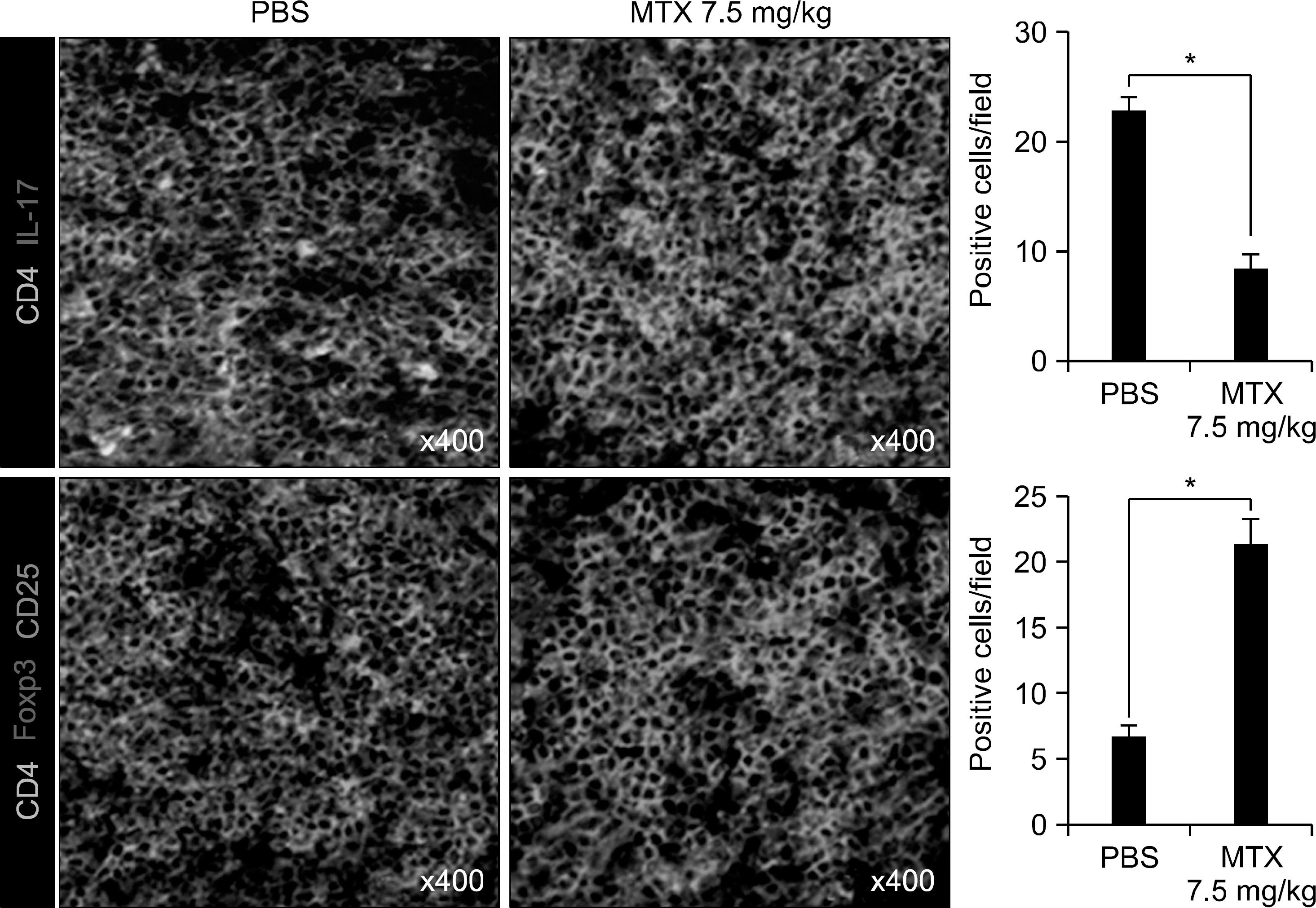
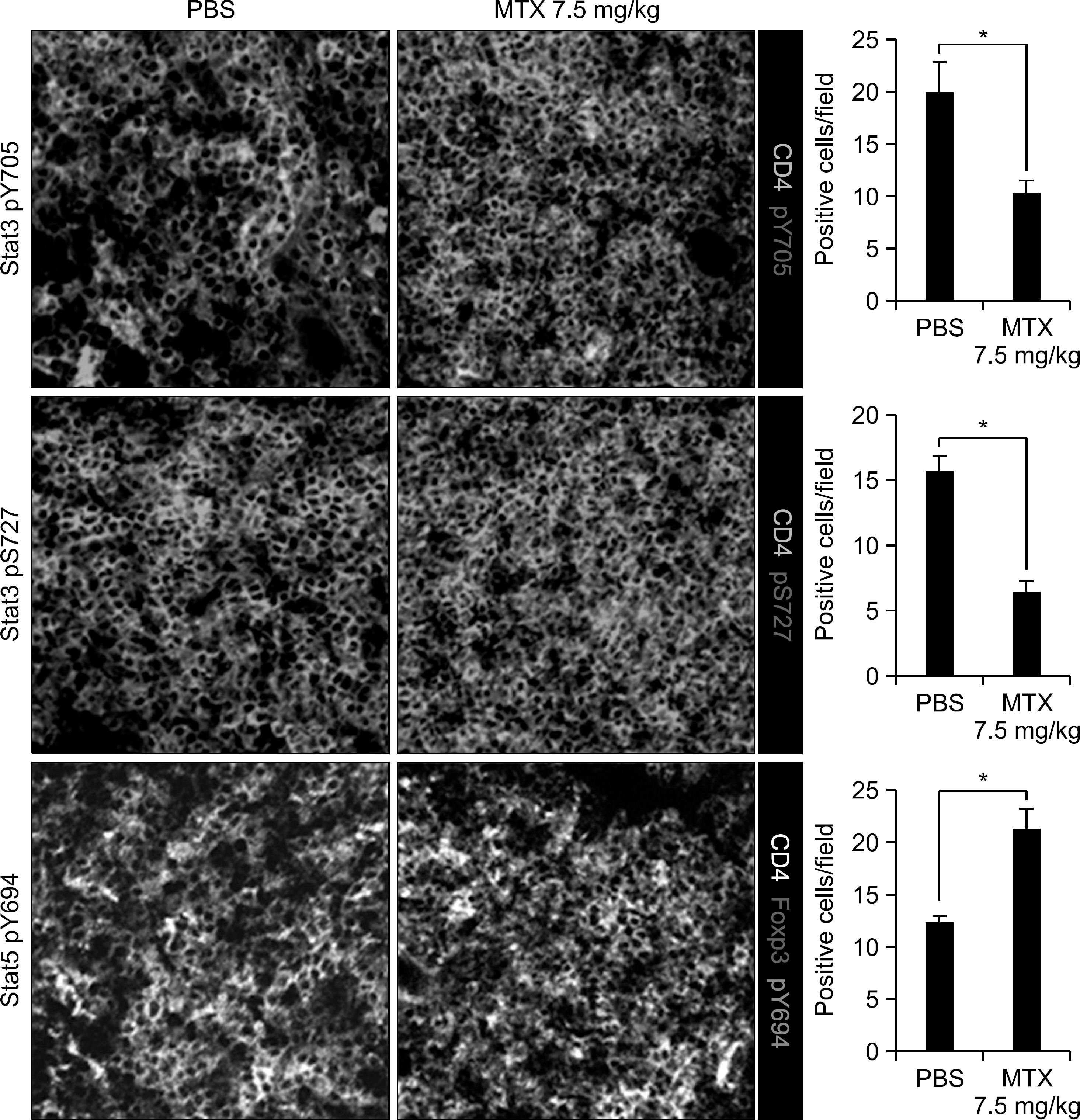
METHODS
The effects of methotrexate on joint inflammation were assessed by clinical scoring and histologic analysis. Levels of cytokines and autoreactive antibodies were analyzed by immunohistochemistry and ELISA. The population of TH17 and Foxp3+ regulatory T (Treg) cells and phosphorylation of their critical transcription activators, STAT3 and STAT5, were examined by fluorescence microscopy and flow cytometry, respectively.
RESULTS
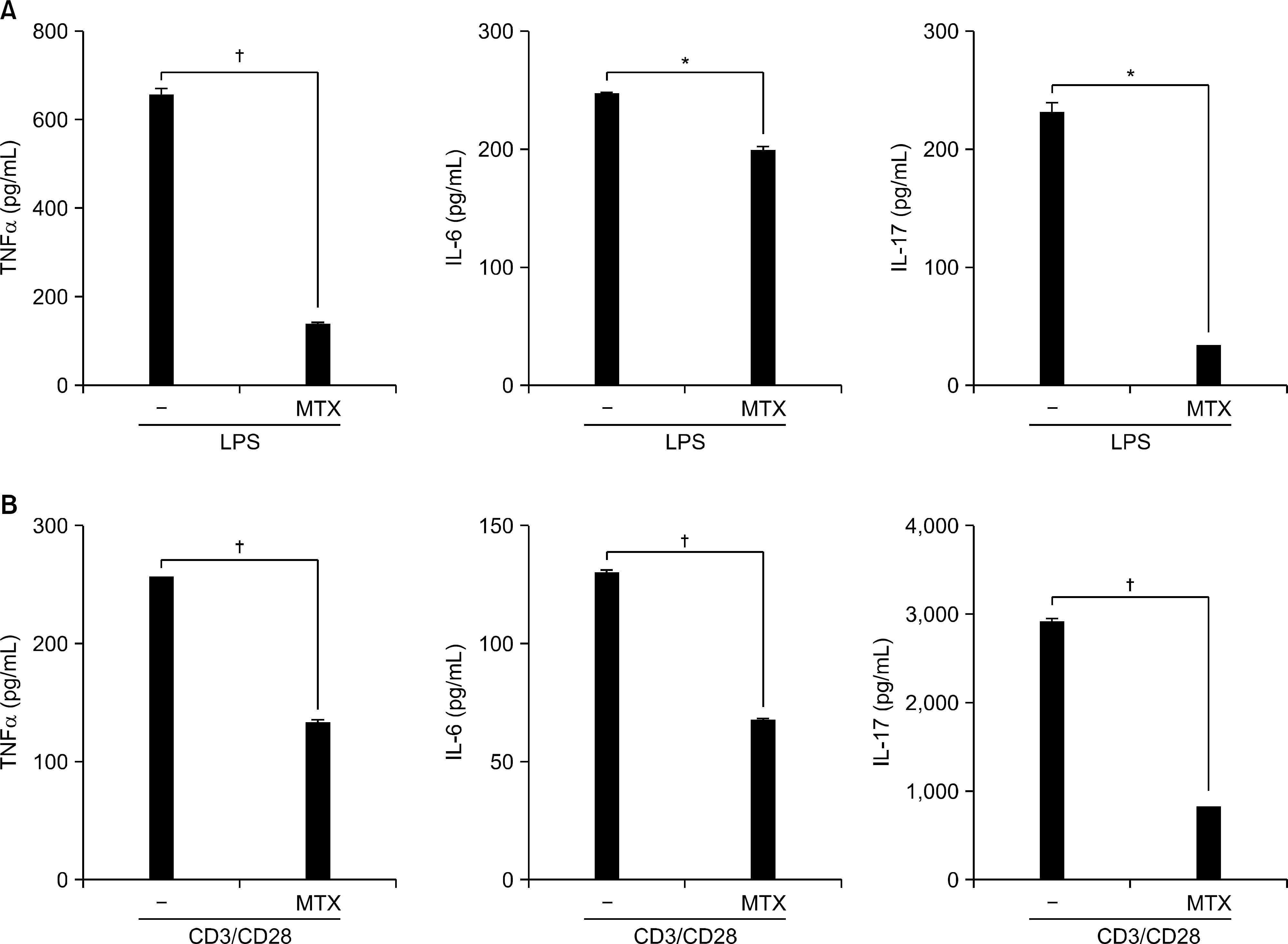
Treatment with methotrexate significantly alleviated joint inflammation and cartilage destruction in CIA. Serum levels of total immunoglobulins G, G1, G2a specific to type II collagen were also reduced considerably in methotrexate-treated mice. The drug inhibited the expression of proinflammatory cytokines such as IL-1beta, TNF-alpha, IL-6 and IL-17 in arthritic joints ex vivo as well as by splenocytes in vitro. Moreover, methotrexate treatment resulted in reciprocal modulation of TH17 cells and Foxp3+ regulatory T (Treg) cells in spleen tissues, in which TH17 cells were decreased and Treg cells in number were increased. Subsequent analysis of CD4+T cells showed that phosphorylation of STAT3 was decreased whereas phosphorylation of STAT5 was increased in methotrexate-treated mice.
CONCLUSION
Methotrexate treatment effectively suppressed autoimmune arthritis and restored homeostasis of the immune system by reciprocal regulation of TH17 and Treg cells in a mouse model of collagen-induced arthritis.
MeSH Terms
-
Animals
Antibodies
Antirheumatic Agents
Arthritis
Arthritis, Experimental
Arthritis, Rheumatoid
Cartilage
Collagen Type II
Cytokines
Enzyme-Linked Immunosorbent Assay
Flow Cytometry
Homeostasis
Immune System
Immunoglobulins
Immunohistochemistry
Inflammation
Interleukin-17
Interleukin-6
Joints
Methotrexate
Mice
Microscopy, Fluorescence
Phosphorylation
Spleen
T-Lymphocytes, Regulatory
Th17 Cells
Tumor Necrosis Factor-alpha
Antibodies
Antirheumatic Agents
Collagen Type II
Cytokines
Immunoglobulins
Interleukin-17
Interleukin-6
Methotrexate
Tumor Necrosis Factor-alpha
Figure
Reference
-
References
1. Firestein GS, Kelley WN. Kelley's textbook of rheumatology. Cannella AC, O'dell JR, editors. Methotrexate, leflunomide, sulfasalazine, hydroxychloroquine, and combination therapies. 8th ed.p. 883. Philadelphia, PA: Saunders Elsevier;2009.2. Link AA, Kino T, Worth JA, McGuire JL, Crane ML, Chrousos GP, et al. Ligand-activation of the adenosine A2a receptors inhibits IL-12 production by human monocytes. J Immunol. 2000; 164:436–42.
Article3. Haskó G, Szabó C, Németh ZH, Kvetan V, Pastores SM, Vizi ES. Adenosine receptor agonists differentially regulate IL-10, TNF-alpha, and nitric oxide production in RAW 264.7 macrophages and in endotoxemic mice. J Immunol. 1996; 157:4634–40.4. Mello SB, Barros DM, Silva AS, Laurindo IM, Novaes GS. Methotrexate as a preferential cyclooxygenase 2 inhibitor in whole blood of patients with rheumatoid arthritis. Rheumatology (Oxford). 2000; 39:533–6.
Article5. Chen Z, Laurence A, Kanno Y, Pacher-Zavisin M, Zhu BM, Tato C, et al. Selective regulatory function of Socs3 in the formation of IL-17-secreting T cells. Proc Natl Acad Sci U S A. 2006; 103:8137–42.
Article6. Durant L, Watford WT, Ramos HL, Laurence A, Vahedi G, Wei L, et al. Diverse targets of the transcription factor STAT3 contribute to T cell pathogenicity and homeostasis. Immunity. 2010; 32:605–15.
Article7. Yang XP, Ghoreschi K, Steward-Tharp SM, Rodriguez-Canales J, Zhu J, Grainger JR, et al. Opposing regulation of the locus encoding IL-17 through direct, reciprocal actions of STAT3 and STAT5. Nat Immunol. 2011; 12:247–54.
Article8. Zhou L, Lopes JE, Chong MM, Ivanov II, Min R, Victora GD, et al. TGF-beta-induced Foxp3 inhibits T(H)17 cell differentiation by antagonizing RORgammat function. Nature. 2008; 453:236–40.9. Elias KM, Laurence A, Davidson TS, Stephens G, Kanno Y, Shevach EM, et al. Retinoic acid inhibits Th17 polarization and enhances FoxP3 expression through a Stat-3/Stat-5 independent signaling pathway. Blood. 2008; 111:1013–20.
Article10. Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007; 317:256–60.11. Li Y, Jiang L, Zhang S, Yin L, Ma L, He D, et al. Methotrexate attenuates the Th17/IL-17 levels in peripheral blood mononuclear cells from healthy individuals and RA patients. Rheumatol Int. 2012; 32:2415–22.
Article12. Fiehn C, Wunder A, Krienke S, Max R, Ho AD, Moehler T. Lack of evidence for inhibition of angiogenesis as a central mechanism of the antiarthritic effect of methotrexate. Rheumatol Int. 2005; 25:108–13.
Article13. Barnett ML, Kremer JM, St Clair EW, Clegg DO, Furst D, Weisman M, et al. Treatment of rheumatoid arthritis with oral type II collagen. Results of a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 1998; 41:290–7.
Article14. Mosmann TR, Cherwinski H, Bond MW, Giedlin MA, Coffman RL. Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J Immunol. 1986; 136:2348–57.15. Harrington LE, Hatton RD, Mangan PR, Turner H, Murphy TL, Murphy KM, et al. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol. 2005; 6:1123–32.
Article16. Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, et al. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol. 2005; 6:1133–41.
Article17. Dong C. Differentiation and function of proinflammatory Th17 cells. Microbes Infect. 2009; 11:584–8.
Article18. Tesmer LA, Lundy SK, Sarkar S, Fox DA. Th17 cells in human disease. Immunol Rev. 2008; 223:87–113.
Article19. Dong C. IL-23/IL-17 biology and therapeutic considerations. J Immunotoxicol. 2008; 5:43–6.
Article20. Iwakura Y, Nakae S, Saijo S, Ishigame H. The roles of IL-17A in inflammatory immune responses and host de-fense against pathogens. Immunol Rev. 2008; 226:57–79.
Article21. Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004; 22:531–62.
Article22. Sakaguchi S, Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T. Regulatory T cells: how do they suppress immune responses? Int Immunol. 2009; 21:1105–11.
Article23. Kremer JM. Toward a better understanding of methotrexate. Arthritis Rheum. 2004; 50:1370–82.
Article24. Oh JS, Kim YG, Lee SG, So MW, Choi SW, Lee CK, et al. The effect of various disease-modifying antirheumatic drugs on the suppressive function of CD4+ CD25+ regulatory T cells. Rheumatol Int. 2013; 33:381–8.25. Kinoshita M, Kayama H, Kusu T, Yamaguchi T, Kunisawa J, Kiyono H, et al. Dietary folic acid promotes survival of Foxp3+ regulatory T cells in the colon. J Immunol. 2012; 189:2869–78.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In vivo action of IL-27: reciprocal regulation of Th17 and Treg cells in collagen-induced arthritis
- Catalpol Inhibits Tregs-to-Th17 Cell Transdifferentiation by Up-Regulating Let-7g-5p to Reduce STAT3 Protein Levels
- DW2007 Ameliorates Colitis and Rheumatoid Arthritis in Mice by Correcting Th17/Treg Imbalance and Inhibiting NF-κB Activation
- Sodium Chloride Aggravates Arthritis via Th17 Polarization
- Obesity aggravates the joint inflammation in a collagen-induced arthritis model through deviation to Th17 differentiation