Infect Chemother.
2012 Oct;44(5):395-398. 10.3947/ic.2012.44.5.395.
Disseminated Invasive Aspergillosis with Multiple Brain Abscess after Allogeneic Hematopoietic Stem Cell Transplantation Treated Successfully with Voriconazole and Neurosurgical Intervention
- Affiliations
-
- 1Department of Internal Medicine, Inha University College of Medicine, Incheon, Korea. visionyhg@hanmail.net
- 2Department of Pathology, Inha University College of Medicine, Incheon, Korea.
- 3Department of Neurosurgery, Inha University College of Medicine, Incheon, Korea.
- KMID: 2170387
- DOI: http://doi.org/10.3947/ic.2012.44.5.395
Abstract
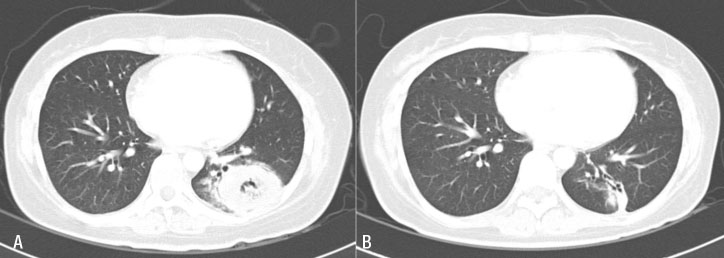
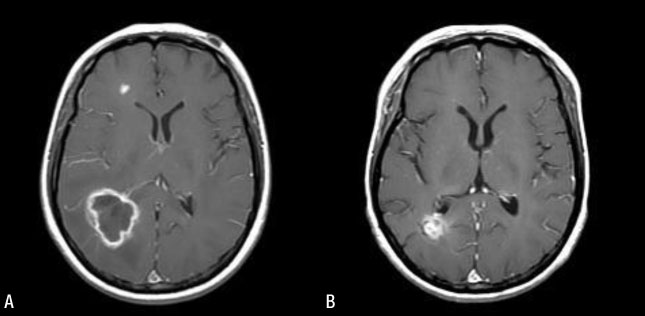
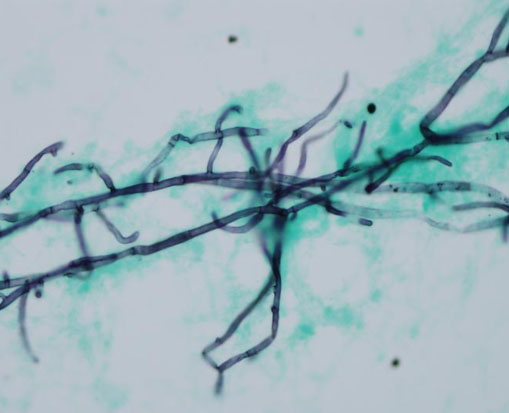
- Invasive aspergillosis is a serious infectious complication, which can occur after hematopoietic stem cell transplantation (HSCT). In particular, despite antifungal treatment, invasive aspergillosis involving the central nervous system (CNS) shows very high mortality. In principle, a neurosurgical procedure with an antifungal agent is recommended for treatment of CNS invasive aspergillosis. We encountered a patient suffering from disseminated invasive aspergillosis involving the lung, brain, and soft tissues after allogeneic HSCT for treatment of relapsed acute myeloid leukemia who was cured with voriconazole and stereotactic drainage of the brain abscess.
Keyword
MeSH Terms
Figure
Reference
-
1. Maschmeyer G, Haas A, Cornely OA. Invasive aspergillosis: epidemiology, diagnosis and management in immunocompromised patients. Drugs. 2007. 67:1567–1601.2. Lass-Flörl C. The changing face of epidemiology of invasive fungal diseases in Europe. Mycoses. 2009. 52:197–205.3. Denning DW, Stevens DA. Antifungal and surgical treatment of invasive aspergillosis: review of 2,121 published cases. Rev Infect Dis. 1990. 12:1147–1201.
Article4. Kasper EM, Bartek J Jr, Johnson S, Kasper BS, Pavlakis M, Wong M. Posttransplant aspergillosis and the role of combined neurosurgical and antifungal therapies under belatacept immunosuppression. Surg Neurol Int. 2011. 2:75.5. Coleman JM, Hogg GG, Rosenfeld JV, Waters KD. Invasive central nervous system aspergillosis: cure with liposomal amphotericin B, itraconazole, and radical surgery-case report and review of the literature. Neurosurgery. 1995. 36:858–863.6. Henze G, Aldenhoff P, Stephani U, Grosse G, Kazner E, Staib F. Successful treatment of pulmonary and cerebral aspergillosis in an immunosuppressed child. Eur J Pediatr. 1982. 138:263–265.
Article7. Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Park SW, Choe YJ, Oh MD, Choe KW. Clinical manifestations and treatment outcome of invasive aspergillosis. Korean J Infect Dis. 2002. 34:160–166.8. Meyer RD, Young LS, Armstrong D, Yu B. Aspergillosis complicating neoplastic disease. Am J Med. 1973. 54:6–15.
Article9. Chae KS, Eun JP. A case of multiple intracerebral aspergillus abscess in neonate. Infect Chemother. 2004. 36:122–126.10. Mandell GL, Douglas RG, Bennett JE, editors. Principles and practice of infectious disease. 2009. 7th ed. Philadelphia: Churchill Livingstone;3365–3369.11. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF. Infectious Diseases Society of America. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008. 46:327–360.
Article12. Schwartz S, Thiel E. Cerebral aspergillosis: tissue penetration is the key. Med Mycol. 2009. 47:Suppl 1. S387–S393.
Article13. Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B. Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002. 347:408–415.
Article14. Schwartz S, Reisman A, Troke PF. The efficacy of voriconazole in the treatment of 192 fungal central nervous system infections: a retrospective analysis. Infection. 2011. 39:201–210.
Article15. Kaffarnik M, Utzolino S, Blaich A, Hopt UT. Successful multimodal therapy of invasive pulmonary and central nervous system aspergillosis in a neutropenic surgical patient: case report and review of the literature. Mycoses. 2008. 51:74–78.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disseminated Aspergillosis following Allogeneic Hematopoietic Stem Cell Transplantation in an Acute Leukemic Patient who was Previously Treated for Invasive Aspergillosis
- Successful Allogeneic Hematopoietic Stem Cell Transplantation for a Patient with Very Severe Aplastic Anemia During Active Invasive Fungal Infection
- Liver Abscess by Aspergillus and Enterococcus faecium in a Patient with Acute Myeloid Leukemia: A Case Report and Literature Review
- Successful Hematopoietic Stem Cell Transplantation in Myelodysplastic Syndrome with Invasive Fungal Infection: A Case Report
- A Case of Invasive Pulmonary Aspergillosis Cured with Liposomal Amphotericin, Granulocyte Transfusion and Surgery in an Allogeneic Hemopoietic Stem Cell Transplantation Recipient