Korean J Hematol.
2009 Dec;44(4):289-293. 10.5045/kjh.2009.44.4.289.
Successful Hematopoietic Stem Cell Transplantation in Myelodysplastic Syndrome with Invasive Fungal Infection: A Case Report
- Affiliations
-
- 1Department of Hematology-Oncology, Soonchunhyang University School of Medicine, Bucheon, Korea. skpark@schbc.ac.kr
- 2Department of Infection, Soonchunhyang University School of Medicine, Bucheon, Korea.
- KMID: 2252113
- DOI: http://doi.org/10.5045/kjh.2009.44.4.289
Abstract
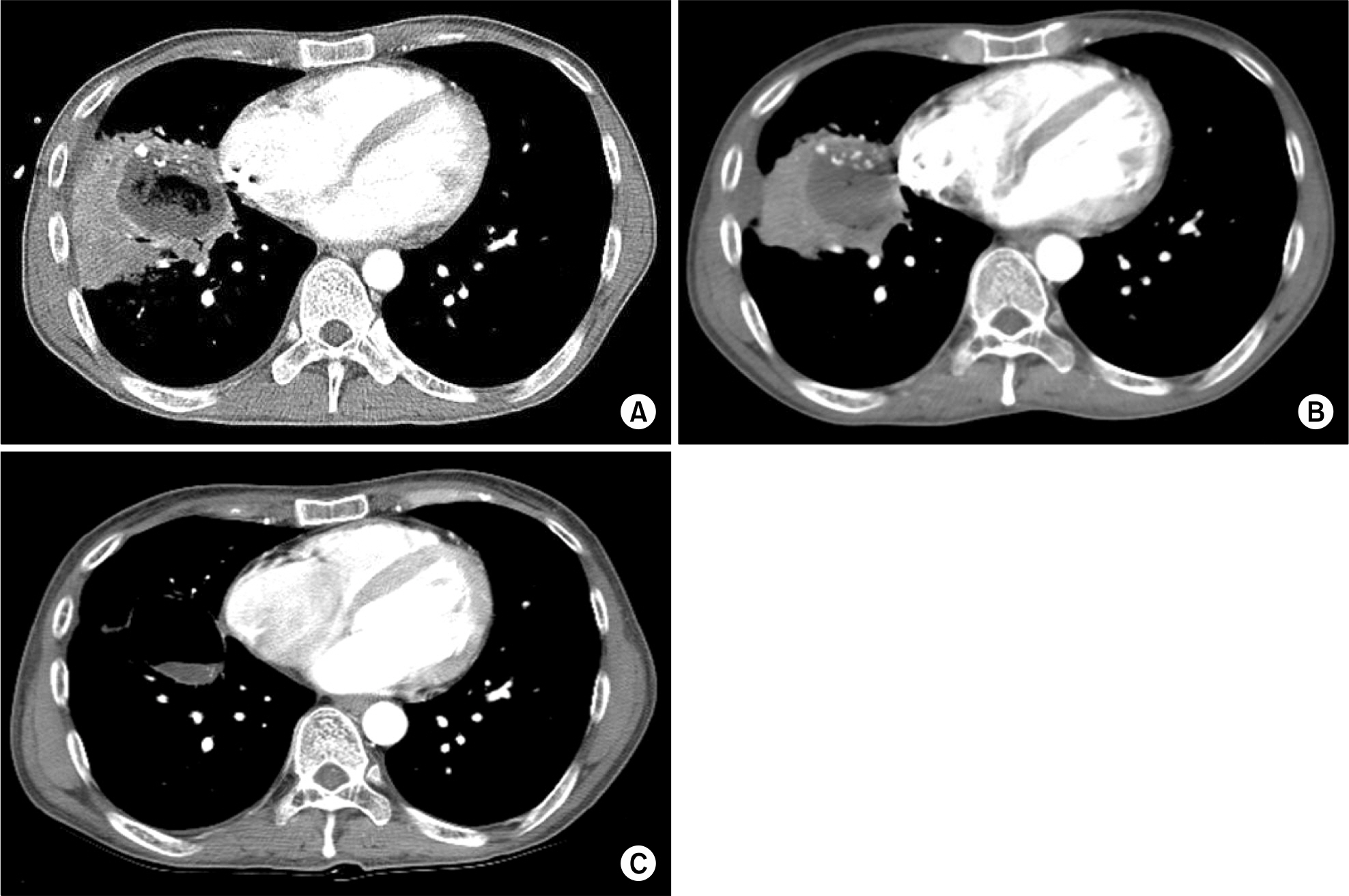
- Myelodysplastic syndrome (MDS) is a heterogeneous group of disorders characterized by ineffective hematopoiesis, morphological dysplasia, peripheral blood cytopenias, and progressive bone marrow failure. The only proven curative treatment for MDS is hematopoietic stem cell transplantation. However, invasive fungal infection following hematopoietic stem cell transplantation has become the leading cause of death from infection. Therefore, transplant candidates with previous invasive fungal infection have often been excluded from the transplant program due to high risk of reactivation and associated death. We report on a case involving an MDS patient with complications from invasive aspergillosis who had shown no response to amphotericin-B. The patient underwent successfully unrelated allogeneic hematopoietic stem cell transplantation.
MeSH Terms
Figure
Reference
-
References
1. Mufti GJ, Bennett JM, Goasguen J, et al. Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of myelodysplastic syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myelo-blasts and ring sideroblasts. Haematologica. 2008; 93:1712–7.
Article2. Kasner MT, Luger SM. Update on the therapy for myelodysplastic syndrome. Am J Hematol. 2009; 84:177–86.
Article3. Barrett AJ, Savani BN. Allogeneic stem cell transplantation for myelodysplastic syndrome. Semin Hematol. 2008; 45:49–59.
Article4. Brown JM. Fungal infections in bone marrow transplant patients. Curr Opin Infect Dis. 2004; 17:347–52.
Article5. Ruhnke M, Böhme A, Buchheidt D, et al. Diagnosis of invasive fungal infections in hematology and oncology–guidelines of the infectious diseases working party (AGIHO) of the german society of hematology and oncology (DGHO). Ann Hematol. 2003; 82(Suppl 2):S141–8.6. Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002; 347:408–15.
Article7. Bhatti Z, Shaukat A, Almyroudis NG, Segal BH. Review of epidemiology, diagnosis, and treatment of invasive mould infections in allogeneic hematopoietic stem cell transplant recipients. Mycopathologia. 2006; 162:1–15.
Article8. Martín-Dávila P, Blanes M, Fortún J. Immunosuppression and infection in transplant recipients. Enferm Infecc Microbiol Clin. 2007; 25:143–54.9. Martino R, Parody R, Fukuda T, et al. Impact of the intensity of the pretransplantation conditioning regimen in patients with prior invasive aspergillosis undergoing allogeneic hematopoietic stem cell transplantation: a retrospective survery of the infectious disease working party of the european group for blood and marrow transplantation. Blood. 2006; 108:2928–36.10. Aki ZS, Sucak GT, Yeğin ZA, Güzel D, Erbas G, Senol E. Hematopoietic stem cell transplantation in patients with active fungal infection: not a contraindication for transplantation. Transplant Proc. 2008; 40:1579–85.
Article11. Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the infectious diseases society of America. Clin Infect Dis. 2008; 46:327–60.
Article12. Zhang P, Song A, Wang Z, Feng S, Qiu L, Han M. Hematopoietic SCT in patients with a history of invasive fungal infection. Bone Marrow Transplant. 2009; 43:533–7.
Article13. Cordonnier C, Maury S, Pautas C, et al. Secondary antifungal prophylaxis with voriconazole to adhere to scheduled treatment in leukemic patients and stem cell transplant recipients. Bone Marrow Transplant. 2004; 33:943–8.
Article14. Krüger WH, Rüssmann B, de Wit M, et al. Haemopoietic cell transplantation of patients with a history of deep or invasive fungal infection during prophylaxis with liposomal amphotericin B. Acta Haematol. 2005; 113:104–8.
Article15. de Fabritiis P, Spagnoli A, Di Bartolomeo P, et al. Efficacy of caspofungin as secondary prophylaxis in patients undergoing allogeneic stem cell transplantation with prior pulmonary and/or systemic fungal infection. Bone Marrow Transplant. 2007; 40:245–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful treatment of myelodysplastic syndrome and Behcet colitis after allogeneic hematopoietic stem cell transplantation
- Evans Syndrome following T Cell-repleted Unrelated Bone Marrow Transplantation for Myelodysplastic Syndrome: Successful Response to High-dose Corticosteroid
- Successful Allogeneic Hematopoietic Stem Cell Transplantation for a Patient with Very Severe Aplastic Anemia During Active Invasive Fungal Infection
- Erratum: Lung Ultrasound to Evaluate Invasive Fungal Diseases after Allogeneic Hematopoietic Stem Cell Transplantation
- Allogeneic hematopoietic stem cell transplantation for myelodysplastic syndromes