Yonsei Med J.
2016 Jan;57(1):180-186. 10.3349/ymj.2016.57.1.180.
Impact of Angiotensin Converting Enzyme Inhibitor versus Angiotensin Receptor Blocker on Incidence of New-Onset Diabetes Mellitus in Asians
- Affiliations
-
- 1Department of Cardiology, Eulji General Hospital, Eulji University College of Medicine, Seoul, Korea.
- 2Cardiovascular Center, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea. swrha617@yahoo.co.kr
- 3Department of Computer Science, Korea Advanced Institute of Science and Technology, Daejeon, Korea.
- KMID: 2466368
- DOI: http://doi.org/10.3349/ymj.2016.57.1.180
Abstract
- PURPOSE
Angiotensin converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) are associated with a decreased incidence of new-onset diabetes mellitus (NODM). The aim of this study was to compare the protective effect of ACEI versus ARBs on NODM in an Asian population.
MATERIALS AND METHODS
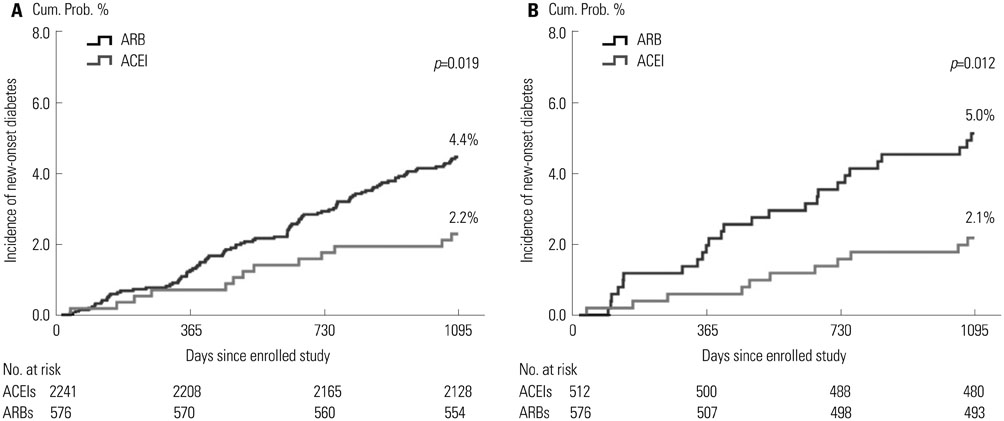
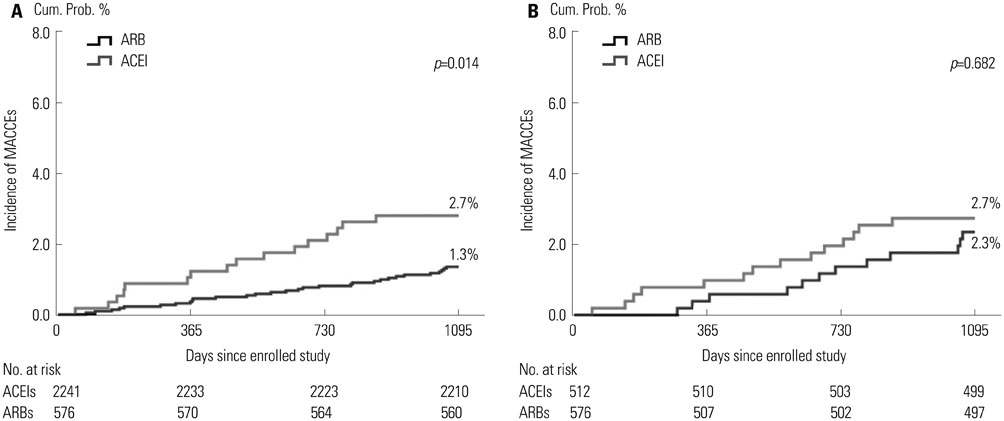
We investigated a total of 2817 patients who did not have diabetes mellitus from January 2004 to September 2009. To adjust for potential confounders, a propensity score matched (PSM) analysis was performed using a logistic regression model. The primary end-point was the cumulative incidence of NODM, which was defined as having a fasting blood glucose > or =126 mg/dL or HbA1c > or =6.5%. Multivariable cox-regression analysis was performed to determine the impact of ACEI versus ARB on the incidence of NODM.
RESULTS
Mean follow-up duration was 1839+/-1019 days in all groups before baseline adjustment and 1864+/-1034 days in the PSM group. After PSM (C-statistics=0.731), a total 1024 patients (ACEI group, n=512 and ARB group, n=512) were enrolled for analysis and baseline characteristics were well balanced. After PSM, the cumulative incidence of NODM at 3 years was lower in the ACEI group than the ARB group (2.1% vs. 5.0%, p=0.012). In multivariate analysis, ACEI vs. ARB was an independent predictor of the lower incidence for NODM (odd ratio 0.37, confidence interval 0.17-0.79, p=0.010).
CONCLUSION
In the present study, compared with ARB, chronic ACEI administration appeared to be associated with a lower incidence of NODM in a series of Asian cardiovascular patients.
MeSH Terms
-
Adult
Aged
Angiotensin Receptor Antagonists/*therapeutic use
Angiotensin-Converting Enzyme Inhibitors/*therapeutic use
Asian Continental Ancestry Group/*statistics & numerical data
Blood Glucose/analysis
Diabetes Mellitus/*diagnosis/*epidemiology
Dose-Response Relationship, Drug
Drug Monitoring/methods
Female
Follow-Up Studies
Humans
Hypertension/*drug therapy
Incidence
Kaplan-Meier Estimate
Logistic Models
Male
Middle Aged
Multivariate Analysis
Propensity Score
Republic of Korea/epidemiology
Risk Factors
Angiotensin Receptor Antagonists
Angiotensin-Converting Enzyme Inhibitors
Blood Glucose
Figure
Reference
-
1. Underwood PC, Adler GK. The renin angiotensin aldosterone system and insulin resistance in humans. Curr Hypertens Rep. 2013; 15:59–70.
Article2. Scheen AJ. Renin-angiotensin system inhibition prevents type 2 diabetes mellitus. Part 1. A meta-analysis of randomised clinical trials. Diabetes Metab. 2004; 30:487–496.3. Chung O, Unger T. Angiotensin II receptor blockade and end-organ protection. Am J Hypertens. 1999; 12(12 Pt 1-2):150S–156S.
Article4. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013; 36:Suppl 1. S67–S74.5. Hasvold LP, Bodegård J, Thuresson M, Stålhammar J, Hammar N, Sundström J, et al. Diabetes and CVD risk during angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker treatment in hypertension: a study of 15,990 patients. J Hum Hypertens. 2014; 28:663–669.
Article6. Basile JN. Antihypertensive therapy, new-onset diabetes, and cardiovascular disease. Int J Clin Pract. 2009; 63:656–666.
Article7. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006; 444:840–846.
Article8. Ferrari R, Pasanisi G, Notarstefano P, Campo G, Gardini E, Ceconi C. Specific properties and effect of perindopril in controlling the renin-angiotensin system. Am J Hypertens. 2005; 18(9 Pt 2):142S–154S.
Article9. Ridker PM. JUPITER Study Group. Rosuvastatin in the primary prevention of cardiovascular disease among patients with low levels of low-density lipoprotein cholesterol and elevated high-sensitivity C-reactive protein: rationale and design of the JUPITER trial. Circulation. 2003; 108:2292–2297.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nursing Management in Diabetes during Pregnancy
- Selection of Antihypertensive Drugs in Hypertensive Patients with Diabetes Mellitus: In Pohang-Gyeongju Primary Care Research Network
- Use of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: A Closer Look at Hyperkalemia
- Effect of Angiotensin Converting Enzyme Inhibitors on Induced Angiotensin Converting Enzyme Activity in Rat Intestine
- A case of angioedema associated with losartan