Nutr Res Pract.
2019 Dec;13(6):509-520. 10.4162/nrp.2019.13.6.509.
Effects of a mobile healthcare service provided by public health centers on practicing of health behaviors and health risk factors
- Affiliations
-
- 1Korea Health Promotion Institute, Seoul 04554, Korea.
- 2Department of Family Medicine, Seoul Paik Hospital, Inje University College of Medicine, 9, Mareunnae-ro, Jung-gu, Seoul 04551, Korea. yangimhur@gmail.com
- 3Department of Family Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University College of Medicine, Seoul 03181, Korea. fmleader@nuri.net
- KMID: 2464130
- DOI: http://doi.org/10.4162/nrp.2019.13.6.509
Abstract
- BACKGROUND/OBJECTIVES
This study evaluated whether a mobile health (mHealth) application can instigate healthy behavioral changes and improvements in metabolic disorders in individuals with metabolic abnormalities.
SUBJECTS/METHODS
Participants were divided into an mHealth intervention group (IG), which used a mobile app for 24 weeks, and a conventional IG. All mobile apps featured activity monitors, with blood pressure and glucose monitors, and body-composition measuring devices. The two groups were compared after 24 weeks in terms of health-behavior practice rate and changes in the proportion of people with health risks, and health behaviors performed by the IG that contributed to reductions in more than one health risk factor were analyzed using multiple logistic regression.
RESULTS
Preference for low-sodium diet, reading nutritional facts, having breakfast, and performing moderate physical activity significantly increased in the mHealth IG. Furthermore, the mHealth IG showed a significant increase of eight items in the mini-dietary assessment; particularly, the items "I eat at least two types of vegetables of various colors at every meal" and "I consume dairies, such as milk, yogurt, and cheese, every day." The proportion of people with health risks, with the exception of fasting glucose, significantly decreased in the mHealth IG, while only the proportion of people with at-risk triglycerides and waist circumference of females significantly decreased in the control group. Finally, compared to those who did not show improvements of health risks, those who showed improvements of health risks in the mHealth IG had an odds ratio of 1.61 for moderate to vigorous physical activity, 1.65 for "I do not add more salt or soy sauce in my food," and 1.77 for "I remove fat in my meat before eating."
CONCLUSIONS
The findings suggest that the additional use of a community-based mHealth service through a mobile application is effective for improving health behaviors and lowering metabolic risks in Koreans.
Keyword
MeSH Terms
-
Blood Pressure
Breakfast
Cheese
Delivery of Health Care*
Diet
Diet, Sodium-Restricted
Disease Management
Fasting
Female
Glucose
Health Behavior*
Humans
Logistic Models
Meat
Milk
Mobile Applications
Motor Activity
Odds Ratio
Public Health*
Risk Factors*
Smartphone
Soy Foods
Telemedicine
Triglycerides
Vegetables
Waist Circumference
Yogurt
Glucose
Triglycerides
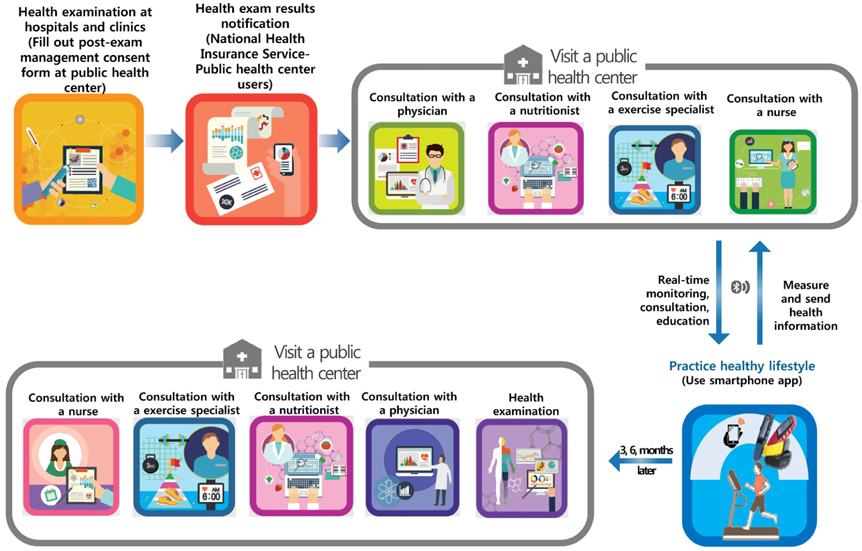
Figure
Reference
-
1. World Health Organization. Global status report on noncommunicable diseases 2014 [Internet]. Geneva: World Health Organization;2014. cited 2017 December 5. Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/.2. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM;. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346:393–403.
Article3. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002; 106:3143–3421.4. Cardiometabolic Risk Working Group: Executive Committee. Leiter LA, Fitchett DH, Gilbert RE, Gupta M, Mancini GB, McFarlane PA, Ross R, Teoh H, Verma S, Anand S, Camelon K, Chow CM, Cox JL, Després JP, Genest J, Harris SB, Lau DC, Lewanczuk R, Liu PP, Lonn EM, McPherson R, Poirier P, Qaadri S, Rabasa-Lhoret R, Rabkin SW, Sharma AM, Steele AW, Stone JA, Tardif JC, Tobe S, Ur E. Cardiometabolic risk in Canada: a detailed analysis and position paper by the cardiometabolic risk working group. Can J Cardiol. 2011; 27:e1–e33.
Article5. Huffman KM, Sun JL, Thomas L, Bales CW, Califf RM, Yates T, Davies MJ, Holman RR, McMurray JJ, Bethel MA, Tuomilehto J, Haffner SM, Kraus WE. Impact of baseline physical activity and diet behavior on metabolic syndrome in a pharmaceutical trial: results from NAVIGATOR. Metabolism. 2014; 63:554–561.
Article6. World Health Organization. Adherence to long-term therapies: evidence for action 2013 [Internet]. Geneva: World Health Organization;2003. cited 2017 December 5. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/.7. Murdock A, Rodgers C, Lindsay H, Tham TC. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J R Soc Med. 2002; 95:284–286.
Article8. Paterson BL, Charlton P, Richard S. Non-attendance in chronic disease clinics: a matter of non-compliance? J Nurs Healthc Chronic Illn. 2010; 2:63–74.
Article9. Oh B, Cho B, Han MK, Choi H, Lee MN, Kang HC, Lee CH, Yun H, Kim Y. The effectiveness of mobile phone-based care for weight control in metabolic syndrome patients: randomized controlled trial. JMIR Mhealth Uhealth. 2015; 3:e83.
Article10. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011; 1:53–71.
Article11. Payne HE, Lister C, West JH, Bernhardt JM. Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR Mhealth Uhealth. 2015; 3:e20.
Article12. World Health Organization. mHealth: new horizons for health through mobile technologies [Internet]. Geneva: World Health Organization;2011. cited 2017 December 5. Available from: https://www.who.int/goe/publications/goe_mhealth_web.pdf.13. Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008; 35:177–181.
Article14. Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, Vandelanotte C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016; 13:127.
Article15. Piette JD, List J, Rana GK, Townsend W, Striplin D, Heisler M. Mobile health devices as tools for worldwide cardiovascular risk reduction and disease management. Circulation. 2015; 132:2012–2027.
Article16. Norman GJ, Kolodziejczyk JK, Adams MA, Patrick K, Marshall SJ. Fruit and vegetable intake and eating behaviors mediate the effect of a randomized text-message based weight loss program. Prev Med. 2013; 56:3–7.
Article17. Park MJ, Kim HS. Evaluation of mobile phone and Internet intervention on waist circumference and blood pressure in post-menopausal women with abdominal obesity. Int J Med Inform. 2012; 81:388–394.
Article18. Liang X, Wang Q, Yang X, Cao J, Chen J, Mo X, Huang J, Wang L, Gu D. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011; 28:455–463.
Article19. Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, Feig DS, Cafazzo JA. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012; 60:51–57.
Article20. Park LG, Howie-Esquivel J, Chung ML, Dracup K. A text messaging intervention to promote medication adherence for patients with coronary heart disease: a randomized controlled trial. Patient Educ Couns. 2014; 94:261–268.
Article21. Cowdery J, Majeske P, Frank R, Brown D. Exergame apps and physical activity: the results of the ZOMBIE trial. Am J Health Educ. 2015; 46:216–222.
Article22. Gasser R, Brodbeck D, Degen M, Luthiger J, Wyss R, Reichlinal S. Persuasiveness of a mobile lifestyle coaching application using social facilitation. In : IJsselsteijn WA, de Kort YAW, Midden C, Eggen B, van den Hoven E, editors. Persuasive Technology. PERSUASIVE 2006. Lecture Notes in Computer Science, vol 3962. Berlin/Heidelberg: Springer;2006. p. 27–38.23. Wharton CM, Johnston CS, Cunningham BK, Sterner D. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial. J Nutr Educ Behav. 2014; 46:440–444.
Article24. Wigginton C, Curran M, Brodeur C. Global Mobile Consumer Trends. 2nd ed. New York (NY): Deloitte Touche Tohmatsu Ltd.;2017.25. Song TM, Ryu S, Lee SH. U-health service for managing chronic disease: a case study on managing metabolic syndrome in a health center in South Korea. Healthc Inform Res. 2011; 17:260–266.
Article26. Joo NS, Kim BT. Mobile phone short message service messaging for behaviour modification in a community-based weight control programme in Korea. J Telemed Telecare. 2007; 13:416–420.
Article27. Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet. 2005; 366:1059–1062.
Article28. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, Kim DY, Kwon HS, Kim SR, Lee CB, Oh SJ, Park CY, Yoo HJ. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75:72–80.
Article29. Ministry of Health and Welfare, Korea Health Promotion Institute. One-Stop Health service Consultation Manual. Seoul: Korea Health Promotion Institute;2011.30. Ministry of Health and Welfare, Korea Health Promotion Institute. Health Exam Result Consultation Manual - Nutritional Consultation. Seoul: Korea Health Promotion Institute;2012.31. McKay FH, Cheng C, Wright A, Shill J, Stephens H, Uccellini M. Evaluating mobile phone applications for health behaviour change: a systematic review. J Telemed Telecare. 2018; 24:22–30.
Article32. Kelly JT, Reidlinger DP, Hoffmann TC, Campbell KL. Telehealth methods to deliver dietary interventions in adults with chronic disease: a systematic review and meta-analysis. Am J Clin Nutr. 2016; 104:1693–1702.
Article33. Ezzati M, Riboli E. Behavioral and dietary risk factors for noncommunicable diseases. N Engl J Med. 2013; 369:954–964.
Article34. Logan AG. Transforming hypertension management using mobile health technology for telemonitoring and self-care support. Can J Cardiol. 2013; 29:579–585.
Article35. Weinstein RS, Lopez AM, Joseph BA, Erps KA, Holcomb M, Barker GP, Krupinski EA. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med. 2014; 127:183–187.
Article36. Safran Naimark J, Madar Z, Shahar DR. The impact of a web-based app (eBalance) in promoting healthy lifestyles: randomized controlled trial. J Med Internet Res. 2015; 17:e56.
Article37. Stuckey M, Russell-Minda E, Read E, Munoz C, Shoemaker K, Kleinstiver P, Petrella R. Diabetes and Technology for Increased Activity (DaTA) study: results of a remote monitoring intervention for prevention of metabolic syndrome. J Diabetes Sci Technol. 2011; 5:928–935.
Article38. Partridge SR, McGeechan K, Hebden L, Balestracci K, Wong AT, Denney-Wilson E, Harris MF, Phongsavan P, Bauman A, Allman-Farinelli M. Effectiveness of a mHealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: Randomized controlled trial. JMIR Mhealth Uhealth. 2015; 3:e66.
Article39. Allman-Farinelli M, Partridge SR, McGeechan K, Balestracci K, Hebden L, Wong A, Phongsavan P, Denney-Wilson E, Harris MF, Bauman A. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): Nine-month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth. 2016; 4:e78.
Article40. Hebden L, Cook A, van der Ploeg HP, King L, Bauman A, Allman-Farinelli M. A mobile health intervention for weight management among young adults: a pilot randomised controlled trial. J Hum Nutr Diet. 2014; 27:322–332.
Article41. Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, Newell J, OLaighin G, Heaney D, O'Donnell M, Murphy AW. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. Br J Gen Pract. 2014; 64:e384–e391.
Article42. Spring B, Gotsis M, Paiva A, Spruijt-Metz D. Healthy apps: mobile devices for continuous monitoring and intervention. IEEE Pulse. 2013; 4:34–40.
Article43. Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Behav Nutr Phys Act. 2012; 9:52.
Article44. Dennison L, Morrison L, Conway G, Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013; 15:e86.
Article45. Guertler D, Vandelanotte C, Kirwan M, Duncan MJ. Engagement and nonusage attrition with a free physical activity promotion program: the case of 10,000 steps Australia. J Med Internet Res. 2015; 17:e176.
Article46. Sandholzer M, Deutsch T, Frese T, Winter A. Predictors of students' self-reported adoption of a smartphone application for medical education in general practice. BMC Med Educ. 2015; 15:91.
Article47. He D, Xi B, Xue J, Huai P, Zhang M, Li J. Association between leisure time physical activity and metabolic syndrome: a meta-analysis of prospective cohort studies. Endocrine. 2014; 46:231–240.
Article48. Zhang D, Liu X, Liu Y, Sun X, Wang B, Ren Y, Zhao Y, Zhou J, Han C, Yin L, Zhao J, Shi Y, Zhang M, Hu D. Leisure-time physical activity and incident metabolic syndrome: a systematic review and dose-response meta-analysis of cohort studies. Metabolism. 2017; 75:36–44.
Article49. McTiernan A, Sorensen B, Irwin ML, Morgan A, Yasui Y, Rudolph RE, Surawicz C, Lampe JW, Lampe PD, Ayub K, Potter JD. Exercise effect on weight and body fat in men and women. Obesity (Silver Spring). 2007; 15:1496–1512.
Article50. Trapp EG, Chisholm DJ, Freund J, Boutcher SH. The effects of high-intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int J Obes (Lond). 2008; 32:684–691.
Article51. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43:1334–1359.
Article52. Department of Health, Social Services and Public Safety. The Scottish Governmnet. Llywodraeth Cymru Welsh Government. Department of Health (GB). Start active, stay active: a report on physical activity for health from the four home countries' Chief Medical Officers [Internet]. London: Department of Health;2011. cited 2017 December 5. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf.53. Boeing H, Bechthold A, Bub A, Ellinger S, Haller D, Kroke A, Leschik-Bonnet E, Müller MJ, Oberritter H, Schulze M, Stehle P, Watzl B. Critical review: vegetables and fruit in the prevention of chronic diseases. Eur J Nutr. 2012; 51:637–663.
Article54. Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013; 346:f1378.
Article55. Streppel MT, Arends LR, van 't Veer P, Grobbee DE, Geleijnse JM. Dietary fiber and blood pressure: a meta-analysis of randomized placebo-controlled trials. Arch Intern Med. 2005; 165:150–156.56. Wanders AJ, van den Borne JJ, de Graaf C, Hulshof T, Jonathan MC, Kristensen M, Mars M, Schols HA, Feskens EJ. Effects of dietary fibre on subjective appetite, energy intake and body weight: a systematic review of randomized controlled trials. Obes Rev. 2011; 12:724–739.
Article57. Weickert MO, Pfeiffer AF. Metabolic effects of dietary fiber consumption and prevention of diabetes. J Nutr. 2008; 138:439–442.
Article58. Cobiac LJ, Vos T, Veerman JL. Cost-effectiveness of interventions to promote fruit and vegetable consumption. PLoS One. 2010; 5:e14148.
Article59. Oh H, Lee HY, Jun DW, Lee SM. Low salt diet and insulin resistance. Clin Nutr Res. 2016; 5:1–6.
Article60. Zock PL, Blom WA, Nettleton JA, Hornstra G. Progressing insights into the role of dietary fats in the prevention of cardiovascular disease. Curr Cardiol Rep. 2016; 18:111.
Article61. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. National Health Survey 1998; 2001 National Health and Nutrition Survey; The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005; Korea Health Statistics 2007: Korea National Health and Nutrition Examination Survey (KNHANES IV-1); Korea Health Statistics 2008: Korea National Health and Nutrition Examination Survey (KNHANES IV-2); Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANES IV-3); Korea Health Statistics 2010: Korea National Health and Nutrition Examination Survey (KNHANES V-1); Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2); Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3). Cheongwon: Korea Centers for Disease Control and Prevention;c1999-2013.62. Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, Weisel H, Heshka S, Matthews DE, Heymsfield SB. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992; 327:1893–1898.
Article63. Pietersma S, Dijkstra A. Do behavioural health intentions engender health behaviour change? A study on the moderating role of self-affirmation on actual fruit intake versus vegetable intake. Br J Health Psychol. 2011; 16:815–827.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of Mobile Health Application Use to Improve Health Behavior Changes: A Systematic Review of Randomized Controlled Trials
- Factors Associated with Nurse Self-Leadership: A Cross-Sectional Study of Nurses Working at Public Health Centers and Primary Healthcare Posts
- Is a New Public Medical School Linked to Compulsory Service Necessary to Strengthen Public Health Care in Korea?: Who Wants to Build a New Public Medical School Linked to Compulsory Service? And Why?
- The Current Status and Propects of Community Nutrition Services: II. The Perception and Needs of Community Nutrition Services among the Residents of the Pilot Service Areas
- Peer-to-Peer JXTA Architecture for Continuing Mobile Medical Education Incorporated in Rural Public Health Centers