Yonsei Med J.
2018 Dec;59(10):1197-1204. 10.3349/ymj.2018.59.10.1197.
The Brain Donation Program in South Korea
- Affiliations
-
- 1Department of Neurology, Sungkyunkwan University School of Medicine, Samsung Medical Center, Seoul, Korea. sangwonseo@empas.com
- 2Department of Neurology, Kangwon National University Hospital, Kangwon National University College of Medicine, Chuncheon, Korea.
- 3Department of Pathology, Sungkyunkwan University School of Medicine, Samsung Medical Center, Seoul, Korea. yl.suh@samsung.com
- 4Department of Pathology, Samsung Medical Center, Seoul, Korea.
- 5Administarative Office, Sungkyunkwan University School of Medicine, Suwon, Korea.
- 6Neuroscience Center, Samsung Medical Center, Seoul, Korea.
- 7Department of Pathology, College of Medicine, Hallym University, Chuncheon, Korea.
- 8Department of Forensic Medicine, Pusan National University School of Medicine, Yangsan, Korea.
- 9Department of Neurology, Pusan National University Hospital, Busan, Korea.
- 10Department of Neurology, Jeju National University College of Medicine, Jeju, Korea.
- 11Department of Forensic Medicine, Jeju National University College of Medicine, Jeju, Korea.
- 12Division of Brain Diseases, Center for Biomedical Sciences, Korea National Institute of Health, Cheongju, Korea.
- 13Department of Neurology, Chonnam National University Medical School, Gwangju, Korea.
- 14Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
- 15Department of Neurology, School of Medicine, Brain Science and Engineering Institute, Kyungpook National University, Daegu, Korea.
- 16Department of Neurology, School of Medicine, Ajou University, Suwon, Korea.
- 17Memory and Aging Center, Departments of Neurology and Pathology, University of California, San Francisco, CA, USA.
- 18Department of Anatomy & Cell Biology, Sungkyunkwan University School of Medicine, Suwon, Korea.
- KMID: 2426334
- DOI: http://doi.org/10.3349/ymj.2018.59.10.1197
Abstract
- PURPOSE
Obtaining brain tissue is critical to definite diagnosis and to furthering understanding of neurodegenerative diseases. The present authors have maintained the National Neuropathology Reference and Diagnostic Laboratories for Dementia in South Korea since 2016. We have built a nationwide brain bank network and are collecting brain tissues from patients with neurodegenerative diseases. We are aiming to facilitate analyses of clinic-pathological and image-pathological correlations of neurodegenerative disease and to broaden understanding thereof.
MATERIALS AND METHODS
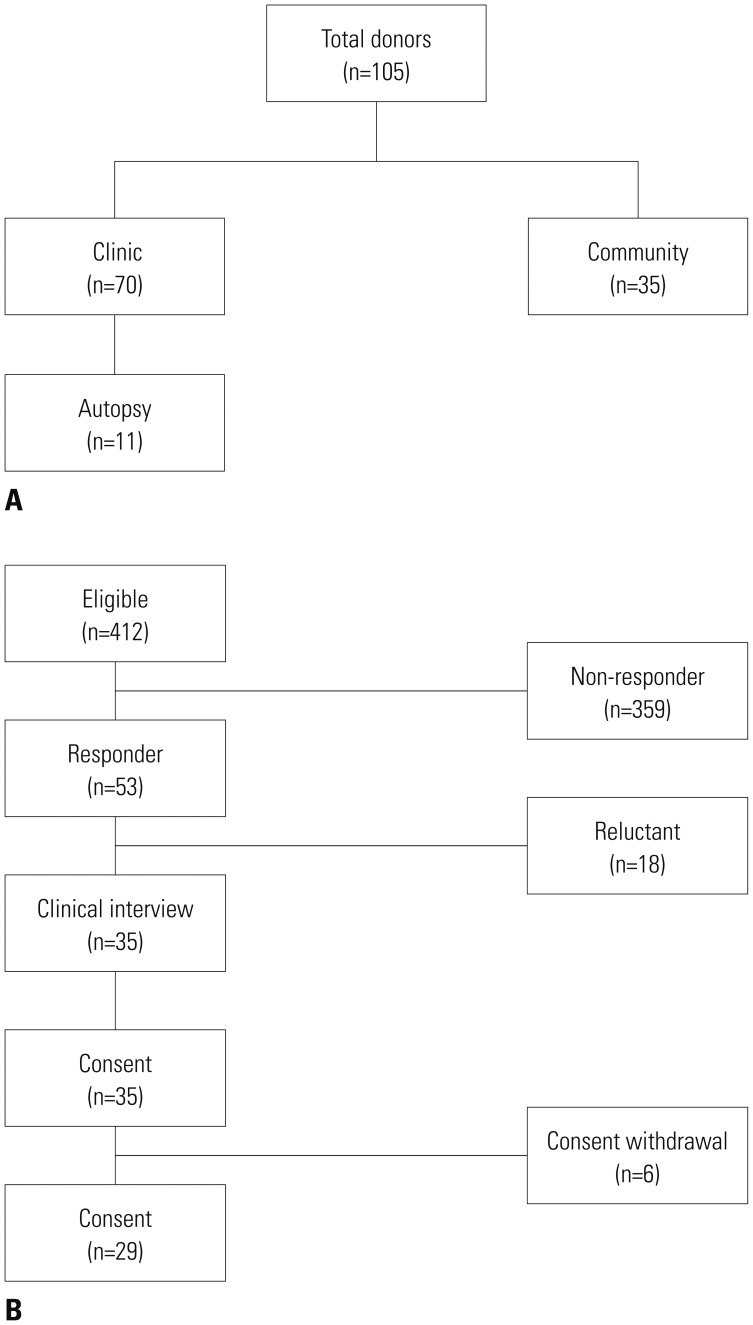
We recruited participants through two routes: from memory clinics and the community. As a baseline evaluation, clinical interviews, a neurological examination, laboratory tests, neuropsychological tests, and MRI were undertaken. Some patients also underwent amyloid PET.
RESULTS
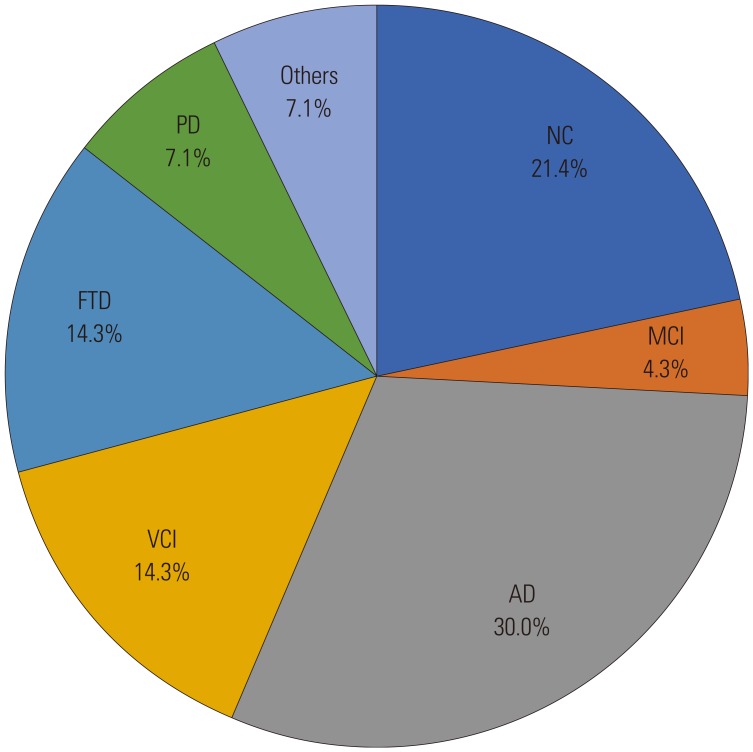
We recruited 105 participants, 70 from clinics and 35 from the community. Among them, 11 died and were autopsied. The clinical diagnoses of the autopsied patients included four with Alzheimer's disease (AD), two with subcortical vascular dementia, two with non-fluent variant primary progressive aphasia, one with leukoencephalopathy, one with frontotemporal dementia (FTD), and one with Creutzfeldt-Jakob disease (CJD). Five patients underwent amyloid PET: two with AD, one with mixed dementia, one with FTD, and one with CJD.
CONCLUSION
The clinical and neuropathological information to be obtained from this cohort in the future will provide a deeper understanding of the neuropathological mechanisms of cognitive impairment in Asia, especially Korea.
MeSH Terms
-
Alzheimer Disease
Amyloid
Aphasia, Primary Progressive
Asia
Brain*
Cognition Disorders
Cohort Studies
Creutzfeldt-Jakob Syndrome
Dementia
Dementia, Vascular
Diagnosis
Frontotemporal Dementia
Humans
Korea*
Leukoencephalopathies
Magnetic Resonance Imaging
Memory
Neurodegenerative Diseases
Neurologic Examination
Neuropathology
Neuropsychological Tests
Amyloid
Figure
Cited by 1 articles
-
Distinct Neural Correlates of Executive Function by Amyloid Positivity and Associations with Clinical Progression in Mild Cognitive Impairment
Hyung-Jun Yoon, Seung-Gon Kim, Sang Hoon Kim, IL Han Choo, Sang Hag Park, Eun Hyun Seo,
Yonsei Med J. 2019;60(10):935-943. doi: 10.3349/ymj.2019.60.10.935.
Reference
-
1. O'Brien RJ, Resnick SM, Zonderman AB, Ferrucci L, Crain BJ, Pletnikova O, et al. Neuropathologic studies of the Baltimore Longitudinal Study of Aging (BLSA). J Alzheimers Dis. 2009; 18:665–675. PMID: 19661626.2. Negash S, Bennett DA, Wilson RS, Schneider JA, Arnold SE. Cognition and neuropathology in aging: multidimensional perspectives from the Rush Religious Orders Study and Rush Memory And Aging Project. Curr Alzheimer Res. 2011; 8:336–340. PMID: 21222592.
Article3. Lim A, Tsuang D, Kukull W, Nochlin D, Leverenz J, McCormick W, et al. Clinico-neuropathological correlation of Alzheimer's disease in a community-based case series. J Am Geriatr Soc. 1999; 47:564–569. PMID: 10323650.
Article4. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci. 2010; 25:1071–1076. PMID: 20592901.
Article5. Kang Y, Na DL. Seoul Neuropsychological Screening Battery (SNSB). Incheon: Human Brain Research & Consulting;2003.6. Kim H, Na DL. Normative data on the Korean version of the Boston Naming Test. J Clin Exp Neuropsychol. 1999; 21:127–133. PMID: 10421007.7. Barthel H, Gertz HJ, Dresel S, Peters O, Bartenstein P, Buerger K, et al. Cerebral amyloid-β PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol. 2011; 10:424–435. PMID: 21481640.
Article8. Lee KH, Seo SW, Lim TS, Kim EJ, Kim BC, Kim Y, et al. Proposal guidelines for standardized operating procedures of brain autopsy: brain bank in South Korea. Yonsei Med J. 2017; 58:1055–1060. PMID: 28792154.
Article9. Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998; 51:1546–1554. PMID: 9855500.
Article10. Mitsuyama Y. Presenile dementia with motor neuron disease in Japan: clinico-pathological review of 26 cases. J Neurol Neurosurg Psychiatry. 1984; 47:953–959. PMID: 6481390.
Article11. Boeve BF, Lang AE, Litvan I. Corticobasal degeneration and its relationship to progressive supranuclear palsy and frontotemporal dementia. Ann Neurol. 2003; 54(Suppl 5):S15–S19. PMID: 12833363.12. Josephs KA. Frontotemporal dementia and related disorders: deciphering the enigma. Ann Neurol. 2008; 64:4–14. PMID: 18668533.
Article13. Harris JM, Gall C, Thompson JC, Richardson AM, Neary D, du Plessis D, et al. Classification and pathology of primary progressive aphasia. Neurology. 2013; 81:1832–1839. PMID: 24142474.14. Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease. Alzheimers Dement. 2012; 8:1–13. PMID: 22265587.
Article15. Thal DR, Rüb U, Orantes M, Braak H. Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology. 2002; 58:1791–1800. PMID: 12084879.16. Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Del Tredici K. Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol. 2006; 112:389–404. PMID: 16906426.
Article17. Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease: a practical approach. Acta Neuropathol. 2012; 123:1–11. PMID: 22101365.
Article18. Lee JH, Kim SH, Kim GH, Seo SW, Park HK, Oh SJ, et al. Identification of pure subcortical vascular dementia using 11C-Pittsburgh compound B. Neurology. 2011; 77:18–25. PMID: 21593437.
Article19. Kim HJ, Yang JJ, Kwon H, Kim C, Lee JM, Chun P, et al. Relative impact of amyloid-β, lacunes, and downstream imaging markers on cognitive trajectories. Brain. 2016; 139(Pt 9):2516–2527. PMID: 27329772.
Article20. Lee MJ, Seo SW, Na DL, Kim C, Park JH, Kim GH, et al. Synergistic effects of ischemia and α-amyloid burden on cognitive decline in patients with subcortical vascular mild cognitive impairment. JAMA Psychiatry. 2014; 71:412–422. PMID: 24554306.21. Noh Y, Seo SW, Jeon S, Lee JM, Kim JH, Kim GH, et al. White matter hyperintensities are associated with amyloid burden in APOE4 non-carriers. J Alzheimers Dis. 2014; 40:877–886. PMID: 24577457.
Article22. Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011; 76:1006–1014. PMID: 21325651.
Article23. Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011; 134(Pt 9):2456–2477. PMID: 21810890.24. Seo SW, Thibodeau MP, Perry DC, Hua A, Sidhu M, Sible I, et al. Early vs late age at onset frontotemporal dementia and frontotemporal lobar degeneration. Neurology. 2018; 90:e1047–e1056. PMID: 29453245.
Article25. Perry DC, Brown JA, Possin KL, Datta S, Trujillo A, Radke A, et al. Clinicopathological correlations in behavioural variant frontotemporal dementia. Brain. 2017; 140:3329–3345. PMID: 29053860.
Article26. Mesulam M. Primary progressive aphasia pathology. Ann Neurol. 2008; 63:124–125.
Article27. Knibb JA, Xuereb JH, Patterson K, Hodges JR. Clinical and pathological characterization of progressive aphasia. Ann Neurol. 2006; 59:156–165. PMID: 16374817.
Article28. Seo SW, Ayakta N, Grinberg LT, Villeneuve S, Lehmann M, Reed B, et al. Regional correlations between [11C]PIB PET and post-mortem burden of amyloid-beta pathology in a diverse neuropathological cohort. Neuroimage Clin. 2016; 13:130–137. PMID: 27981028.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on the Relationship between the Awareness of Blood Program and the Blood Donation Experience
- The Knowledge and Attitude of Medical Students towards the Organ Donation
- A Study about the Directed blood donation program
- Organ donation from donors with viral hepatitis in South Korea: a 2013–2017 nationwide data analysis
- Educational Outcomes and Perception Changes in Medical Students After Visiting a Blood Donation Center