Korean J Physiol Pharmacol.
2018 Sep;22(5):481-491. 10.4196/kjpp.2018.22.5.481.
Influence of rutin on the effects of neonatal cigarette smoke exposure-induced exacerbated MMP-9 expression, Th17 cytokines and NF-κB/iNOS-mediated inflammatory responses in asthmatic mice model
- Affiliations
-
- 1Children's Medical Center, Qilu Hospital of Shandong University, Jinan, Shandong 250012, P.R.China. lfhfuhai@hotmail.com
- 2Department of Pathology, Shandong University of Medicine, Jinan, Shandong 250012, P.R.China.
- KMID: 2418998
- DOI: http://doi.org/10.4196/kjpp.2018.22.5.481
Abstract
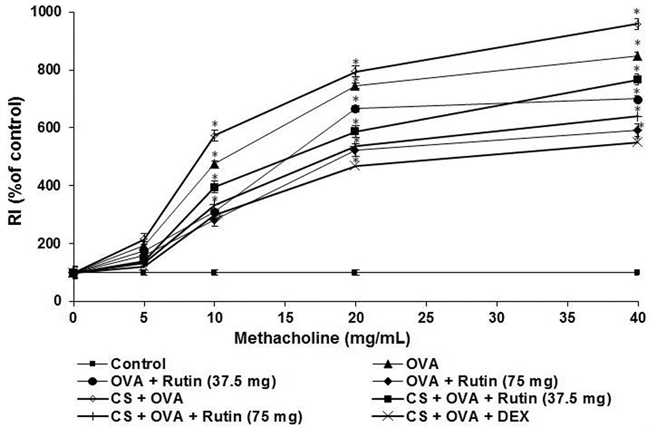
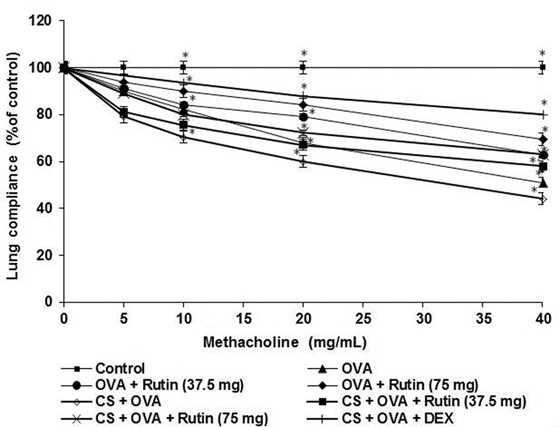
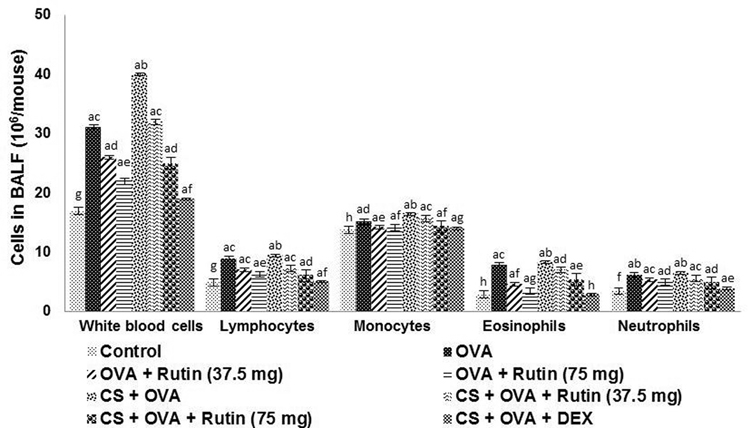
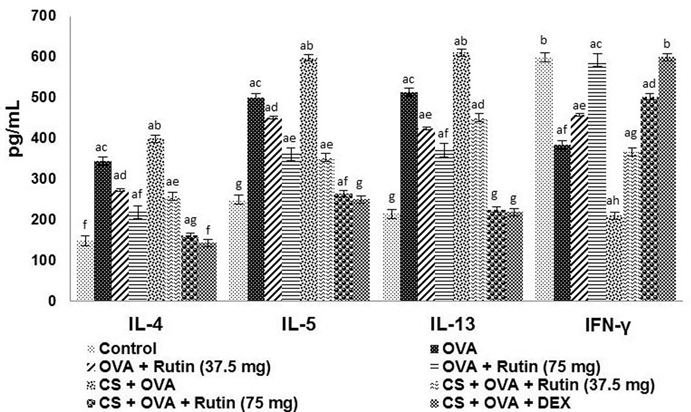
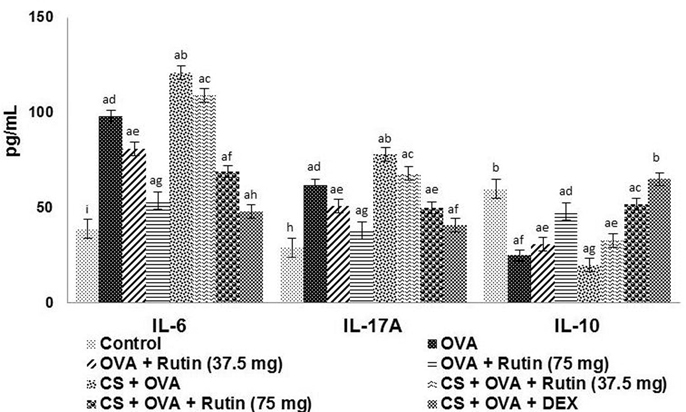
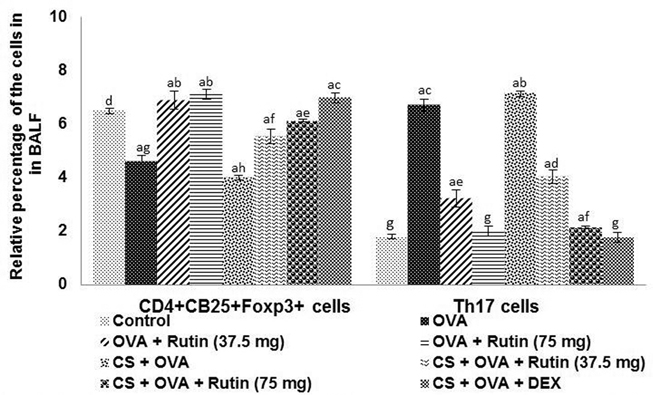
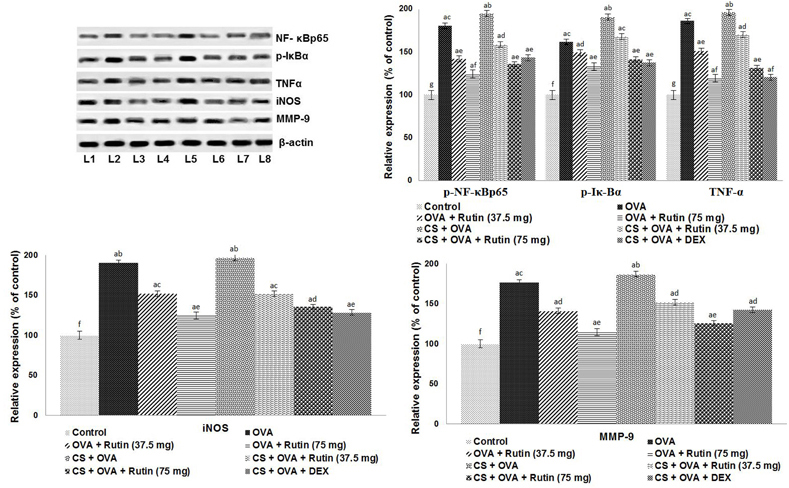
- Allergic asthma is one of the most enduring diseases of the airway. The T-helper cells and regulatory T-cells are critically involved in inflammatory responses, mucus hypersecretion, airway remodelling and in airway hyper-responsiveness. Cigarette smoke (CS) has been found to aggravate inflammatory responses in asthma. Though currently employed drugs are effective, associated side effects demand identification and development of novel drugs with negligible or no adverse effects. Rutin, plant-derived flavonoid has been found to possess antioxidant and anti-inflammatory effects. We investigated the ability of rutin to modulate T-cells and inhibit inflammation in experimentally-induced asthma in cigarette smoke exposed mice. Separate groups of neonatal mice were exposed to CS for 10 days from post-natal days 2 to 11. After 2 weeks, the mice were sensitized and challenged with ovalbumin (OVA). Treatment group were given rutin (37.5 or 75 mg/kg body weight) during OVA sensitization and challenge. Rutin treatment was found to significantly inhibit cellular infiltration in the airways and Th2 and Th17 cytokine levels as well. Flow cytometry revealed effectively raised CD4âºCD25âºFox3⺠Treg cells and supressed Th17 cell population on rutin treatment. Airway hyper-responsiveness observed following CS and OVA challenge were inhibited by rutin. NF-κB and iNOS, chief regulators of inflammatory responses robustly activated by CS and OVA were down-regulated by rutin. Rutin also inhibited the expression of matrix metalloproteinase 9, thereby aiding in prevention of airway remodelling in asthma thereby revealing to be a potent candidate in asthma therapy.
MeSH Terms
Figure
Reference
-
1. Galli SJ, Tsai M, Piliponsky AM. The development of allergic inflammation. Nature. 2008; 454:445–454.
Article2. Medoff BD, Thomas SY, Luster AD. T cell trafficking in allergic asthma: the ins and outs. Annu Rev Immunol. 2008; 26:205–232.
Article3. Bosnjak B, Stelzmueller B, Erb KJ, Epstein MM. Treatment of allergic asthma: modulation of Th2 cells and their responses. Respir Res. 2011; 12:114.
Article4. Nakajima H, Hirose K. Role of IL-23 and Th17 cells in air way inflammation in asthma. Immune Netw. 2010; 10:1–4.5. Brewer JM, Conacher M, Hunter CA, Mohrs M, Brombacher F, Alexander J. Aluminium hydroxide adjuvant initiates strong antigen-specific Th2 responses in the absence of IL-4- or IL-13-mediated signaling. J Immunol. 1999; 163:6448–6454.6. Schmidt-Weber CB, Akdis M, Akdis CA. TH17 cells in the big picture of immunology. J Allergy Clin Immunol. 2007; 120:247–254.
Article7. Sergejeva S, Ivanov S, Lötvall J, Lindén A. Interleukin-17 as a recruitment and survival factor for airway macrophages in allergic airway inflammation. Am J Respir Cell Mol Biol. 2005; 33:248–253.
Article8. Hellings PW, Kasran A, Liu Z, Vandekerckhove P, Wuyts A, Overbergh L, Mathieu C, Ceuppens JL. Interleukin-17 orchestrates the granulocyte influx into airways after allergen inhalation in a mouse model of allergic asthma. Am J Respir Cell Mol Biol. 2003; 28:42–50.
Article9. Boulet LP, Turcott H, Plante S, Chakir J. Airway function, inflammation and regulatory T cell function in subjects in asthma remission. Can Respir J. 2012; 19:19–25.
Article10. Umetsu DT, DeKruyff RH. The regulation of allergy and asthma. Immunol Rev. 2006; 212:238–255.
Article11. Sakaguchi S, Ono M, Setoguchi R, Yagi H, Hori S, Fehervari Z, Shimizu J, Takahashi T, Nomura T. Foxp3+ CD25+ CD4+ natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev. 2006; 212:8–27.12. Choi IW, Kim DK, Ko HM, Lee HK. Administration of antisense phosphorothioate oligonucleotide to the p65 subunit of NF-kappaB inhibits established asthmatic reaction in mice. Int Immunopharmacol. 2004; 4:1817–1828.13. Gagliardo R, Chanez P, Mathieu M, Bruno A, Costanzo G, Gougat C, Vachier I, Bousquet J, Bonsignore G, Vignola AM. Persistent activation of nuclear factor-kappaB signaling pathway in severe uncontrolled asthma. Am J Respir Crit Care Med. 2003; 168:1190–1198.14. Jeon WY, Shin IS, Shin HK, Lee MY. Samsoeum water extract attenuates allergic airway inflammation via modulation of Th1/Th2 cytokines and decrease of iNOS expression in asthmatic mice. BMC Complement Altern Med. 2015; 15:47.
Article15. Yoo D, Guk K, Kim H, Khang G, Wu D, Lee D. Antioxidant polymeric nanoparticles as novel therapeutics for airway inflammatory diseases. Int J Pharm. 2013; 450:87–94.
Article16. Elias JA. Airway remodeling in asthma. Unanswered questions. Am J Respir Crit Care Med. 2000; 161:S168–S171.17. Bossé M, Chakir J, Rouabhia M, Boulet LP, Audette M, Laviolette M. Serum matrix metalloproteinase-9:Tissue inhibitor of metalloproteinase-1 ratio correlates with steroid responsiveness in moderate to severe asthma. Am J Respir Crit Care Med. 1999; 159:596–602.
Article18. Tritar-Cherif F, Ben M'Rad S, Merai S, Djenayah F. Corticotherapy for asthma in the child. Tunis Med. 2002; 80:1–6.19. Kleiman A, Tuckermann JP. Glucocorticoid receptor action in beneficial and side effects of steroid therapy: lessons from conditional knockout mice. Mol Cell Endocrinol. 2007; 275:98–108.
Article20. Li XM, Brown L. Efficacy and mechanisms of action of traditional Chinese medicines for treating asthma and allergy. J Allergy Clin Immunol. 2009; 123:297–306. quiz 307–308.
Article21. Cho SJ, Kim HW, Kim BY, Cho SI. Sam So Eum, a herb extract, as the remedy for allergen-induced asthma in mice. Pulm Pharmacol Ther. 2008; 21:578–583.
Article22. Metodiewa D, Kochman A, Karolczak S. Evidence for antiradical and antioxidant properties of four biologically active N,N-diethylaminoethyl ethers of flavanone oximes: a comparison with natural polyphenolic flavonoid (rutin) action. Biochem Mol Biol Int. 1997; 41:1067–1075.23. Guardia T, Rotelli AE, Juarez AO, Pelzer LE. Anti-inflammatory properties of plant flavonoids. Effects of rutin, quercetin and hesperidin on adjuvant arthritis in rat. Farmaco. 2001; 56:683–687.
Article24. Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffmann F. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the Genetics and Environment of Asthma. Eur Respir J. 2000; 15:470–477.25. Barrett EG, Wilder JA, March TH, Espindola T, Bice DE. Cigarette smoke-induced airway hyperresponsiveness is not dependent on elevated immunoglobulin and eosinophilic inflammation in a mouse model of allergic airway disease. Am J Respir Crit Care Med. 2002; 165:1410–1418.
Article26. Wu ZX, Benders KB, Hunter DD, Dey RD. Early postnatal exposure of mice to side-steam tobacco smoke increases neuropeptide Y in lung. Am J Physiol Lung Cell Mol Physiol. 2012; 302:L152–L159.
Article27. Pinkerton KE, Joad JP. The mammalian respiratory system and critical windows of exposure for children's health. Environ Health Perspect. 2000; 108:Suppl 3. 457–462.
Article28. Oh SW, Pae CI, Lee DK, Jones F, Chiang GK, Kim HO, Moon SH, Cao B, Ogbu C, Jeong KW, Kozu G, Nakanishi H, Kahn M, Chi EY, Henderson WR Jr. Tryptase inhibition blocks airway inflammation in a mouse asthma model. J Immunol. 2002; 168:1992–2000.
Article29. Djukanović R, Roche WR, Wilson JW, Beasley CR, Twentyman OP, Howarth RH, Holgate ST. Mucosal inflammation in asthma. Am Rev Respir Dis. 1990; 142:434–457.
Article30. Jain VV, Kitagaki K, Businga T, Hussain I, George C, O'shaughnessy P, Kline JN. CpG-oligodeoxynucleotides inhibit airway remodeling in a murine model of chronic asthma. J Allergy Clin Immunol. 2002; 110:867–872.
Article31. Pichavant M, Goya S, Hamelmann E, Gelfand EW, Umetsu DT. Animal models of airway sensitization. Curr Protoc Immunol. 2007; Chapter 15:Unit 15.18.
Article32. Glaab T, Daser A, Braun A, Neuhaus-Steinmetz U, Fabel H, Alarie Y, Renz H. Tidal midexpiratory flow as a measure of airway hyperresponsiveness in allergic mice. Am J Physiol Lung Cell Mol Physiol. 2001; 280:L565–L573.
Article33. Bao Z, Guan S, Cheng C, Wu S, Wong SH, Kemeny DM, Leung BP, Wong WS. A novel antiinflammatory role for andrographolide in asthma via inhibition of the nuclear factor-kappaB pathway. Am J Respir Crit Care Med. 2009; 179:657–665.34. Duan W, Chan JH, Wong CH, Leung BP, Wong WS. Anti-inflammatory effects of mitogen-activated protein kinase kinase inhibitor U0126 in an asthma mouse model. J Immunol. 2004; 172:7053–7059.
Article35. Lee YC, Lee HB, Rhee YK, Song CH. The involvement of matrix metalloproteinase-9 in airway inflammation of patients with acute asthma. Clin Exp Allergy. 2001; 31:1623–1630.
Article36. Busse WW, Lemanske RF Jr. Asthma. N Engl J Med. 2001; 344:350–362.
Article37. Moerloose KB, Robays LJ, Maes T, Brusselle GG, Tournoy KG, Joos GF. Cigarette smoke exposure facilitates allergic sensitization in mice. Respir Res. 2006; 7:49–57.
Article38. Yang SR, Chida AS, Bauter MR, Shafiq N, Seweryniak K, Maggirwar SB, Kilty I, Rahman I. Cigarette smoke induces proinflammatory cytokine release by activation of NF-kappaB and posttranslational modifications of histone deacetylase in macrophages. Am J Physiol Lung Cell Mol Physiol. 2006; 291:L46–L57.39. Elsner J, Kapp A. Regulation and modulation of eosinophil effector functions. Allergy. 1999; 54:15–26.
Article40. Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet. 2006; 368:804–813.
Article41. Li J, Zhang B. Apigenin protects ovalbumin-induced asthma through the regulation of Th17 cells. Fitoterapia. 2013; 91:298–304.
Article42. Simon D, Braathen LR, Simon HU. Eosinophils and atopic dermatitis. Allergy. 2004; 59:561–570.
Article43. Kolls JK, Lindén A. Interleukin-17 family members and inflammation. Immunity. 2004; 21:467–476.
Article44. Cockcroft DW, Davis BE. Mechanisms of airway hyperresponsiveness. J Allergy Clin Immunol. 2006; 118:551–559. quiz 560–561.
Article45. Royer B, Varadaradjalou S, Saas P, Guillosson JJ, Kantelip JP, Arock M. Inhibition of IgE-induced activation of human mast cells by IL-10. Clin Exp Allergy. 2001; 31:694–704.
Article46. Nembrini C, Marsland BJ, Kopf M. IL-17-producing T cells in lung immunity and inflammation. J Allergy Clin Immunol. 2009; 123:986–994. quiz 995–996.
Article47. Siebenlist U, Brown K, Claudio E. Control of lymphocyte development by nuclear factor-kappaB. Nat Rev Immunol. 2005; 5:435–445.48. Rahman MS, Yamasaki A, Yang J, Shan L, Halayko AJ, Gounni AS. IL-17A induces eotaxin-1/CC chemokine ligand 11 expression in human airway smooth muscle cells: role of MAPK (Erk1/2, JNK, and p38) pathways. J Immunol. 2006; 177:4064–4071.
Article49. Suresh V, Mih JD, George SC. Measurement of IL-13-induced iNOS-derived gas phase nitric oxide in human bronchial epithelial cells. Am J Respir Cell Mol Biol. 2007; 37:97–104.
Article50. Grzela K, Zagorska W, Krejner A, Litwiniuk M, Zawadzka-Krajewska A, Banaszkiewicz A, Kulus M, Grzela T. Prolonged treatment with inhaled corticosteroids does not normalize high activity of matrix metalloproteinase-9 in exhaled breath condensates of children with asthma. Arch Immunol Ther Exp (Warsz). 2015; 63:231–237.
Article51. Mehra D, Sternberg DI, Jia Y, Canfield S, Lemaitre V, Nkyimbeng T, Wilder J, Sonett J, D'Armiento J. Altered lymphocyte trafficking and diminished airway reactivity in transgenic mice expressing human MMP-9 in a mouse model of asthma. Am J Physiol Lung Cell Mol Physiol. 2010; 298:L189–L196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-inflammatory effects of rutin in lipopolysaccharide-stimulated canine macrophage cells
- Anti-inflammatory activities of Scolopendra subspinipes mutilans in RAW 264.7 cells
- Effect of Transcription Factor Decoy for NF-κB on the TNF-α Induced Cytokine and ICAM-1 Expression in Cultured HaCaT cells
- Lipopolysaccharide induces neuroglia activation and NF-κB activation in cerebral cortex of adult mice
- Anti-Inflammatory Activities of (+)-Afzelechin against Lipopolysaccharide-Induced Inflammation