Yonsei Med J.
2011 Mar;52(2):351-357. 10.3349/ymj.2011.52.2.351.
The Characteristics of Metallo-beta-Lactamase-Producing Gram-Negative Bacilli Isolated from Sputum and Urine: A Single Center Experience in Korea
- Affiliations
-
- 1AIDS Research Institute and Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. jmkim@yuhs.ac
- 2Research Institute of Bacterial Resistance and Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1779675
- DOI: http://doi.org/10.3349/ymj.2011.52.2.351
Abstract
- Metallo-beta-lactamase (MBL) production usually results in high-level resistance to most beta-lactams, and a rapid spread of MBL producing major gram-negative pathogens is a matter of particular concern worldwide. However, clinical data are scarce and most studies compared MBL producer (MP) with MBL non-producer (MNP) strains which included carbapenem susceptible isolates. Therefore, we collected clinical data of patients in whom imipenem-nonsusceptible Pseudomonas aeruginosa (PA) and Acinetobacter baumannii (AB) were isolated from sputum or urine, and investigated MBL production and the risk factors related with MBL acquisition. The antimicrobial susceptibility patterns were also compared between MPs and imipenem-nonsusceptible MNPs (INMNP). Among the 176 imipenem-nonsusceptible isolates, 12 MPs (6.8%) were identified. There was no identifiable risk factor that contributed to the acquisition of MPs when compared to INMNPs, and case-fatalities were not different between the two groups. The percentage of susceptible isolates was higher among MPs for piperacilin/tazobactam and fluoroquinolones while that of ceftazidime was higher in INMNPs (p < 0.05). As regards to aztreonam, which has been known to be a uniquely stable beta-lactam against MBLs, susceptibility was preserved in only two isolates (16.7%) among MPs, and was not higher than that of INMNPs (23.2%). In conclusion, the contribution of MBLs to imipenem non-susceptibility in PA/ABs isolated from sputum and urine was relatively limited, and there was no significant risk factor associated with acquisition of MPs compared with INMNPs. However, limited susceptibility to aztreonam implies that MPs may hold additional resistance mechanisms, such as extended spectrum beta-lactamases, AmpC beta-lactamases, or other non-enzymatic mechanisms.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Anti-Bacterial Agents/pharmacology/therapeutic use
Child
Child, Preschool
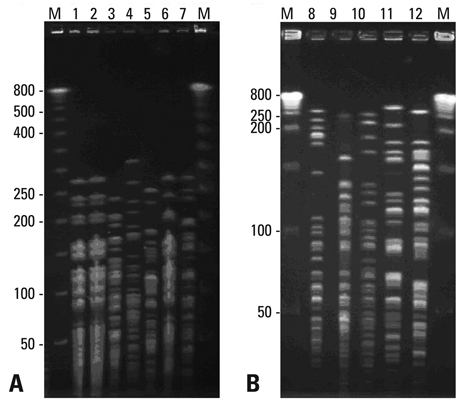
Electrophoresis, Gel, Pulsed-Field
Female
Gram-Negative Bacteria/drug effects/*enzymology/isolation & purification
Gram-Negative Bacterial Infections/drug therapy/enzymology/microbiology
Humans
Male
Microbial Sensitivity Tests
Middle Aged
Republic of Korea
Sputum/*microbiology
Urine/*microbiology
beta-Lactam Resistance
beta-Lactamases/*metabolism
Figure
Cited by 1 articles
-
Clinical Outcomes of Tigecycline in the Treatment of Multidrug-Resistant Acinetobacter baumannii Infection
Jung Ar Shin, Yoon Soo Chang, Hyung Jung Kim, Se Kyu Kim, Joon Chang, Chul Min Ahn, Min Kwang Byun
Yonsei Med J. 2012;53(5):974-984. doi: 10.3349/ymj.2012.53.5.974.
Reference
-
1. Cornaglia G, Akova M, Amicosante G, Cantón R, Cauda R, Docquier JD, et al. Metallo-beta-lactamases as emerging resistance determinants in Gram-negative pathogens: open issues. Int J Antimicrob Agents. 2007. 29:380–388.
Article2. Zavascki AP, Barth AL, Gonçalves AL, Moro AL, Fernandes JF, Martins AF, et al. The influence of metallo-beta-lactamase production on mortality in nosocomial Pseudomonas aeruginosa infections. J Antimicrob Chemother. 2006. 58:387–392.
Article3. Zavascki AP, Barth AL, Gaspareto PB, Gonçalves AL, Moro AL, Fernandes JF, et al. Risk factors for nosocomial infections due to Pseudomonas aeruginosa producing metallo-beta-lactamase in two tertiary-care teaching hospitals. J Antimicrob Chemother. 2006. 58:882–885.
Article4. Hirakata Y, Yamaguchi T, Nakano M, Izumikawa K, Mine M, Aoki S, et al. Clinical and bacteriological characteristics of IMP-type metallo-beta-lactamase-producing Pseudomonas aeruginosa. Clin Infect Dis. 2003. 37:26–32.
Article5. Zavascki AP, Barth AL, Fernandes JF, Moro AL, Gonçalves AL, Goldani LZ. Reappraisal of Pseudomonas aeruginosa hospital-acquired pneumonia mortality in the era of metallo-beta-lactamase-mediated multidrug resistance: a prospective observational study. Crit Care. 2006. 10:R114.6. Lautenbach E, Weiner MG, Nachamkin I, Bilker WB, Sheridan A, Fishman NO. Imipenem resistance among pseudomonas aeruginosa isolates: risk factors for infection and impact of resistance on clinical and economic outcomes. Infect Control Hosp Epidemiol. 2006. 27:893–900.
Article7. Kwon KT, Oh WS, Song JH, Chang HH, Jung SI, Kim SW, et al. Impact of imipenem resistance on mortality in patients with Acinetobacter bacteraemia. J Antimicrob Chemother. 2007. 59:525–530.
Article8. Murray EJ, Baron EJ, Pfaller MA, Tenover FC, Yolken RH. Manual of clinical microbiology. 1999. 7th ed. Washington DC: ASM Press;442–458.9. CLSI document M100-S19. Performance standards for antimicrobial susceptibiliy testing; Nineteenth Informational Supplement. 2009.10. Lee K, Lim YS, Yong D, Yum JH, Chong Y. Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-beta-lactamase-producing isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2003. 41:4623–4629.
Article11. Lee K, Yum JH, Yong D, Lee HM, Kim HD, Docquier JD, et al. Novel acquired metallo-beta-lactamase gene, bla(SIM-1), in a class 1 integron from Acinetobacter baumannii clinical isolates from Korea. Antimicrob Agents Chemother. 2005. 49:4485–4491.
Article12. Lee K, Ha GY, Shin BM, Kim JJ, Kang JO, Jang SJ, et al. Metallo-beta-lactamase-producing Gram-negative bacilli in Korean Nationwide Surveillance of Antimicrobial Resistance group hospitals in 2003: continued prevalence of VIM-producing Pseudomonas spp. and increase of IMP-producing Acinetobacter spp. Diagn Microbiol Infect Dis. 2004. 50:51–58.
Article13. Nouér SA, Nucci M, de-Oliveira MP, Pellegrino FL, Moreira BM. Risk factors for acquisition of multidrug-resistant Pseudomonas aeruginosa producing SPM metallo-beta-lactamase. Antimicrob Agents Chemother. 2005. 49:3663–3667.
Article14. Kim YA, Choi JY, Kim CK, Kim CO, Kim MS, Choi SH, et al. Risk factors and outcomes of bloodstream infections with metallo-beta-lactamase-producing Acinetobacter. Scand J Infect Dis. 2008. 40:234–240.
Article15. Horianopoulou M, Legakis NJ, Kanellopoulou M, Lambropoulos S, Tsakris A, Falagas ME. Frequency and predictors of colonization of the respiratory tract by VIM-2-producing Pseudomonas aeruginosa in patients of a newly established intensive care unit. J Med Microbiol. 2006. 55:1435–1439.
Article16. Laupland KB, Parkins MD, Church DL, Gregson DB, Louie TJ, Conly JM, et al. Population-based epidemiological study of infections caused by carbapenem-resistant Pseudomonas aeruginosa in the Calgary Health Region: importance of metallo-beta-lactamase (MBL)-producing strains. J Infect Dis. 2005. 192:1606–1612.
Article17. Daikos GL, Petrikkos P, Psichogiou M, Kosmidis C, Vryonis E, Skoutelis A, et al. Prospective observational study of the impact of VIM-1 metallo-beta-lactamase on the outcome of patients with Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2009. 53:1868–1873.18. Huang YT, Chang SC, Lauderdale TL, Yang AJ, Wang JT. Molecular epidemiology of carbapenem-resistant Pseudomonas aeruginosa carrying metallo-beta-lactamase genes in Taiwan. Diagn Microbiol Infect Dis. 2007. 59:211–216.19. Doi Y, Ghilardi AC, Adams J, de Oliveira Garcia D, Paterson DL. High prevalence of metallo-beta-lactamase and 16S rRNA methylase coproduction among imipenem-resistant Pseudomonas aeruginosa isolates in Brazil. Antimicrob Agents Chemother. 2007. 51:3388–3390.20. Pasteran F, Faccone D, Petroni A, Rapoport M, Galas M, Vázquez M, et al. Novel variant (bla(VIM-11)) of the metallo-{beta}-lactamase bla(VIM) family in a GES-1 extended-spectrum-{beta}-lactamase-producing Pseudomonas aeruginosa clinical isolate in Argentina. Antimicrob Agents Chemother. 2005. 49:474–475.
Article21. Yong D, Shin JH, Kim S, Lim Y, Yum JH, Lee K, et al. High prevalence of PER-1 extended-spectrum-beta-lactamase-producing Acinetobacter spp. in Korea. Antimicrob Agents Chemother. 2003. 47:1749–1751.
Article22. Segal H, Nelson EC, Elisha BG. Genetic environment and transcription of ampC in an Acinetobacter baumannii clinical isolate. Antimicrob Agents Chemother. 2004. 48:612–614.
Article23. Cavallo JD, Fabre R, Leblanc F, Nicolas-Chanoine MH, Thabaut A. Group d'Etude de la Résistance de Pseudomonas aeruginosa aux Bêtalactamines. Antibiotic susceptibility and mechanisms of beta-lactam resistance in 1310 strains of pseudomonas aeruginosa: a French multicentre study (1996). J Antimicrob Chemother. 2000. 46:133–136.
Article24. Corvec S, Caroff N, Espaze E, Giraudeau C, Drugeon H, Reynaud A. AmpC cephalosporinase hyperproduction in Acinetobacter baumannii clinical strains. J Antimicrob Chemother. 2003. 52:629–635.
Article25. Peleg AY, Franklin C, Bell JM, Spelman DW. Dissemination of the metallo-beta-lactamase gene blaIMP-4 among gram-negative pathogens in a clinical setting in Australia. Clin Infect Dis. 2005. 41:1549–1556.
Article26. Fukigai S, Alba J, Kimura S, Iida T, Nishikura N, Ishii Y, et al. Nosocomial outbreak of genetically related IMP-1 beta-lactamase-producing Klebsiella pneumoniae in a general hospital in Japan. Int J Antimicrob Agents. 2007. 29:306–310.
Article27. Lee K, Kim MN, Choi TY, Cho SE, Lee S, Whang DH, et al. Wide dissemination of OXA-type carbapenemases in clinical Acinetobacter spp. isolates from South Korea. Int J Antimicrob Agents. 2009. 33:520–524.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metallo-beta-lactamase Producing Gram-negative Bacilli
- Increasing Carbapenem-Resistant Gram-Negative Bacilli and Decreasing Metallo-beta-Lactamase Producers over Eight Years from Korea
- VIM-2 Type Metallo-beta-lactamase Producing Achromobacter xylosoxidans subsp. xylosoxidans Isolated from Urine Specimens
- Epidemiology and Characteristics of Metallo-beta-Lactamase-Producing Pseudomonas aeruginosa
- Emergence of Acinetobacter pittii Harboring New Delhi Metallo-beta-Lactamase Genes in Daejeon, Korea