J Neurocrit Care.
2018 Jun;11(1):1-6. 10.18700/jnc.180049.
Antibiotics Induced Seizures and Encephalopathy
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea. zhau@yuhs.ac
- KMID: 2426207
- DOI: http://doi.org/10.18700/jnc.180049
Abstract
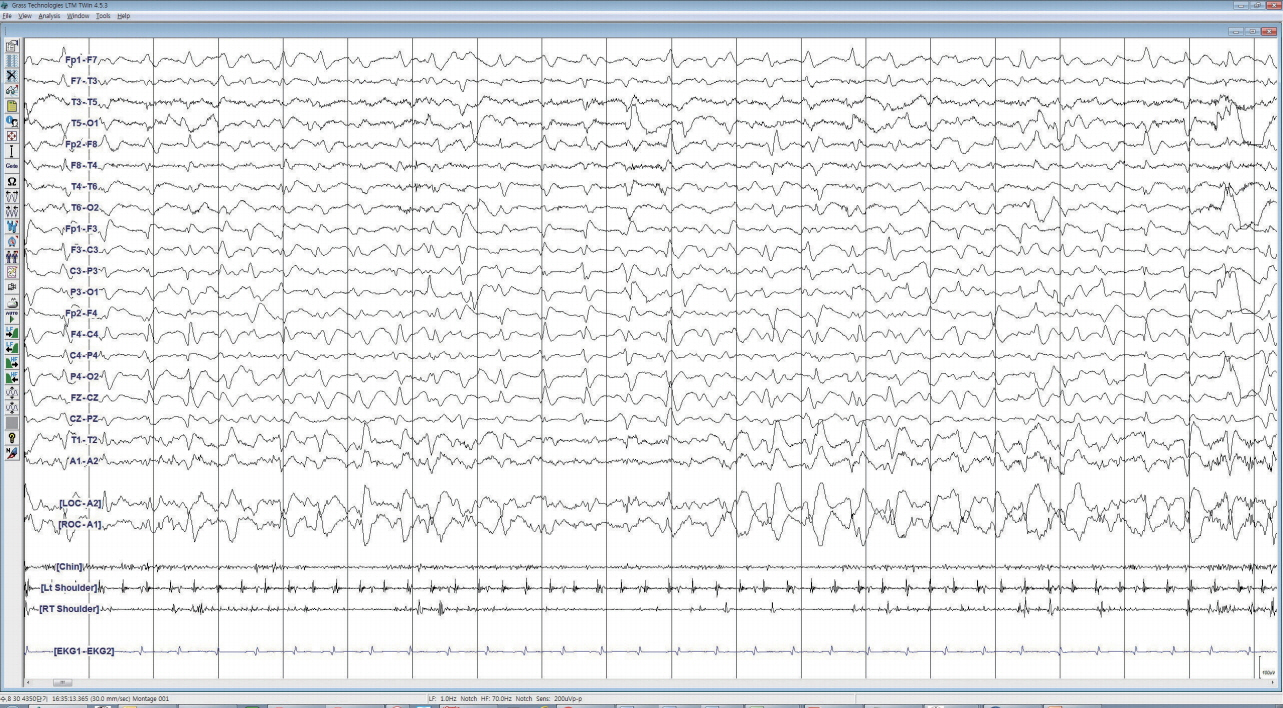
- Drug-induced seizures and delirium are common among patients with critical illnesses, especially those in an intensive care unit. With an increase in the use of potent, broad-spectrum antibiotics, the etiology for encephalopathy remains under-recognized. Antibiotics-induced nonconvulsive seizures should also be considered in patients with unexplained mental status, therefore continuous electroencephalography monitoring is often needed for its detection. Prompt discontinuation, substitution, or dose adjustment of the causative antibiotics might help improve prognosis. Also, antibiotics should be used with caution especially in patients with known epilepsy, central nervous system disorders, critical illnesses, or renal dysfunction.
MeSH Terms
Figure
Cited by 1 articles
-
Cefepime-induced neurotoxicity
Se-Jin Lee
J Neurocrit Care. 2019;12(2):74-84. doi: 10.18700/jnc.190109.
Reference
-
1. Chen R, Young GB. Metabolic encephalopathies. Bailleres Clin Neurol. 1996; 5:577–98.2. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014; 383:911–22.
Article3. Alagiakrishnan K, Wiens CA. An approach to drug induced delirium in the elderly. Postgrad Med J. 2004; 80:388–93.
Article4. Pesola GR, Avasarala J. Bupropion seizure proportion among new-onset generalized seizures and drug related seizures presenting to an emergency department. J Emerg Med. 2002; 22:235–9.
Article5. Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999; 340:669–76.
Article6. Young GB, Jordan KG, Doig GS. An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality. Neurology. 1996; 47:83–9.7. Martens E, Demain AL. The antibiotic resistance crisis, with a focus on the United States. J Antibiot (Tokyo). 2017; 70:520–6.
Article8. Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010; 23:858–83.
Article9. Sonneville R, Verdonk F, Rauturier C, Klein IF, Wolff M, Annane D, et al. Understanding brain dysfunction in sepsis. Ann Intensive Care. 2013; 3:15.
Article10. Bhattacharyya S, Darby RR, Raibagkar P, Gonzalez Castro LN, Berkowitz AL. Antibiotic-associated encephalopathy. Neurology. 2016; 86:963–71.
Article11. Reuling JR, Cramer C. Intrathecal penicillin. J Am Med Assoc. 1947; 134:16–8.
Article12. Weinstein L, Lerner PI, Chew WH. Clinical and bacteriologic studies of the effect of "massive" doses of penicillin g on infections caused by gram-negative bacilli. N Engl J Med. 1964; 271:525–33.
Article13. Conway N, Beck E, Somerville J. Penicillin encephalopathy. Postgrad Med J. 1968; 44:891–7.
Article14. Teresa Ravizza SB, Nicola Marchi. Experimental models of inflammation in epilepsy research. In : Asla Pitkanen PSB, Galanopoulou Aristea S., Moshe Solomon L., editors. Models of seizures and epilepsy. 2nd ed. London: Academic Press;p. 2017–965.15. Gutnick MJ, Prince DA. Penicillinase and the convulsant action of penicillin. Neurology. 1971; 21:759–64.
Article16. Davidoff RA. Penicillin and inhibition in the cat spinal cord. Brain Res. 1972; 45:638–42.
Article17. Dingledine R, Gjerstad L. Penicillin blocks hippocampal IPSPs, unmasking prolonged EPSPs. Brain Res. 1979; 168:205–9.
Article18. Wong RK, Prince DA. Dendritic mechanisms underlying penicillin-induced epileptiform activity. Science. 1979; 204:1228–31.
Article19. Lindquist CE, Dalziel JE, Cromer BA, Birnir B. Penicillin blocks human alpha 1 beta 1 and alpha 1 beta 1 gamma 2S GABAA channels that open spontaneously. Eur J Pharmacol. 2004; 496:23–32.20. Sutter R, Rüegg S, Tschudin-Sutter S. Seizures as adverse events of antibiotic drugs: a systematic review. Neurology. 2015; 85:1332–41.21. Papp-Wallace KM, Endimiani A, Taracila MA, Bonomo RA. Carbapenems: past, present, and future. Antimicrob Agents Chemother. 2011; 55:4943–60.
Article22. Cannon JP, Lee TA, Clark NM, Setlak P, Grim SA. The risk of seizures among the carbapenems: a meta-analysis. J Antimicrob Chemother. 2014; 69:2043–55.
Article23. Rodloff AC, Goldstein EJ, Torres A. Two decades of imipenem therapy. J Antimicrob Chemother. 2006; 58:916–29.
Article24. Horiuchi M, Kimura M, Tokumura M, Hasebe N, Arai T, Abe K. Absence of convulsive liability of doripenem, a new carbapenem antibiotic, in comparison with beta-lactam antibiotics. Toxicology. 2006; 222:114–24.25. Miller AD, Ball AM, Bookstaver PB, Dornblaser EK, Bennett CL. Epileptogenic potential of carbapenem agents: mechanism of action, seizure rates, and clinical considerations. Pharmacotherapy. 2011; 31:408–23.
Article26. Mancl EE, Gidal BE. The effect of carbapenem antibiotics on plasma concentrations of valproic acid. Ann Pharmacother. 2009; 43:2082–7.
Article27. Fernández-Torre JL, Martínez-Martínez M, González-Rato J, Maestro I, Alonso I, Rodrigo E, et al. Cephalosporin-induced nonconvulsive status epilepticus: clinical and electroencephalographic features. Epilepsia. 2005; 46:1550–2.28. Sugimoto M, Fukami S, Kayakiri H, Yamazaki S, Matsuoka N, Uchida I, et al. The beta-lactam antibiotics, penicillin-G and cefoselis have different mechanisms and sites of action at GABA(A) receptors. Br J Pharmacol. 2002; 135:427–32.29. Alkharfy KM, Kellum JA, Frye RF, Matzke GR. Effect of ceftazidime on systemic cytokine concentrations in rats. Antimicrob Agents Chemother. 2000; 44:3217–9.
Article30. Grill MF, Maganti R. Cephalosporin-induced neurotoxicity: clinical manifestations, potential pathogenic mechanisms, and the role of electroencephalographic monitoring. Ann Pharmacother. 2008; 42:1843–50.
Article31. Sugimoto M, Uchida I, Mashimo T, Yamazaki S, Hatano K, Ikeda F, et al. Evidence for the involvement of GABA(A) receptor blockade in convulsions induced by cephalosporins. Neuropharmacology. 2003; 45:304–14.
Article32. Moore TD, Bechtel TP, Ayers LW. Effect of multidose therapy on cerebrospinal fluid penetration of cefazolin. Am J Hosp Pharm. 1981; 38:1496–9.
Article33. Fugate JE, Kalimullah EA, Hocker SE, Clark SL, Wijdicks EF, Rabinstein AA. Cefepime neurotoxicity in the intensive care unit: a cause of severe, underappreciated encephalopathy. Crit Care. 2013; 17:R264.
Article34. Fernández-Torre JL. Levofloxacin-induced delirium: diagnostic considerations. Clin Neurol Neurosurg. 2006; 108:614.
Article35. Schmuck G, Schürmann A, Schlüter G. Determination of the excitatory potencies of fluoroquinolones in the central nervous system by an in vitro model. Antimicrob Agents Chemother. 1998; 42:1831–6.
Article36. Thomas RJ, Reagan DR. Association of a tourette-like syndrome with ofloxacin. Ann Pharmacother. 1996; 30:138–41.
Article37. Rao DN, Mason RP. Generation of nitro radical anions of some 5-nitrofurans, 2- and 5-nitroimidazoles by norepinephrine, dopamine, and serotonin. A possible mechanism for neurotoxicity caused by nitroheterocyclic drugs. J Biol Chem. 1987; 262:11731–6.
Article38. Alston TA, Abeles RH. Enzymatic conversion of the antibiotic metronidazole to an analog of thiamine. Arch Biochem Biophys. 1987; 257:357–62.
Article39. Kim E, Na DG, Kim EY, Kim JH, Son KR, Chang KH. MR imaging of metronidazole-induced encephalopathy: lesion distribution and diffusion-weighted imaging findings. AJNR Am J Neuroradiol. 2007; 28:1652–8.
Article40. Grill MF, Maganti RK. Neurotoxic effects associated with antibiotic use: management considerations. Br J Clin Pharmacol. 2011; 72:381–93.
Article41. Naeije G, Depondt C, Meeus C, Korpak K, Pepersack T, Legros B. EEG patterns compatible with nonconvulsive status epilepticus are common in elderly patients with delirium: a prospective study with continuous EEG monitoring. Epilepsy Behav. 2014; 36:18–21.
Article42. Sutter R, Semmlack S, Kaplan PW. Nonconvulsive status epilepticus in adults - insights into the invisible. Nat Rev Neurol. 2016; 12:281–93.
Article43. Maganti R, Jolin D, Rishi D, Biswas A. Nonconvulsive status epilepticus due to cefepime in a patient with normal renal function. Epilepsy Behav. 2006; 8:312–4.
Article44. Johnson E, Carballido Martinez N, Ritzl E. Cefepime-related encephalopathy and associated EEG activity (P6.369). Neurology. 2016; 86.45. Johnson E, Martinez NC, Ritzl E. Cefepime-related encephalopathy and associated EEG activity (P6.369). Neurology. 2016; 86(16 Suppl):6.369.46. Wallace KL. Antibiotic-induced convulsions. Crit Care Clin. 1997; 13:741–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cisplatin-Induced Encephalopathy With Status Epilepticus
- Cefepime Induced Encephalopathy Mimicking Acute Stroke
- Ischemic Encephalothy Found Accidentally in Children Diagnosed as Febrile Seizures
- A case of valproic acid-induced hyperammonemic encephalopathy with normal liver function
- A case of metronidazole induced encephalopathy in a cirrhotic patient