Accuracy of three different fecal calprotectin tests in the diagnosis of inflammatory bowel disease
- Affiliations
-
- 1Department of Internal Medicine, Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea. geniushee@yuhs.ac
- 2Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2354948
- DOI: http://doi.org/10.5217/ir.2016.14.4.305
Abstract
- BACKGROUND/AIMS
Several studies have found that the measurement of fecal calprotectin is useful for the early diagnosis of inflammatory bowel disease (IBD). We compared the effectiveness of three different fecal calprotectin kits for initial diagnosis in patients with suspected IBD.
METHODS
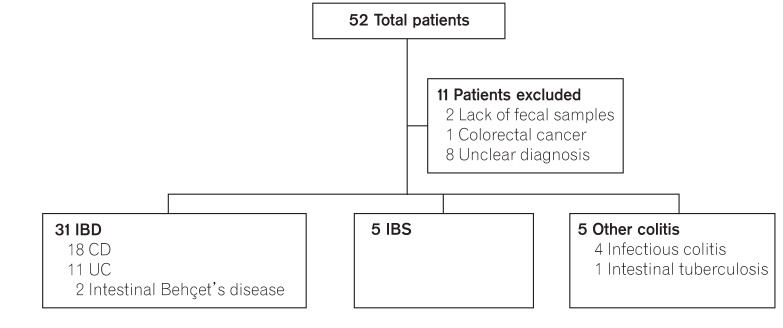
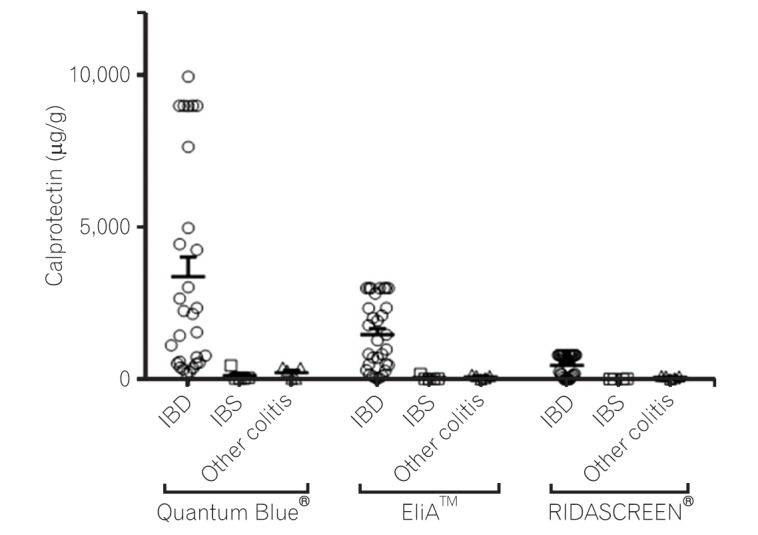
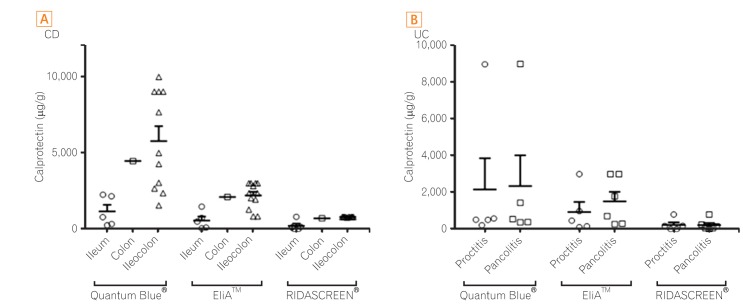
We enrolled 31 patients with IBD (18 Crohn's disease [CD], 11 ulcerative colitis [UC], and two intestinal Behçet's disease), five with irritable bowel syndrome (IBS), and five with other colitis (four infectious colitis and one intestinal tuberculosis). Diagnosis was based on clinical, laboratory, and endoscopic examinations. Fecal samples were obtained at the first diagnosis and calprotectin levels were measured using three different kits (Quantum Blue® Calprotectin, EliAâ„¢ Calprotectin, and RIDASCREEN® Calprotectin).
RESULTS
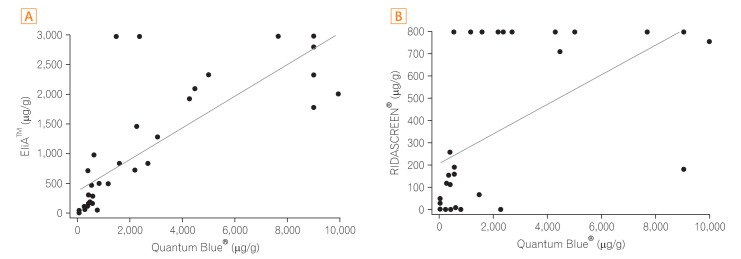
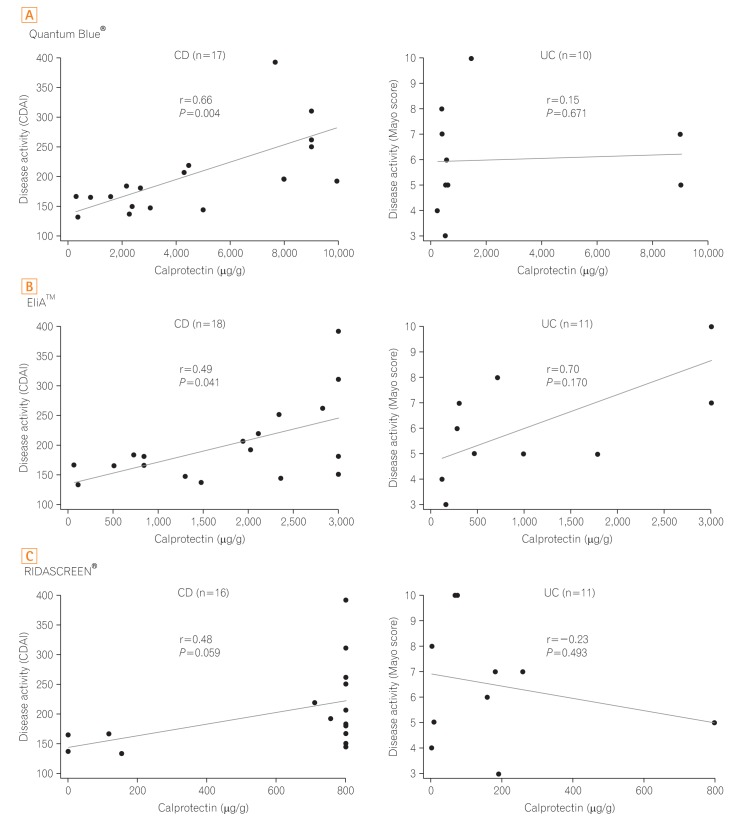
The overall accuracy for differentiating IBD from IBS or other colitis was 94% and 91%, respectively, for Quantum Blue® (cutoff, 50 µg/g); 92% and 89%, respectively, for EliAâ„¢ (cutoff, 50 µg/g); and 82% and 76%, respectively, for RIDASCREEN® (cutoff, 50 µg/g). In patients with CD, the results of Quantum Blue® Calprotectin and EliAâ„¢ Calprotectin correlated significantly with levels of the Crohn's disease activity index (Spearman's rank correlation coefficient, r=0.66 and r=0.49, respectively). In patients with UC, the results of EliAâ„¢ Calprotectin correlated significantly with the Mayo score (r=0.70).
CONCLUSIONS
Fecal calprotectin measurement is useful for the identification of IBD. The overall accuracies of the three fecal calprotectin kits are comparable.
MeSH Terms
Figure
Cited by 3 articles
-
The role of platelet to lymphocyte ratio and neutrophil to lymphocyte ratio in ulcerative colitis
Yujin Jeong, Seong Ran Jeon, Hyun Gun Kim, Jung Rock Moon, Tae Hee Lee, Jae Young Jang, Jun-Hyung Cho, Jun Seok Park, Heesu Park, Ki-hun Lee, Jin-Oh Kim, Joon Seong Lee, Bong Min Ko, Suyeon Park
Intest Res. 2021;19(1):62-70. doi: 10.5217/ir.2019.09156.Experience of patients with inflammatory bowel disease in using a home fecal calprotectin test as an objective reported outcome for self-monitoring
Shu-Chen Wei, Chien-Chih Tung, Meng-Tzu Weng, Jau-Min Wong
Intest Res. 2018;16(4):546-553. doi: 10.5217/ir.2018.00052.Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease?
Shu Chen Wei
Intest Res. 2016;14(4):293-294. doi: 10.5217/ir.2016.14.4.293.
Reference
-
1. Hsu K, Champaiboon C, Guenther BD, et al. Anti-infective protective properties of S100 calgranulins. Antiinflamm Antiallergy Agents Med Chem. 2009; 8:290–305. PMID: 20523765.
Article2. Tibble J, Teahon K, Thjodleifsson B, et al. A simple method for assessing intestinal inflammation in Crohn's disease. Gut. 2000; 47:506–513. PMID: 10986210.
Article3. Tibble JA, Sigthorsson G, Foster R, Forgacs I, Bjarnason I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology. 2002; 123:450–460. PMID: 12145798.
Article4. von Roon AC, Karamountzos L, Purkayastha S, et al. Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am J Gastroenterol. 2007; 102:803–813. PMID: 17324124.
Article5. Gisbert JP, McNicholl AG. Questions and answers on the role of faecal calprotectin as a biological marker in inflammatory bowel disease. Dig Liver Dis. 2009; 41:56–66. PMID: 18602356.
Article6. van Rheenen PF, Van de Vijver E, Fidler V. Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: diagnostic meta-analysis. BMJ. 2010; 341:c3369. PMID: 20634346.
Article7. Lee KM. Fecal biomarkers in inflammatory bowel disease. Intest Res. 2013; 11:73–78.
Article8. Røseth AG, Aadland E, Grzyb K. Normalization of faecal calprotectin: a predictor of mucosal healing in patients with inflammatory bowel disease. Scand J Gastroenterol. 2004; 39:1017–1020. PMID: 15513345.
Article9. Wagner M, Peterson CG, Stolt I, et al. Fecal eosinophil cationic protein as a marker of active disease and treatment outcome in collagenous colitis: a pilot study. Scand J Gastroenterol. 2011; 46:849–854. PMID: 21557718.
Article10. Sipponen T, Savilahti E, Kärkkäinen P, et al. Fecal calprotectin, lactoferrin, and endoscopic disease activity in monitoring anti-TNF-alpha therapy for Crohn's disease. Inflamm Bowel Dis. 2008; 14:1392–1398. PMID: 18484671.
Article11. De Vos M, Dewit O, D'Haens G, et al. Fast and sharp decrease in calprotectin predicts remission by infliximab in anti-TNF naïve patients with ulcerative colitis. J Crohns Colitis. 2012; 6:557–562. PMID: 22398050.
Article12. Molander P, af Björkesten CG, Mustonen H, et al. Fecal calprotectin concentration predicts outcome in inflammatory bowel disease after induction therapy with TNF alpha blocking agents. Inflamm Bowel Dis. 2012; 18:2011–2017. PMID: 22223566.
Article13. Hämäläinen A, Sipponen T, Kolho KL. Infliximab in pediatric inflammatory bowel disease rapidly decreases fecal calprotectin levels. World J Gastroenterol. 2011; 17:5166–5171. PMID: 22215940.
Article14. Ho GT, Lee HM, Brydon G, et al. Fecal calprotectin predicts the clinical course of acute severe ulcerative colitis. Am J Gastroenterol. 2009; 104:673–678. PMID: 19262524.
Article15. Gisbert JP, Bermejo F, Pérez-Calle JL, et al. Fecal calprotectin and lactoferrin for the prediction of inflammatory bowel disease relapse. Inflamm Bowel Dis. 2009; 15:1190–1198. PMID: 19291780.
Article16. Costa F, Mumolo MG, Ceccarelli L, et al. Calprotectin is a stronger predictive marker of relapse in ulcerative colitis than in Crohn's disease. Gut. 2005; 54:364–368. PMID: 15710984.
Article17. D'Incà R, Dal Pont E, Di Leo V, et al. Can calprotectin predict relapse risk in inflammatory bowel disease? Am J Gastroenterol. 2008; 103:2007–2014. PMID: 18802997.18. Kallel L, Ayadi I, Matri S, et al. Fecal calprotectin is a predictive marker of relapse in Crohn's disease involving the colon: a prospective study. Eur J Gastroenterol Hepatol. 2010; 22:340–345. PMID: 19581809.
Article19. Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: current management. J Crohns Colitis. 2010; 4:28–62. PMID: 21122489.
Article20. Dignass A, Lindsay JO, Sturm A, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012; 6:991–1030. PMID: 23040451.
Article21. Coorevits L, Baert FJ, Vanpoucke HJ. Faecal calprotectin: comparative study of the Quantum Blue rapid test and an established ELISA method. Clin Chem Lab Med. 2013; 51:825–831. PMID: 23001318.
Article22. Oyaert M, Trouvé C, Baert F, De Smet D, Langlois M, Vanpoucke H. Comparison of two immunoassays for measurement of faecal calprotectin in detection of inflammatory bowel disease: (pre)-analytical and diagnostic performance characteristics. Clin Chem Lab Med. 2014; 52:391–397. PMID: 24114912.
Article23. Fagerhol MK, Dale I, Anderson T. Release and quantitation of a leucocyte derived protein (L1). Scand J Haematol. 1980; 24:393–398.
Article24. Mirsepasi-Lauridsen HC, Bachmann Holmetoft U, Ingdam Halkjær S, Angeliki Krogfelt K, Munk Petersen A. Comparison of three commercial fecal calprotectin ELISA test kits used in patients with inflammatory bowel disease. Scand J Gastroenterol. 2016; 51:211–217. PMID: 26359672.
Article25. Labaere D, Smismans A, Van Olmen A, et al. Comparison of six different calprotectin assays for the assessment of inflammatory bowel disease. United European Gastroenterol J. 2014; 2:30–37.
Article26. Schoepfer AM, Trummler M, Seeholzer P, Criblez DH, Seibold F. Accuracy of four fecal assays in the diagnosis of colitis. Dis Colon Rectum. 2007; 50:1697–1706. PMID: 17762964.
Article27. Costa F, Mumolo MG, Bellini M, et al. Role of faecal calprotectin as non-invasive marker of intestinal inflammation. Dig Liver Dis. 2003; 35:642–647. PMID: 14563186.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fecal Calprotectin in Inflammatory Bowel Disease
- The role of fecal calprotectin in pediatric disease
- Combination of leucine-rich alpha-2 glycoprotein and fecal markers detect Crohn’s disease activity confirmed by balloon-assisted enteroscopy
- Usefulness of fecal immunochemical test and fecal calprotectin for detection of active ulcerative colitis
- Could fecal calprotectin enter mainstream use for diagnosing and monitoring inflammatory bowel disease?