Tuberc Respir Dis.
2010 Apr;68(4):226-230.
Bicalutamide-induced Interstitial Lung Disease
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, East-West Neo Medical Center, Kyung Hee University School of Medicine, Seoul, Korea. yeehyung@gmail.com
- 2Department of Hematology and Oncology, East-West Neo Medical Center, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Department of Pulmonary and Critical Care Medicine, Kyung Hee University Medical Center, Kyung Hee University School of Medicine, Seoul, Korea.
Abstract
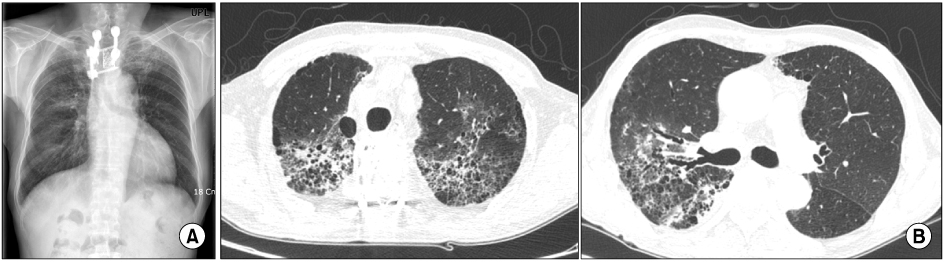
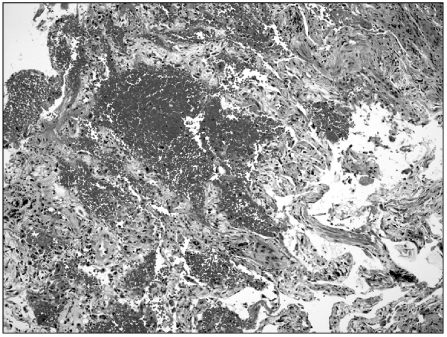
- Androgen deprivation therapy, which is the standard treatment for metastatic prostate cancer, includes nonsteroidal antiandrogenic drugs, such as flutamide, nilutamide and bicalutamide. Of them, bicalutamide rarely induces interstitial pneumonia. We report a case of bicalutamide-induced interstitial pneumonia. A 68-year old male diagnosed with prostate cancer and multiple bone metastases presented with dry cough and low grade fever for 3 days. He had taken bicalutamide (50 mg/day) for 13 months. High resolution computed tomography revealed ground glass opacity in his right upper lung. The laboratory studies showed no eosinophilia in the serum and bronchoalveolar lavage fluid. Despite the use of antimicrobial agents for 2 weeks, the extent of the lung lesions increased to the left upper and right lower lung. He had no environmental exposure, collagen vascular disease and microbiological causes. Under the suspicion of bicalutamide-induced interstitial pneumonia, bicalutamide was stopped and prednisolone (1 mg/kg/day) was initiated. The symptoms and radiologic abnormalities were resolved with residual minimal fibrosis.
MeSH Terms
-
Anilides
Anti-Infective Agents
Bronchoalveolar Lavage Fluid
Collagen
Cough
Environmental Exposure
Eosinophilia
Fever
Fibrosis
Flutamide
Glass
Humans
Imidazolidines
Lung
Lung Diseases, Interstitial
Male
Neoplasm Metastasis
Nitriles
Prednisolone
Prostatic Neoplasms
Tosyl Compounds
Vascular Diseases
Anilides
Anti-Infective Agents
Collagen
Flutamide
Imidazolidines
Nitriles
Prednisolone
Tosyl Compounds
Figure
Reference
-
1. Camus P, Fanton A, Bonniaud P, Camus C, Foucher P. Interstitial lung disease induced by drugs and radiation. Respiration. 2004. 71:301–326.2. Pfitzenmeyer P, Foucher P, Piard F, Coudert B, Braud ML, Gabez P, et al. Nilutamide pneumonitis: a report on eight patients. Thorax. 1992. 47:622–627.3. Azuma T, Kurimoto S, Mikami K, Oshi M. Interstitial pneumonitis related to leuprorelin acetate and flutamide. J Urol. 1999. 161:221.4. Shioi K, Sakai N, Yoshida M, Nakamura M. Successful recovery from interstitial pneumonitis, induced by bicalutamide and leuprorelin acetate given as treatment for prostate cancer. Hinyokika Kiyo. 2005. 51:211–214.5. Shioi K, Yoshida M, Sakai N. Interstitial pneumonitis induced by bicalutamide and leuprorelin acetate for prostate cancer. Int J Urol. 2003. 10:625–626.6. Mayaud C, Fartoukh M, Parrot A, Cadranel J, Milleron B, Akoun G. Drug-associated interstitial lung disease: a diagnostic challenge. Rev Pneumol Clin. 2005. 61:179–185.7. Ben-Noun L. Drug-induced respiratory disorders: incidence, prevention and management. Drug Saf. 2000. 23:143–164.8. Ellis SJ, Cleverley JR, Muller NL. Drug-induced lung disease: high-resolution CT findings. AJR Am J Roentgenol. 2000. 175:1019–1024.9. Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics, 1999. CA Cancer J Clin. 1999. 49:8–31.10. Dahele M, Brade A, Pearson S, Bezjak A. Stereotactic radiation therapy for inoperable, early-stage non-small-cell lung cancer. CMAJ. 2009. 180:1326–1328.11. Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee DH, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005. 235:208–215.12. Koenig TR, Munden RF, Erasmus JJ, Sabloff BS, Gladish GW, Komaki R, et al. Radiation injury of the lung after three-dimensional conformal radiation therapy. AJR Am J Roentgenol. 2002. 178:1383–1388.13. Ikezoe J, Takashima S, Morimoto S, Kadowaki K, Takeuchi N, Yamamoto T, et al. CT appearance of acute radiation-induced injury in the lung. AJR Am J Roentgenol. 1988. 150:765–770.14. Cleverley JR, Screaton NJ, Hiorns MP, Flint JD, Muller NL. Drug-induced lung disease: high-resolution CT and histological findings. Clin Radiol. 2002. 57:292–299.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Cancers in a Patient with Systemic Sclerosis and Aggravated Interstitial Lung Disease by Chemotherapy
- Carbamazepine-induced Acute Interstitial Lung Disease
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Reversible Lansoprazole-Induced Interstitial Lung Disease Showing Improvement after Drug Cessation
- Interstitial Lung Diseases: Respiratory Review of 2013