Korean J Radiol.
2008 Apr;9(2):175-178. 10.3348/kjr.2008.9.2.175.
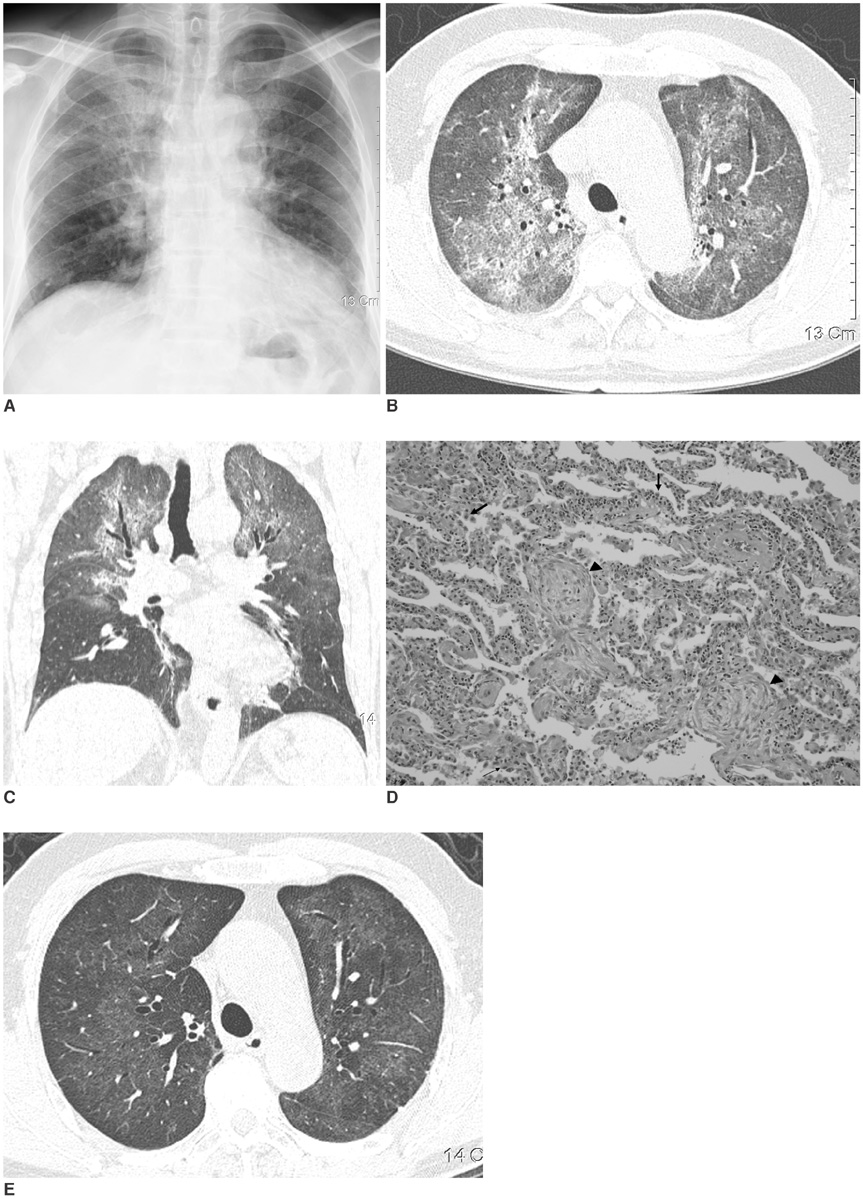
Reversible Lansoprazole-Induced Interstitial Lung Disease Showing Improvement after Drug Cessation
- Affiliations
-
- 1Department of Radiology, College of Medicine, Korea University, Guro Hospital, Seoul, Korea. wokhee@unitel.co.kr
- 2Department of Pathology, College of Medicine, Korea University, Guro Hospital, Seoul, Korea.
- 3Department of Internal Medicine, College of Medicine, Korea University, Guro Hospital, Seoul, Korea.
- KMID: 1098197
- DOI: http://doi.org/10.3348/kjr.2008.9.2.175
Abstract
- Lansoprazole is an acid proton-pump inhibiting drug that is used for the treatment of duodenal or gastric ulcers, H. pylori infection, gastroesophageal reflux disease or Zollinger-Ellison syndrome. Although lansoprazole is well known for its gastrointestinal and dermatologic adverse effects, mild pulmonary symptoms are also known to develop from taking this drug. There have been no reports about lansoprazole-induced interstitial lung disease. We report here a case of lansoprazole-induced interstitial lung disease that developed in a 66-year-old man.
MeSH Terms
Figure
Reference
-
1. Pietra GG. Pathologic mechanism of drug-induced lung disorders. J Thorac Imaging. 1991. 6(1):1–7.2. Kohno S, Yamaguchi K, Yasuoka A, Koga H, Hayashi T, Komori K, et al. Clinical evaluation of 12 cases of antimicrobial drug-induced pneumonitis. Jpn J Med. 1990. 29:248–254.3. Akira M, Ishikawa H, Yamamoto S. Drug-induced pneumonitis: thin-section CT findings in 60 patients. Radiology. 2002. 224:852–860.4. Rossi SE, Erasmus JJ, McAdams HP, Sporn TA, Goodman PC. Pulmonary drug toxicity: radiologic and pathologic manifestation. Radiographics. 2000. 20:1245–1259.5. Cleverley JR, Screaton NJ, Hiorns MP, Flint JD, Muller NL. Drug-induced lung disease: high-resolution CT and histologic findings. Clin Radiol. 2002. 57:292–299.6. Fraser RS, Muller NL, Colman N, Pare PD. Fraser & Pare: Diagnosis of disease of the chest. 1999. 4th ed. Philadelphia: Saunders;2537–2540.