Ann Dermatol.
2010 May;22(2):206-208. 10.5021/ad.2010.22.2.206.
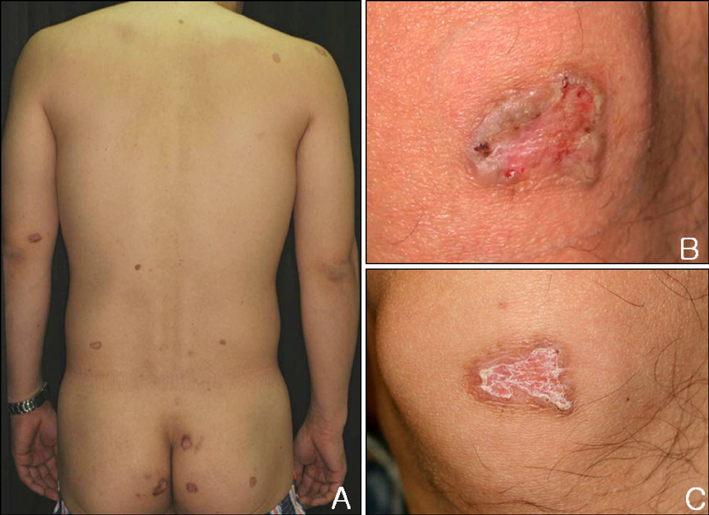
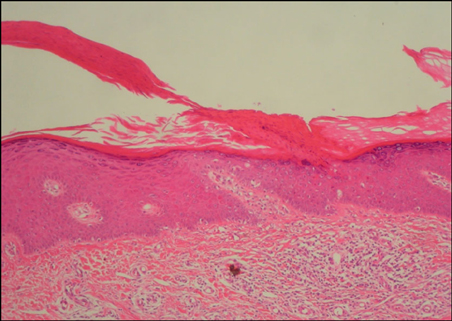
Atypical Porokeratosis Developing Following Bone Marrow Transplantation in a Patient with Myelodysplastic Syndrome
- Affiliations
-
- 1Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea. derm@catholic.ac.kr
- KMID: 2265396
- DOI: http://doi.org/10.5021/ad.2010.22.2.206
Abstract
- Porokeratosis is an abnormal disease of keratinization of epidermis. It is clinically characterized by margins covered with keratin layer and it typically has an atrophied macule with a protruded, circular form. Histopathologically, it shows the findings of cornoid lamella. Risk factors for its development include organ transplantation, long-term use of corticosteroids, immunocompromised status, including AIDS, and exposure to ultraviolet light. We herein report a case of atypical porokeratosis in a 38-year-old man who developed porokeratosis involving multiple sites following bone marrow transplantation for myelodysplastic syndrome.
MeSH Terms
Figure
Reference
-
1. Schamroth JM, Zlotogorski A, Gilead L. Porokeratosis of Mibelli. Overview and review of the literature. Acta Derm Venereol. 1997. 77:207–213.2. Alexis AF, Busam K, Myskowski PL. Porokeratosis of Mibelli following bone marrow transplantation. Int J Dermatol. 2006. 45:361–365.
Article3. Levin RM, Heymann WR. Superficial disseminate porokeratosis in a patient with myelodysplastic syndrome. Int J Dermatol. 1999. 38:138–139.
Article4. Herranz P, Pizarro A, De Lucas R, Robayna MG, Rubio FA, Sanz A, et al. High incidence of porokeratosis in renal transplant recipients. Br J Dermatol. 1997. 136:176–179.
Article5. Lederman JS, Sober AJ, Lederman GS. Immunosuppression: a cause of porokeratosis? J Am Acad Dermatol. 1985. 13:75–79.
Article6. Rio B, Magana C, Le Tourneau A, Bachmeyer C, Levy V, Hamont N, et al. Disseminated superficial porokeratosis after autologous bone marrow transplantation. Bone Marrow Transplant. 1997. 19:77–79.
Article7. Gilead L, Guberman D, Zlotogorski A, Vardy DA, Klaus SN. Immunosuppression-induced porokeratosis of Mibelli: complete regression of lesions upon cessation of immunosuppressive therapy. J Eur Acad Dermatol Venereol. 1995. 5:170–172.
Article8. Raychaudhuri SP, Smoller BR. Porokeratosis in immunosuppressed and nonimmunosuppressed patients. Int J Dermatol. 1992. 31:781–782.
Article9. Ghigliotti G, Nigro A, Gambini C, Farris A, Burroni A, de Marchi R. Mibelli's porokeratosis after bone marrow transplantation. Ann Dermatol Venereol. 1992. 119:968–970.10. Manganoni AM, Facchetti F, Gavazzoni R. Involvement of epidermal Langerhans cells in porokeratosis of immunosuppressed renal transplant recipients. J Am Acad Dermatol. 1989. 21:799–801.
Article11. Anzai S, Takeo N, Yamaguchi T, Sato T, Takasaki S, Terashi H, et al. Squamous cell carcinoma in a renal transplant recipient with linear porokeratosis. J Dermatol. 1999. 26:244–247.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Exacerbation of Porokeratosis with Myelodysplastic Syndrome
- A Case of Leukemia Cutis in Myelodysplastic Syndrome Evolving into An Atypical Chronic Myeloid Leukemia
- Evans Syndrome following T Cell-repleted Unrelated Bone Marrow Transplantation for Myelodysplastic Syndrome: Successful Response to High-dose Corticosteroid
- Myelodysplastic Syndrome in a Renal Transplant Recipient Treated with Long-term Azathioprine
- A Case of Histiocytoid Sweet's Syndrome with Myelodysplastic Syndrome