Allergy Asthma Immunol Res.
2013 May;5(3):175-178. 10.4168/aair.2013.5.3.175.
Improvement of Eosinophilic Otitis Media by Optimized Asthma Treatment
- Affiliations
-
- 1Department of Otolaryngology, Tokyo Women's Medical University School of Medicine, Tokyo, Japan. nonaka-m@oto.twmu.ac.jp
- 2First Department of Medicine, Tokyo Women's Medical University School of Medicine, Tokyo, Japan.
- 3Division of Allergy, Department of Pediatrics, Nippon Medical School, Tokyo, Japan.
- KMID: 2260338
- DOI: http://doi.org/10.4168/aair.2013.5.3.175
Abstract
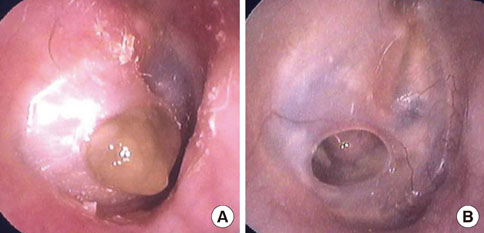
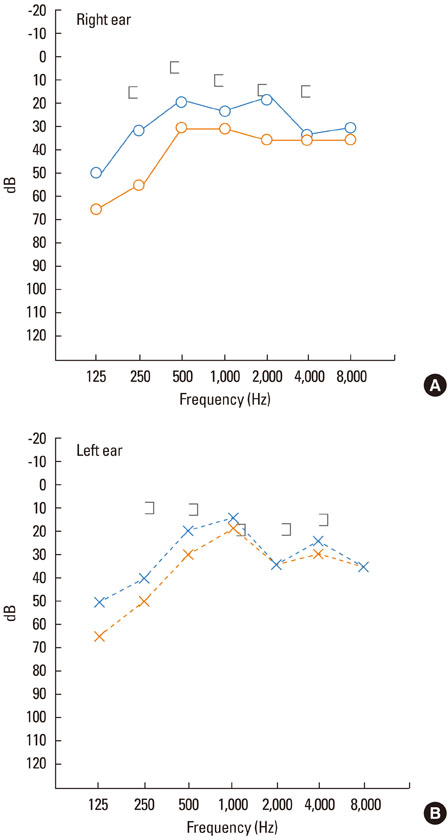
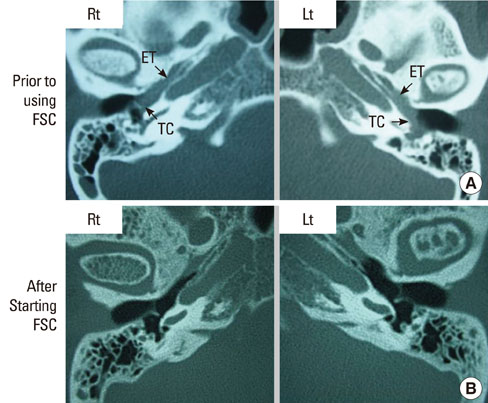
- Eosinophilic otitis media (EOM) shows a very high rate of association with asthma, and intractable otitis media involves marked eosinophil infiltration into the middle ear. The middle ear space is connected to the nasopharynx by the Eustachian tube, and it is considered a part of the upper respiratory tract. Allergic rhinitis and asthma often coexist as chronic inflammatory diseases of the upper and lower airways, respectively, and have an impact on each other. In fact, inhaled corticosteroids reduce seasonal eosinophilia systemically in the circulation and locally in the nasal mucosa, as well as attenuate seasonal nasal symptoms. We report a case of EOM associated with adult-onset asthma that improved following optimal asthma therapy after changing the treatment from inhaled fluticasone propionate (FP) (200 microg b.i.d.) to a combination of FP/salmeterol (250/50 microg b.i.d.). This result supports the hypothesis that EOM and asthma are closely linked, presenting as different manifestations of a similar disease syndrome.
MeSH Terms
Figure
Cited by 1 articles
-
Optimal control of asthma improved eosinophilic otitis media
Yukako Seo, Manabu Nonaka, Yukie Yamamura, Ruby Pawankar, Etsuko Tagaya
Asia Pac Allergy. 2018;8(1):. doi: 10.5415/apallergy.2018.8.e5.
Reference
-
1. Iino Y, Tomioka-Matsutani S, Matsubara A, Nakagawa T, Nonaka M. Diagnostic criteria of eosinophilic otitis media, a newly recognized middle ear disease. Auris Nasus Larynx. 2011. 38:456–461.2. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O'Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D. World Health Organization. GA(2)LEN. AllerGen. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008. 63:Suppl 86. 8–160.3. Pawankar R. Allergic rhinitis and asthma: are they manifestations of one syndrome? Clin Exp Allergy. 2006. 36:1–4.4. Braunstahl GJ, Hellings PW. Allergic rhinitis and asthma: the link further unraveled. Curr Opin Pulm Med. 2003. 9:46–51.5. Tomioka S, Yuasa R, Iino Y. Mogi G, Honjo I, Ishii T, Takasaka T, editors. Intractable otitis media in cases with bronchial asthma. Recent advances in otitis media. Proceedings of the second extraordinary international symposium on recent advances in otitis media. 1993. Amsterdam, New York: Kugler Publications;183–186.6. Iino Y, Kakizaki K, Katano H, Saigusa H, Kanegasaki S. Eosinophil chemoattractants in the middle ear of patients with eosinophilic otitis media. Clin Exp Allergy. 2005. 35:1370–1376.7. Hellings PW, Hessel EM, Van Den Oord JJ, Kasran A, Van Hecke P, Ceuppens JL. Eosinophilic rhinitis accompanies the development of lower airway inflammation and hyper-reactivity in sensitized mice exposed to aerosolized allergen. Clin Exp Allergy. 2001. 31:782–790.8. Wang J, Palmer K, Lŏtvall J, Milan S, Lei XF, Matthaei KI, Gauldie J, Inman MD, Jordana M, Xing Z. Circulating, but not local lung, IL-5 is required for the development of antigen-induced airways eosinophilia. J Clin Invest. 1998. 102:1132–1141.9. Braunstahl GJ, Kleinjan A, Overbeek SE, Prins JB, Hoogsteden HC, Fokkens WJ. Segmental bronchial provocation induces nasal inflammation in allergic rhinitis patients. Am J Respir Crit Care Med. 2000. 161:2051–2057.10. Braunstahl GJ, Overbeek SE, Fokkens WJ, Kleinjan A, McEuen AR, Walls AF, Hoogsteden HC, Prins JB. Segmental bronchoprovocation in allergic rhinitis patients affects mast cell and basophil numbers in nasal and bronchial mucosa. Am J Respir Crit Care Med. 2001. 164:858–865.11. Beeh KM, Beier J, Kornmann O, Meier C, Taeumer T, Buhl R. A single nasal allergen challenge increases induced sputum inflammatory markers in non-asthmatic subjects with seasonal allergic rhinitis: correlation with plasma interleukin-5. Clin Exp Allergy. 2003. 33:475–482.12. Greiff L, Andersson M, Svensson C, Linden M, Wollmer P, Brattsand R, Persson CG. Effects of orally inhaled budesonide in seasonal allergic rhinitis. Eur Respir J. 1998. 11:1268–1273.13. Barnes PJ, Pedersen S. Efficacy and safety of inhaled corticosteroids in asthma. Report of a workshop held in Eze, France, October 1992. Am Rev Respir Dis. 1993. 148:S1–S26.14. Chapman KR, Ringdal N, Backer V, Palmqvist M, Saarelainen S, Briggs M. Salmeterol and fluticasone propionate (50/250 microg) administered via combination Diskus inhaler: as effective as when given via separate Diskus inhalers. Can Respir J. 1999. 6:45–51.15. Barnes PJ. Scientific rationale for inhaled combination therapy with long-acting beta2-agonists and corticosteroids. Eur Respir J. 2002. 19:182–191.16. Iino Y, Nagamine H, Kakizaki K, Komiya T, Katano H, Saruya S, Kodera K. Effectiveness of instillation of triamcinolone acetonide into the middle ear for eosinophilic otitis media associated with bronchial asthma. Ann Allergy Asthma Immunol. 2006. 97:761–766.