J Korean Endocr Soc.
2009 Sep;24(3):212-216. 10.3803/jkes.2009.24.3.212.
A Case of Osteomalacia with Multiple Fractures and Hypocalcemia Associated with Phenytoin Therapy
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Ajou University School of Medicine, Korea.
- 2Department of Radiology, Ajou University School of Medicine, Korea.
- 3Department of Neurology, Ajou University School of Medicine, Korea.
- 4Department of Orthopedic Surgery, Ajou University School of Medicine, Korea.
- KMID: 2178185
- DOI: http://doi.org/10.3803/jkes.2009.24.3.212
Abstract
- Many studies have shown that patients taking antiepileptic drugs are at an increased risk for metabolic bone disease and low bone mineral density. Traditionally, this has been attributed to alterations in vitamin D metabolism by antiepileptic drugs which induce hepatic microsomal cytochrome P450 enzyme. However, there appear to be multiple mechanisms for antiepileptic drug-induced bone loss including lack of physical activity, reduced sunlight exposure, increased propensity for falling, and fractures associated with seizures or loss of consciousness. We experienced a case of antiepileptic drug-induced osteomalacia in a 63-year-old woman who had been on phenytoin for 8 years and was admitted with hypocalcemic seizures and multiple pathological fractures. This patient also had other risk factors for osteomalacia including reduced sunlight exposure, prolonged immobilization, and decreased dietary vitamin D intake. We discontinued phenytoin, and started calcium and vitamin D replacement. The patient's serum calcium and vitamin D level were normalized after treatment. Metabolic bone disease including osteomalacia should be considered in patients who are taking antiepileptic drugs especially those who are exposed to other risk factors.
Keyword
MeSH Terms
-
Anticonvulsants
Bone Density
Bone Diseases, Metabolic
Calcium
Cytochrome P-450 Enzyme System
Female
Fractures, Spontaneous
Humans
Hypocalcemia
Immobilization
Middle Aged
Motor Activity
Osteomalacia
Phenytoin
Risk Factors
Seizures
Sunlight
Unconsciousness
Vitamin D
Anticonvulsants
Calcium
Cytochrome P-450 Enzyme System
Phenytoin
Vitamin D
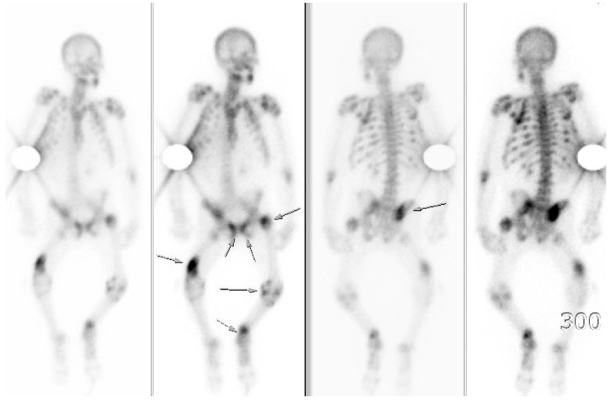
Figure
Reference
-
1. Frame B, Parfitt AM. Osteomalacia: current concepts. Ann Intern Med. 1978. 89:966–982.2. Schmid F. Osteopathien bei antiepileptischer Dauerbehandlung. Fortschr Med. 1967. 85:381–382.3. Kruse R. Osteopathies in antiepileptic long-term therapy (preliminary report). Monatsschr Kinderheilkd. 1968. 116:378–381.4. Valmadrid C, Voorhees C, Litt B, Schneyer CR. Practice patterns of neurologists regarding bone and mineral effects of antiepileptic drug therapy. Arch Neurol. 2001. 58:1369–1374.5. Hoikka V, Savolainen K, Alhava EM, Sivenius J, Karjalainen P, Parvianinen M. Anticonvulsant osteomalacia in epileptic outpatients. Ann Clin Res. 1982. 14:129–132.6. Sato Y, Kondo I, Ishida S, Motooka H, Takayama K, Tomita Y, Maeda H, Satoh K. Decreased bone mass and increased bone turnover with valproate therapy in adults with epilepsy. Neurology. 2001. 57:445–449.7. Andress DL, Ozuna J, Tirschwell D, Grande L, Johnson M, Jacobson AF, Spain W. Antiepileptic drug-induced bone loss in young male patients who have seizures. Arch Neurol. 2002. 59:781–786.8. Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995. 332:767–773.9. van Staa TP, Leufkens HG, Cooper C. Utility of medical and drug history in fracture risk prediction among men and women. Bone. 2002. 31:508–514.10. Weinstein RS, Bryce GF, Sappington LJ, King DW, Gallagher BB. Decreased serum ionized calcium and normal vitamin D metabolite levels with anticonvulsant drug treatment. J Clin Endocrinol Metab. 1984. 58:1003–1009.11. Babayigit A, Dirik E, Bober E, Cakmakci H. Adverse effects of antiepileptic drugs on bone mineral density. Pediatr Neurol. 2006. 35:177–181.12. Fitzpatrick LA. Pathophysiology of bone loss in patients receiving anticonvulsant therapy. Epilepsy Behav. 2004. 5:S3–S15.13. Gough H, Bissesar A, Goggin T, Higgins D, Baker M, Crowley M, Callaghan N. Factors associated with the biochemical changes in vitamin D and calcium metabolism in institutionalized patients with epilepsy. Ir J Med Sci. 1986. 155:181–189.14. Fogelman I, Gray JM, Gardner MD, Beastall GH, McIntosh WB, Allam BF, Boyce BF, Boyle IT, Lawson DH. Do anticonvulsant drugs commonly induce osteomalacia? Scott Med J. 1982. 27:136–142.15. Cho YW, Lee IK, Hur SH. Adverse effects of antiepileptic drugs on bone mineral density in women with epilepsy. J Korean Endocr Soc. 2002. 17:218–225.16. Suh YS, Kim YG, Lee JH, Yoo KH, Lee JW, Tockgo YC. The effect of long-term phenobarbital administration on the bone mineral density of children. J Korean Pediatr Soc. 1994. 37:368–375.17. Heller HJ, Sakhaee K. Anticonvulsant-induced bone disease: a plea for monitoring and treatment. Arch Neurol. 2001. 58:1352–1353.18. Drezner MK. Treatment of anticonvulsant drug-induced bone disease. Epilepsy Behav. 2004. 5:S41–S47.19. Toss G, Andersson R, Diffey BL, Fall PA, Larkö O, Larsson L. Oral vitamin D and ultraviolet radiation for the prevention of vitamin D deficiency in the elderly. Acta Med Scand. 1982. 212:157–161.20. Williams C, Netzloff M, Folkerts L, Vargas A, Garnica A, Frias J. Vitamin D metabolism and anticonvulsant therapy: effect of sunshine on incidence of osteomalacia. South Med J. 1984. 77:834–836.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oncogenic Osteomalacia with Multiple Insufficiency Fractures: A Case Report
- A Case of Osteomalacia with Long Term Carbamazepine Therapy
- Dilated Cardiomyopathy in a 2 Month-Old Infant: A Severe Form of Hypocalcemia With Vitamin D Deficient Rickets
- Generalized Cutaneous Pseudolymphoma Associated with Phenytoin Therapy
- Hypophosphatemic Osteomalacia with Multiple Bone Fractures: ADV-Induced Fanconi's Syndrome