J Korean Fract Soc.
2017 Jul;30(3):146-150. 10.12671/jkfs.2017.30.3.146.
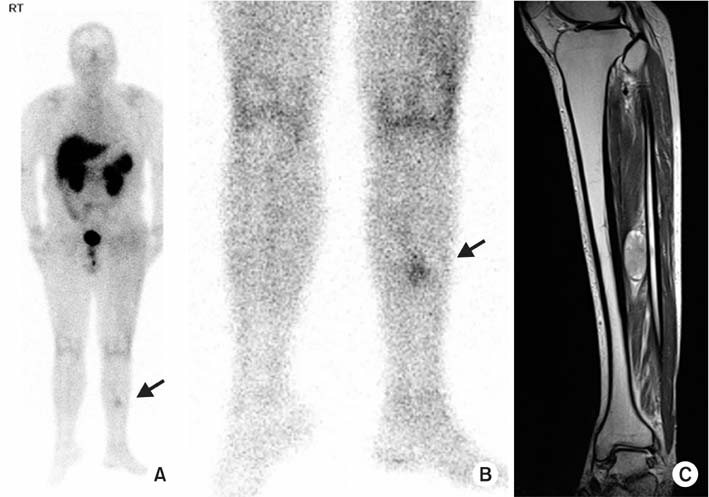
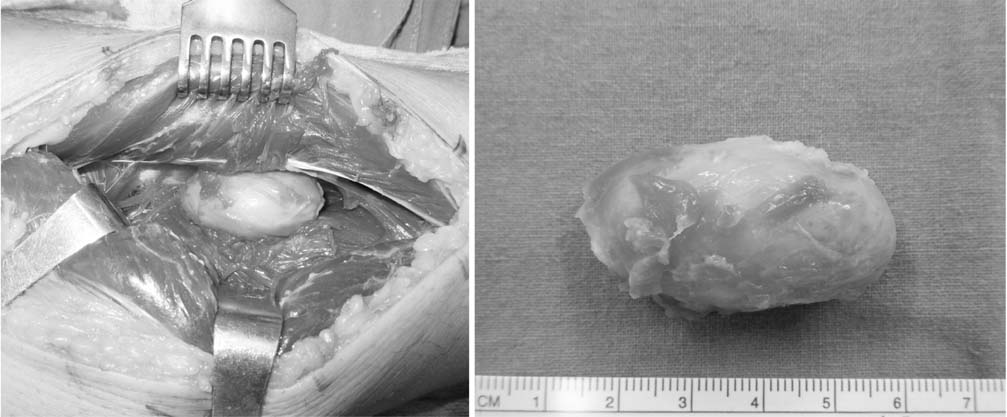
Oncogenic Osteomalacia with Multiple Insufficiency Fractures: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kyang@yuhs.ac
- KMID: 2424124
- DOI: http://doi.org/10.12671/jkfs.2017.30.3.146
Abstract
- Oncogenic osteomalacia is a rare paraneoplastic syndrome, characterized by hypophosphatemia, renal phosphate wasting, osteomalacia, and multiple insufficiency fractures, as a result of the tumor. A wide excision of the causative tumor is considered as the treatment of choice, following which, a dramatic recovery is expected. Authors report a case in which the symptoms and bone mineral density were dramatically recovered after an excision of the causative tumor around the tibialis posterior muscle in oncogenic osteomalacia.
Figure
Reference
-
1. McCance RA. Osteomalacia with Looser's nodes (Milkman's syndrome) due to a raised resistance to vitamin D acquired about the age of 15 years. Q J Med. 1947; 16:33–46.2. Kumar R, Folpe AL, Mullan BP. Tumor-induced osteomalacia. Transl Endocrinol Metab. 2015; 7:1871.3. Ledford CK, Zelenski NA, Cardona DM, Brigman BE, Eward WC. The phosphaturic mesenchymal tumor: why is definitive diagnosis and curative surgery often delayed? Clin Orthop Relat Res. 2013; 471:3618–3625.
Article4. Jan de Beur SM. Tumor-induced osteomalacia. JAMA. 2005; 294:1260–1267.
Article5. Jiang Y, Xia WB, Xing XP, et al. Tumor-induced osteomalacia: an important cause of adult-onset hypophosphatemic osteomalacia in China: report of 39 cases and review of the literature. J Bone Miner Res. 2012; 27:1967–1975.
Article6. Chong WH, Andreopoulou P, Chen CC, et al. Tumor localization and biochemical response to cure in tumor-induced osteomalacia. J Bone Miner Res. 2013; 28:1386–1398.
Article7. Zhang J, Zhu Z, Zhong D, et al. 68Ga DOTATATE PET/CT is an accurate imaging modality in the detection of culprit tumors causing osteomalacia. Clin Nucl Med. 2015; 40:642–646.
Article8. Andreopoulou P, Dumitrescu CE, Kelly MH, et al. Selective venous catheterization for the localization of phosphaturic mesenchymal tumors. J Bone Miner Res. 2011; 26:1295–1302.
Article9. Umphrey LG, Whitaker MD, Bosch EP, Cook CB. Clinical and bone density outcomes of tumor-induced osteomalacia after treatment. Endocr Pract. 2007; 13:458–462.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Osteosarcoma induced Oncogenic Osteomalacia Detected by MRI
- Nasal Hemangiopericytoma Causing Oncogenic Osteomalacia
- Oncogenic osteomalacia
- Using 18F-FDG PET/CT to Detect an Occult Mesenchymal Tumor Causing Oncogenic Osteomalacia
- A FGF23-Positive Maxillary Sinus Tumor Associated with Oncogenic Osteomalacia