J Gynecol Oncol.
2010 Sep;21(3):181-185. 10.3802/jgo.2010.21.3.181.
High expression of mTOR is associated with radiation resistance in cervical cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ds123.bae@samsung.com
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1980855
- DOI: http://doi.org/10.3802/jgo.2010.21.3.181
Abstract
OBJECTIVE
Mammalian target of rapamycin (mTOR) is known to promote cell proliferation, survival, and resistance to radiation. The aim of this study was to determine whether mTOR expression was associated with survival and the response to radiation in patients with cervical cancer.
METHODS
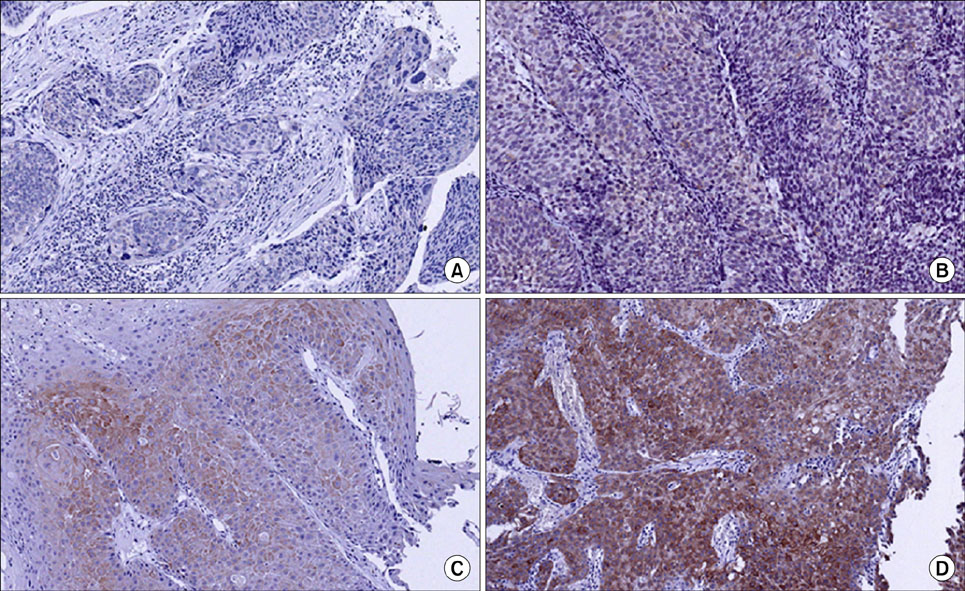
After reviewing 119 patients treated by primary radiotherapy for stage IIB-IVA cervical cancer, a case-control study was performed. The cases (n=12) with local recurrence or radiation failure after primary radiation therapy were selected. For each case, two controls that had no recurrence were selected. Using pretreatment paraffin-embedded tissues, the cytoplasmic expression of phosphorylated-mTOR (p-mTOR) was evaluated by immunohistochemistry. Staining was scored based on intensity (intensity score [IS] 0-3) and proportion (proportion score [PS] 0-100). The progression free survival (PFS) was defined from the end of treatment to the day of recurrence by imaging studies or biopsy. The staining distribution and PFS were compared between the two groups. The results were analyzed by the Student t-test, Mann-Whitney U-test, Fisher's exact test, and Cox proportional hazards regression model.
RESULTS
The p-mTOR cytoplasmic expression was significantly associated with a poor response to radiotherapy (p<0.01). With respect to survival, a higher cytoplasmic expression of p-mTOR was associated with a worse outcome (p=0.02). The hazard ratio for recurrence or radiation failure was 6.18 for mTOR IS and 1.04 for mTOR PS (p<0.05 for both), indicating that the degree of p-mTOR staining correlated with the recurrence risk.
CONCLUSION
High expression of p-mTOR was associated with radiation resistance; therefore p-mTOR may be a prognostic marker for response to radiotherapy in patients with cervical cancer.
Keyword
MeSH Terms
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005. 55:74–108.2. Petignat P, Roy M. Diagnosis and management of cervical cancer. BMJ. 2007. 335:765–768.3. Ogawa K, Murayama S, Mori M. Predicting the tumor response to radiotherapy using microarray analysis (Review). Oncol Rep. 2007. 18:1243–1248.4. Abraham RT, Gibbons JJ. The mammalian target of rapamycin signaling pathway: twists and turns in the road to cancer therapy. Clin Cancer Res. 2007. 13:3109–3114.5. Peterson RT, Beal PA, Comb MJ, Schreiber SL. FKBP12-rapamycin-associated protein (FRAP) autophosphorylates at serine 2481 under translationally repressive conditions. J Biol Chem. 2000. 275:7416–7423.6. Nave BT, Ouwens M, Withers DJ, Alessi DR, Shepherd PR. Mammalian target of rapamycin is a direct target for protein kinase B: identification of a convergence point for opposing effects of insulin and amino-acid deficiency on protein translation. Biochem J. 1999. 344 Pt 2:427–431.7. Herberger B, Puhalla H, Lehnert M, Wrba F, Novak S, Brandstetter A, et al. Activated mammalian target of rapamycin is an adverse prognostic factor in patients with biliary tract adenocarcinoma. Clin Cancer Res. 2007. 13:4795–4799.8. Pelloski CE, Lin E, Zhang L, Yung WK, Colman H, Liu JL, et al. Prognostic associations of activated mitogen-activated protein kinase and Akt pathways in glioblastoma. Clin Cancer Res. 2006. 12:3935–3941.9. Faried LS, Faried A, Kanuma T, Sano T, Nakazato T, Tamura T, et al. Predictive and prognostic role of activated mammalian target of rapamycin in cervical cancer treated with cisplatin-based neoadjuvant chemotherapy. Oncol Rep. 2006. 16:57–63.10. Ji J, Zheng PS. Activation of mTOR signaling pathway contributes to survival of cervical cancer cells. Gynecol Oncol. 2010. 117:103–108.11. Lee JE, Huh SJ, Park W, Lim do H, Ahn YC, Park CS, et al. Radical radiotherapy for locally advanced cancer of uterine cervix. Cancer Res Treat. 2004. 36:222–227.12. Freitas S, Moore DH, Michael H, Kelley MR. Studies of apurinic/apyrimidinic endonuclease/ref-1 expression in epithelial ovarian cancer: correlations with tumor progression and platinum resistance. Clin Cancer Res. 2003. 9:4689–4694.13. Paglin S, Lee NY, Nakar C, Fitzgerald M, Plotkin J, Deuel B, et al. Rapamycin-sensitive pathway regulates mitochondrial membrane potential, autophagy, and survival in irradiated MCF-7 cells. Cancer Res. 2005. 65:11061–11070.14. Cao C, Subhawong T, Albert JM, Kim KW, Geng L, Sekhar KR, et al. Inhibition of mammalian target of rapamycin or apoptotic pathway induces autophagy and radiosensitizes PTEN null prostate cancer cells. Cancer Res. 2006. 66:10040–10047.15. Bianco R, Garofalo S, Rosa R, Damiano V, Gelardi T, Daniele G, et al. Inhibition of mTOR pathway by everolimus cooperates with EGFR inhibitors in human tumours sensitive and resistant to anti-EGFR drugs. Br J Cancer. 2008. 98:923–930.16. Awada A, Cardoso F, Fontaine C, Dirix L, De Greve J, Sotiriou C, et al. The oral mTOR inhibitor RAD001 (everolimus) in combination with letrozole in patients with advanced breast cancer: results of a phase I study with pharmacokinetics. Eur J Cancer. 2008. 44:84–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clusterin expression and paclitaxel resistance in cervical cancer cell lines
- Increased expression of pAKT is associated with radiation resistance in cervical cancer
- Radiation sigmoiditis mimicking sigmoid colon cancer after radiation therapy for cervical cancer: the implications of three-dimensional image-based brachytherapy planning
- AR-mTOR-SRF Axis Regulates HMMR Expression in Human Prostate Cancer Cells
- PD-L1 Upregulation by the mTOR Pathway in VEGFR-TKI–Resistant Metastatic Clear Cell Renal Cell Carcinoma