Safe Sedation and Hypnosis using Dexmedetomidine for Minimally Invasive Spine Surgery in a Prone Position
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- KMID: 1802496
- DOI: http://doi.org/10.3344/kjp.2014.27.4.313
Abstract
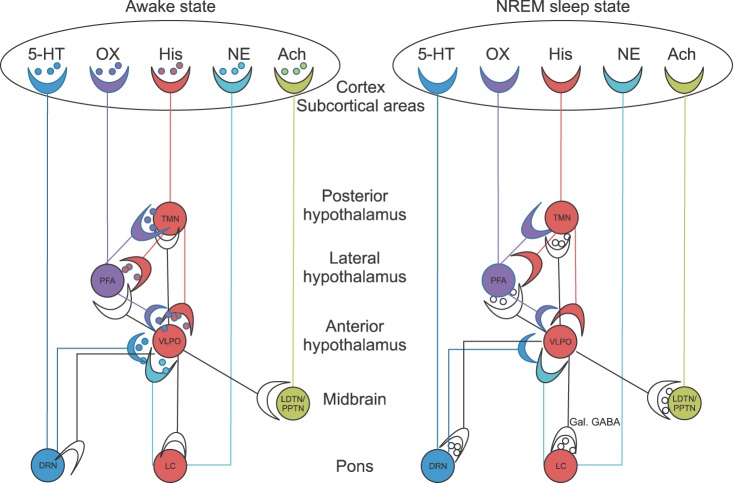
- Dexmedetomidine, an imidazoline compound, is a highly selective alpha2-adrenoceptor agonist with sympatholytic, sedative, amnestic, and analgesic properties. In order to minimize the patients' pain and anxiety during minimally invasive spine surgery (MISS) when compared to conventional surgery under general anesthesia, an adequate conscious sedation (CS) or monitored anesthetic care (MAC) should be provided. Commonly used intravenous sedatives and hypnotics, such as midazolam and propofol, are not suitable for operations in a prone position due to undesired respiratory depression. Dexmedetomidine converges on an endogenous non-rapid eye movement (NREM) sleep-promoting pathway to exert its sedative effects. The great merit of dexmedetomidine for CS or MAC is the ability of the operator to recognize nerve damage during percutaneous endoscopic lumbar discectomy, a representative MISS. However, there are 2 shortcomings for dexmedetomidine in MISS: hypotension/bradycardia and delayed emergence. Its hypotension/bradycardiac effects can be prevented by ketamine intraoperatively. Using atipamezole (an alpha2-adrenoceptor antagonist) might allow doctors to control the rate of recovery from procedural sedation in the future. MAC, with other analgesics such as ketorolac and opioids, creates ideal conditions for MISS. In conclusion, dexmedetomidine provides a favorable surgical condition in patients receiving MISS in a prone position due to its unique properties of conscious sedation followed by unconscious hypnosis with analgesia. However, no respiratory depression occurs based on the dexmedetomidine-related endogenous sleep pathways involves the inhibition of the locus coeruleus in the pons, which facilitates VLPO firing in the anterior hypothalamus.
Keyword
MeSH Terms
-
Adrenergic alpha-2 Receptor Agonists
Analgesia
Analgesics
Analgesics, Opioid
Anesthesia, General
Anxiety
Conscious Sedation
Dexmedetomidine*
Diskectomy
Diskectomy, Percutaneous
Eye Movements
Fires
Humans
Hypnosis*
Hypnotics and Sedatives
Hypothalamus, Anterior
Ketamine
Ketorolac
Locus Coeruleus
Midazolam
Pons
Prone Position*
Propofol
Respiratory Insufficiency
Spine*
Surgical Procedures, Minimally Invasive
Adrenergic alpha-2 Receptor Agonists
Analgesics
Analgesics, Opioid
Dexmedetomidine
Hypnotics and Sedatives
Ketamine
Ketorolac
Midazolam
Propofol
Figure
Cited by 7 articles
-
Dexmedetomidine during suprazygomatic maxillary nerve block for pediatric cleft palate repair, randomized double-blind controlled study
Mohamed F. Mostafa, Fatma A. Abdel Aal, Ibrahim Hassan Ali, Ahmed K. Ibrahim, Ragaa Herdan
Korean J Pain. 2020;33(1):81-89. doi: 10.3344/kjp.2020.33.1.81.Combined Use of Intrathecal Opioids and Dexmedetomidine in the Management of Neuropathic Pain
Mohamed Amin Ghobadifar, Farideh Pourghashdar, Armin Akbarzadeh, Zahra Mosallanejad
Korean J Pain. 2015;28(2):156-157. doi: 10.3344/kjp.2015.28.2.156.Dexamethasone or Dexmedetomidine as Local Anesthetic Adjuvants for Ultrasound-guided Axillary Brachial Plexus Blocks with Nerve Stimulation
Myeong Jong Lee, Dae Jeong Koo, Yu Sun Choi, Kyu Chang Lee, Hye Young Kim
Korean J Pain. 2016;29(1):29-33. doi: 10.3344/kjp.2016.29.1.29.Earlier treatment improves the chances of complete relief from postherpetic neuralgia
Dong Hee Kang, Su Young Kim, Hyuck Goo Kim, Jung Hyun Park, Tae Kyun Kim, Kyung Hoon Kim
Korean J Pain. 2017;30(3):214-219. doi: 10.3344/kjp.2017.30.3.214.Efficacy and safety of low dose oral ketamine for controlling pain and distress during intravenous cannulation in children: a double-blind, randomized, placebo-controlled trial
Mahdi Bagheri, Alireza Ebrahim Soltani, Mostafa Qorbani, Antoni Sureda, Toktam Faghihi
Korean J Pain. 2022;35(3):311-318. doi: 10.3344/kjp.2022.35.3.311.Prevention, diagnosis, and treatment of opioid use disorder under the supervision of opioid stewardship programs: it’s time to act now
Eun-Ji Kim, Eun-Jung Hwang, Yeong-Min Yoo, Kyung-Hoon Kim
Korean J Pain. 2022;35(4):361-382. doi: 10.3344/kjp.2022.35.4.361.Sedation for magnetic resonance imaging in the prone position - A report of four cases -
Jaewoong Jung, Youjin Kang, Won Seok Chae, Yang-Hoon Chung
Anesth Pain Med. 2022;17(3):286-290. doi: 10.17085/apm.21103.
Reference
-
1. Newman-Tancredi A, Nicolas JP, Audinot V, Gavaudan S, Verrièle L, Touzard M, et al. Actions of alpha2 adrenoceptor ligands at alpha2A and 5-HT1A receptors: the antagonist, atipamezole, and the agonist, dexmedetomidine, are highly selective for alpha2A adrenoceptors. Naunyn Schmiedebergs Arch Pharmacol. 1998; 358:197–206. PMID: 9750005.
Article2. Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001; 14:13–21. PMID: 16369581.
Article3. Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008; 4:619–627. PMID: 18484919.
Article4. Bylund DB, Eikenberg DC, Hieble JP, Langer SZ, Lefkowitz RJ, Minneman KP, et al. International Union of Pharmacology nomenclature of adrenoceptors. Pharmacol Rev. 1994; 46:121–136. PMID: 7938162.5. Insel PA. Seminars in medicine of the Beth Israel Hospital, Boston. Adrenergic receptors--evolving concepts and clinical implications. N Engl J Med. 1996; 334:580–585. PMID: 8569827.
Article6. Haselman MA. Dexmedetomidine: a useful adjunct to consider in some high-risk situations. AANA J. 2008; 76:335–339. PMID: 18947160.7. Correa-Sales C, Rabin BC, Maze M. A hypnotic response to dexmedetomidine, an alpha 2 agonist, is mediated in the locus coeruleus in rats. Anesthesiology. 1992; 76:948–952. PMID: 1350889.
Article8. Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology. 2003; 98:428–436. PMID: 12552203.
Article9. Nelson LE, Guo TZ, Lu J, Saper CB, Franks NP, Maze M. The sedative component of anesthesia is mediated by GABA(A) receptors in an endogenous sleep pathway. Nat Neurosci. 2002; 5:979–984. PMID: 12195434.
Article10. Saper CB, Scammell TE, Lu J. Hypothalamic regulation of sleep and circadian rhythms. Nature. 2005; 437:1257–1263. PMID: 16251950.
Article11. Huupponen E, Maksimow A, Lapinlampi P, Särkelä M, Saastamoinen A, Snapir A, et al. Electroencephalogram spindle activity during dexmedetomidine sedation and physiological sleep. Acta Anaesthesiol Scand. 2008; 52:289–294. PMID: 18005372.
Article12. Khan ZP, Ferguson CN, Jones RM. alpha-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role. Anaesthesia. 1999; 54:146–165. PMID: 10215710.
Article13. Hsu YW, Cortinez LI, Robertson KM, Keifer JC, Sum-Ping ST, Moretti EW, et al. Dexmedetomidine pharmacodynamics: part I: crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004; 101:1066–1076. PMID: 15505441.14. Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996; 84:873–881. PMID: 8638842.
Article15. Li SS, Zhang WS, Ji D, Zhou YL, Li H, Yang JL, et al. Involvement of spinal microglia and interleukin-18 in the anti-nociceptive effect of dexmedetomidine in rats subjected to CCI. Neurosci Lett. 2014; 560:21–25. PMID: 24345418.
Article16. Funai Y, Pickering AE, Uta D, Nishikawa K, Mori T, Asada A, et al. Systemic dexmedetomidine augments inhibitory synaptic transmission in the superficial dorsal horn through activation of descending noradrenergic control: an in vivo patch-clamp analysis of analgesic mechanisms. Pain. 2014; 155:617–628. PMID: 24355412.
Article17. Fan QQ, Li L, Wang WT, Yang X, Suo ZW, Hu XD. Activation of α2 adrenoceptors inhibited NMDA receptor-mediated nociceptive transmission in spinal dorsal horn of mice with inflammatory pain. Neuropharmacology. 2014; 77:185–192. PMID: 24103367.
Article18. Seyrek M, Halici Z, Yildiz O, Ulusoy HB. Interaction between dexmedetomidine and α-adrenergic receptors: emphasis on vascular actions. J Cardiothorac Vasc Anesth. 2011; 25:856–862. PMID: 21862350.
Article19. Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992; 77:1134–1142. PMID: 1361311.20. Sulaiman S, Karthekeyan RB, Vakamudi M, Sundar AS, Ravullapalli H, Gandham R. The effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass grafting. Ann Card Anaesth. 2012; 15:39–43. PMID: 22234020.
Article21. Kallio A, Scheinin M, Koulu M, Ponkilainen R, Ruskoaho H, Viinamäki O, et al. Effects of dexmedetomidine, a selective alpha 2-adrenoceptor agonist, on hemodynamic control mechanisms. Clin Pharmacol Ther. 1989; 46:33–42. PMID: 2568211.
Article22. Shukry M, Miller JA. Update on dexmedetomidine: use in nonintubated patients requiring sedation for surgical procedures. Ther Clin Risk Manag. 2010; 6:111–121. PMID: 20421911.
Article23. Carollo DS, Nossaman BD, Ramadhyani U. Dexmedetomidine: a review of clinical applications. Curr Opin Anaesthesiol. 2008; 21:457–461. PMID: 18660652.
Article24. Gerlach AT, Dasta JF. Dexmedetomidine: an updated review. Ann Pharmacother. 2007; 41:245–252. PMID: 17299013.
Article25. Tobias JD. Dexmedetomidine and ketamine: an effective alternative for procedural sedation? Pediatr Crit Care Med. 2012; 13:423–427. PMID: 22067985.26. Pomarol-Clotet E, Honey GD, Murray GK, Corlett PR, Absalom AR, Lee M, et al. Psychological effects of ketamine in healthy volunteers. Phenomenological study. Br J Psychiatry. 2006; 189:173–179. PMID: 16880489.27. Kim KH. Use of lidocaine patch for percutaneous endoscopic lumbar discectomy. Korean J Pain. 2011; 24:74–80. PMID: 21716614.
Article28. Triltsch AE, Welte M, von Homeyer P, Grosse J, Genähr A, Moshirzadeh M, et al. Bispectral index-guided sedation with dexmedetomidine in intensive care: a prospective, randomized, double blind, placebo-controlled phase II study. Crit Care Med. 2002; 30:1007–1014. PMID: 12006795.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation for magnetic resonance imaging in the prone position - A report of four cases -
- Dexmedetomidine: Clinical Use
- Dexmedetomidine intravenous sedation using a patient-controlled sedation infusion pump: a case report
- Patient Positioning in Spine Surgery: What Spine Surgeons Should Know?
- Large Dose Dexmedetomidine in a Patient during Sedation for Invasive Oral Procedure