Anesth Pain Med.
2022 Jul;17(3):286-290. 10.17085/apm.21103.
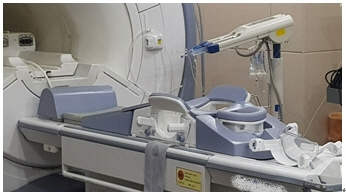
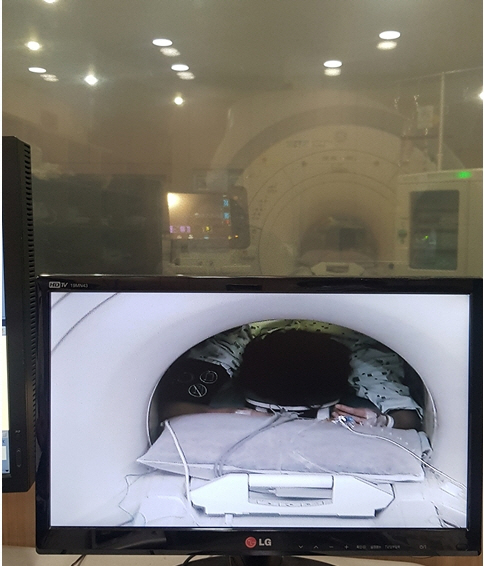
Sedation for magnetic resonance imaging in the prone position - A report of four cases -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- KMID: 2535321
- DOI: http://doi.org/10.17085/apm.21103
Abstract
- Background
Magnetic resonance imaging (MRI) is a useful tool, but it can be difficult to perform in those with claustrophobia as it requires being enclosed in a noisy cylindrical space. Being in the prone position is essential to spread breast tissue. However, sedation in a prone position is challenging because of the possibility of respiratory depression and the difficulty in manipulating the airway. Case: Four patients with claustrophobia were sedated using dexmedetomidine, has minimal effect on respiration. Dexmedetomidine also enables the patient’s cooperation in assuming the prone position while infusing loading time. But dexmedetomidine requires a longer time to reach moderate sedation, an intermittent bolus of midazolam was required for rapid induction of moderate sedation. All exams were conducted successfully without any complications. Conclusions: Administering dexmedetomidine and a midazolam bolus at the appropriate dose and timing will render MRI examinations in the prone position safe and satisfactory, without respiratory complications.
Keyword
Figure
Reference
-
1. Enders J, Zimmermann E, Rief M, Martus P, Klingebiel R, Asbach P, et al. Reduction of claustrophobia during magnetic resonance imaging: methods and design of the "CLAUSTRO" randomized controlled trial. BMC Med Imaging. 2011; 11:4.
Article2. Eshed I, Althoff CE, Hamm B, Hermann KG. Claustrophobia and premature termination of magnetic resonance imaging examinations. J Magn Reson Imaging. 2007; 26:401–4.
Article3. Kim KH. Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J Pain. 2014; 27:313–20.
Article4. Weerink MAS, Struys MMRF, Hannivoort LN, Barends CRM, Absalom AR, Colin P. Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet. 2017; 56:893–913.
Article5. Loh PS, Ariffin MA, Rai V, Lai LL, Chan L, Ramli N. Comparing the efficacy and safety between propofol and dexmedetomidine for sedation in claustrophobic adults undergoing magnetic resonance imaging (PADAM trial). J Clin Anesth. 2016; 34:216–22.
Article6. Candiotti KA, Bergese SD, Bokesch PM, Feldman MA, Wisemandle W, Bekker AY; MAC Study Group. Monitored anesthesia care with dexmedetomidine: a prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010; 110:47–56.
Article7. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–94.
Article8. Mahmoud M, Gunter J, Donnelly LF, Wang Y, Nick TG, Sadhasivam S. A comparison of dexmedetomidine with propofol for magnetic resonance imaging sleep studies in children. Anesth Analg. 2009; 109:745–53.
Article9. Kamal K, Asthana U, Bansal T, Dureja J, Ahlawat G, Kapoor S. Evaluation of efficacy of dexmedetomidine versus propofol for sedation in children undergoing magnetic resonance imaging. Saudi J Anaesth. 2017; 11:163–8.
Article10. Richa F, Chalhoub V, Dagher C, Yazbeck PH. Dexmedetomidine sedation for a claustrophobic patient with obstructive sleep apnea undergoing magnetic resonance imaging. J Clin Anesth. 2015; 27:698–9.
Article11. Nafiu OO, Srinivasan A, Ravanbakht J, Wu B, Lau WC. Dexmedetomidine sedation in a patient with superior vena cava syndrome and extreme needle phobia. J Cardiothorac Vasc Anesth. 2008; 22:581–3.
Article12. Barends CRM, Absalom AR, Struys MMRF. Drug selection for ambulatory procedural sedation. Curr Opin Anaesthesiol. 2018; 31:673–8.
Article13. Bang YS, So E, Kim S, Chun DH. Effects of low dose midazolam on bradycardia and sedation during dexmedetomidine infusion. Int J Clin Exp Med. 2016; 9:11838–44.14. Bol CJ, Vogelaar JP, Tang JP, Mandema JW. Quantification of pharmacodynamic interactions between dexmedetomidine and midazolam in the rat. J Pharmacol Exp Ther. 2000; 294:347–55.15. Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992; 77:1134–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation for Pediatric Patients Undergoing MRI
- Procedural Sedation of Preterm Neonate with Frequent Apnea during Magnetic Resonance Imaging: A Case Report
- Sedation under JCI standard
- Lateral Medullary Syndrome Caused by Prone Position for Spine Surgery
- Potential Clinical Applications of ¹â¸F-Fluorodeoxyglucose Positron Emission Tomography/Magnetic Resonance Mammography in Breast Cancer