Clin Exp Otorhinolaryngol.
2019 Aug;12(3):294-300. 10.21053/ceo.2018.00612.
The Effects of Air Pollutants on the Prevalence of Common Ear, Nose, and Throat Diseases in South Korea: A National Population-Based Study
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul Medical Center, Seoul, Korea.
- 2Clinical Research Center, Asan Institute of Life Sciences, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. entpmk@gmail.com
- KMID: 2455371
- DOI: http://doi.org/10.21053/ceo.2018.00612
Abstract
OBJECTIVES
The effects of air pollutants on upper airway disease development have been seldom studied. In this study, we evaluated the effects of air pollution on the prevalence of ENT diseases.
METHODS
We identified cases of ENT disease occurring in 2009, as recorded by the Korea National Health and Nutrition Examination Survey, and explored their associations with the levels of five air pollutants: sulfur dioxide (SOâ‚‚), nitrogen dioxide (NOâ‚‚), ozone (O₃), carbon monoxide (CO), and particulate matter (PMâ‚â‚€ particles; particulates ≤10 μm in aerodynamic diameter). Subjects diagnosed with at least one of the five studied ENT diseases were included in analysis, but those aged under 19 years were excluded. Linear associations between ENT disease frequency and pollutant levels were evaluated by calculating Spearman correlations. After adjusting for age, gender, and geographic region, multivariate logistic regression was used to obtain odds ratios (OR) with 95% confidence intervals (CI).
RESULTS
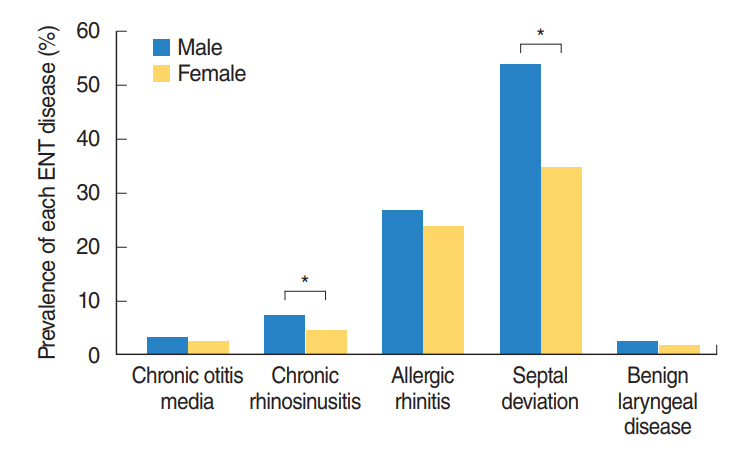
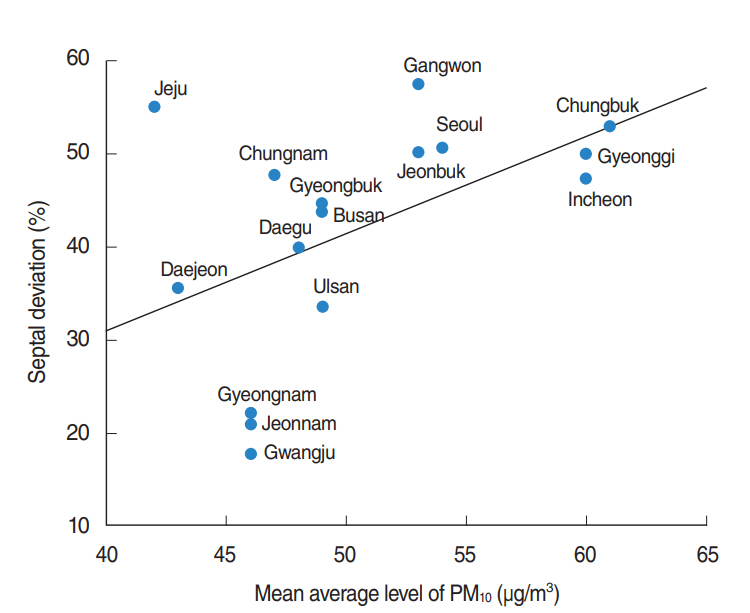
A total of 7,399 subjects with ENT diseases were identified. A linear association was evident between PMâ‚â‚€ concentration and the frequency of septal deviation (Spearman coefficient, 0.507; P=0.045). After adjustment, the PMâ‚â‚€ level was associated with high odds ratios for chronic rhinosinusitis (1.22; 95% CI, 1.02 to 1.46) and septal deviation (1.43; 95% CI, 1.22 to 1.67). Both of these conditions were more prevalent in males.
CONCLUSION
We found that increased ambient concentrations of PMâ‚â‚€ particles were clearly associated with increased the risk of chronic rhinosinusitis and septal deviation; the exposure-response relationship was definitive.
MeSH Terms
-
Air Pollutants*
Air Pollution
Carbon Monoxide
Ear*
Health Impact Assessment
Humans
Korea*
Logistic Models
Male
Nitrogen Dioxide
Nose*
Nutrition Surveys
Odds Ratio
Otorhinolaryngologic Diseases
Ozone
Particulate Matter
Pharynx*
Prevalence*
Respiratory Tract Infections
Sulfur Dioxide
Air Pollutants
Carbon Monoxide
Nitrogen Dioxide
Ozone
Particulate Matter
Sulfur Dioxide
Figure
Cited by 1 articles
-
Association of Particulate Matter With ENT Diseases
Ji-Hun Mo
Clin Exp Otorhinolaryngol. 2019;12(3):237-238. doi: 10.21053/ceo.2019.00752.
Reference
-
1. World Health Organization. Analysis of estimates of the environmental attributable fraction, by disease [Internet]. Geneva, CH: WHO Press;c2017 [cited 2018 Dec 20]. Available from: http://www.who.int/quantifying_ehimpacts/publications/preventingdisease5.pdf?ua=1.2. West JV. Acute upper airway infections: childhood respiratory infections. Br Med Bull. 2002; 61(1):215–30.3. Calderon-Garciduenas L, Franco-Lira M, Henriquez-Roldan C, Osnaya N, Gonzalez-Maciel A, Reynoso-Robles R, et al. Urban air pollution: influences on olfactory function and pathology in exposed children and young adults. Exp Toxicol Pathol. 2010; Jan. 62(1):91–102.4. Zhang F, Krafft T, Ye B, Zhang F, Zhang J, Luo H, et al. The lag effects and seasonal differences of air pollutants on allergic rhinitis in Beijing. Sci Total Environ. 2013; Jan. 442:172–6.
Article5. Zhang F, Wang W, Lv J, Krafft T, Xu J. Time-series studies on air pollution and daily outpatient visits for allergic rhinitis in Beijing, China. Sci Total Environ. 2011; Jun. 409(13):2486–92.
Article6. Zhang F, Xu J, Zhang Z, Meng H, Wang L, Lu J, et al. Ambient air quality and the effects of air pollutants on otolaryngology in Beijing. Environ Monit Assess. 2015; Aug. 187(8):495.
Article7. Calderon-Garciduenas L, Rodriguez-Alcaraz A, Garcia R, Barragan G, Villarreal-Calderon A, Madden MC. Cell proliferation in nasal respiratory epithelium of people exposed to urban pollution. Carcinogenesis. 1999; Mar. 20(3):383–9.8. Noh J, Sohn J, Cho J, Cho SK, Choi YJ, Kim C, et al. Short-term effects of ambient air pollution on emergency department visits for asthma: an assessment of effect modification by prior allergic disease history. J Prev Med Public Health. 2016; Sep. 49(5):329–41.
Article9. Kang SH, Heo J, Oh IY, Kim J, Lim WH, Cho Y, et al. Ambient air pollution and out-of-hospital cardiac arrest. Int J Cardiol. 2016; Jan. 203:1086–92.
Article10. Hong YC, Lee JT, Kim H, Kwon HJ. Air pollution: a new risk factor in ischemic stroke mortality. Stroke. 2002; Sep. 33(9):2165–9.11. Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014; Sep. 122(9):906–11.
Article12. Rogers GA, Den Beste K, Parkos CA, Nusrat A, Delgaudio JM, Wise SK. Epithelial tight junction alterations in nasal polyposis. Int Forum Allergy Rhinol. 2011; Jan-Feb. 1(1):50–4.
Article13. London NR Jr, Tharakan A, Ramanathan M Jr. The role of innate immunity and aeroallergens in chronic rhinosinusitis. Adv Otorhinolaryngol. 2016; 79:69–77.14. Nicolussi FH, Santos AP, Andre SC, Veiga TB, Takayanagui AM. Air pollution and respiratory allergic diseases in schoolchildren. Rev Saude Publica. 2014; Apr. 48(2):326–30.15. Brauer M, Hoek G, Van Vliet P, Meliefste K, Fischer PH, Wijga A, et al. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am J Respir Crit Care Med. 2002; Oct. 166(8):1092–8.
Article16. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007; May. 29(5):879–88.
Article17. Pedersen PA, Weeke ER. Allergic rhinitis in Danish general practice: prevalence and consultation rates. Allergy. 1981; Aug. 36(6):375–9.18. Mamikoglu B, Houser S, Akbar I, Ng B, Corey JP. Acoustic rhinometry and computed tomography scans for the diagnosis of nasal septal deviation, with clinical correlation. Otolaryngol Head Neck Surg. 2000; Jul. 123(1 Pt 1):61–8.
Article19. Szucs E, Clement PA. Acoustic rhinometry and rhinomanometry in the evaluation of nasal patency of patients with nasal septal deviation. Am J Rhinol. 1998; Sep-Oct. 12(5):345–52.20. Choi H, Park IH, Yoon HG, Lee HM. Diagnostic accuracy evaluation of nasal sound spectral analysis compared with peak nasal inspiratory flow in nasal septal deviation. Am J Rhinol Allergy. 2011; Mar-Apr. 25(2):e86–9.
Article21. Andrades P, Cuevas P, Danilla S, Bernales J, Longton C, Borel C, et al. The accuracy of different methods for diagnosing septal deviation in patients undergoing septorhinoplasty: a prospective study. J Plast Reconstr Aesthet Surg. 2016; Jun. 69(6):848–55.
Article22. Sedaghat AR, Busaba NY, Cunningham MJ, Kieff DA. Clinical assessment is an accurate predictor of which patients will need septoplasty. Laryngoscope. 2013; Jan. 123(1):48–52.
Article23. Calderon-Garciduenas L, Rodriguez-Alcaraz A, Villarreal-Calderon A, Lyght O, Janszen D, Morgan KT. Nasal epithelium as a sentinel for airborne environmental pollution. Toxicol Sci. 1998; Dec. 46(2):352–64.
Article24. Calderon-Garciduenas L, Rodriguez-Alcaraz A, Valencia-Salazar G, Mora-Tascareno A, Garcia R, Osnaya N, et al. Nasal biopsies of children exposed to air pollutants. Toxicol Pathol. 2001; Sep-Oct. 29(5):558–64.
Article25. Calderon-Garciduenas L, Valencia-Salazar G, Rodriguez-Alcaraz A, Gambling TM, Garcia R, Osnaya N, et al. Ultrastructural nasal pathology in children chronically and sequentially exposed to air pollutants. Am J Respir Cell Mol Biol. 2001; Feb. 24(2):132–8.
Article26. Abbey DE, Burchette RJ, Knutsen SF, McDonnell WF, Lebowitz MD, Enright PL. Long-term particulate and other air pollutants and lung function in nonsmokers. Am J Respir Crit Care Med. 1998; Jul. 158(1):289–98.
Article27. Galizia A, Kinney PL. Long-term residence in areas of high ozone: associations with respiratory health in a nationwide sample of nonsmoking young adults [dsee comments]. Environ Health Perspect. 1999; Aug. 107(8):675–9.
Article28. Korrick SA, Neas LM, Dockery DW, Gold DR, Allen GA, Hill LB, et al. Effects of ozone and other pollutants on the pulmonary function of adult hikers. Environ Health Perspect. 1998; Feb. 106(2):93–9.
Article29. Wang B, Peng Z, Zhang X, Xu Y, Wang H, Allen G, et al. Particulate matter, sulfur dioxide, and pulmonary function in never-smoking adults in Chongqing, China. Int J Occup Environ Health. 1999; Jan-Mar. 5(1):14–9.
Article30. Ackermann-Liebrich U, Leuenberger P, Schwartz J, Schindler C, Monn C, Bolognini G, et al. Lung function and long term exposure to air pollutants in Switzerland. Study on Air Pollution and Lung Diseases in Adults (SAPALDIA) Team. Am J Respir Crit Care Med. 1997; Jan. 155(1):122–9.
Article31. Chestnut LG, Schwartz J, Savitz DA, Burchfiel CM. Pulmonary function and ambient particulate matter: epidemiological evidence from NHANES I. Arch Environ Health. 1991; May-Jun. 46(3):135–44.32. Jedrychowski W, Krzyzanowski M. Ventilatory lung function and chronic chest symptoms among the inhabitants of urban areas with various levels of acid aerosols: prospective study in Cracow. Environ Health Perspect. 1989; Feb. 79:101–7.
Article33. Oosterlee A, Drijver M, Lebret E, Brunekreef B. Chronic respiratory symptoms in children and adults living along streets with high traffic density. Occup Environ Med. 1996; Apr. 53(4):241–7.
Article34. Zeka A, Zanobetti A, Schwartz J. Individual-level modifiers of the effects of particulate matter on daily mortality. Am J Epidemiol. 2006; May. 163(9):849–59.
Article35. Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Environ Health Perspect. 2010; Feb. 118(2):167–76.
Article36. Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Cien Saude Colet. 2011; Apr. 16(4):2221–38.
Article