Allergy Asthma Respir Dis.
2016 Jul;4(4):248-256. 10.4168/aard.2016.4.4.248.
Air pollution and childhood allergic disease
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea. yoolina@korea.ac.kr
- 2Environmental Health Center, Korea University Anam Hospital, Seoul, Korea.
- 3Allergy Immunology Center, Korea University, Seoul, Korea.
- KMID: 2346753
- DOI: http://doi.org/10.4168/aard.2016.4.4.248
Abstract
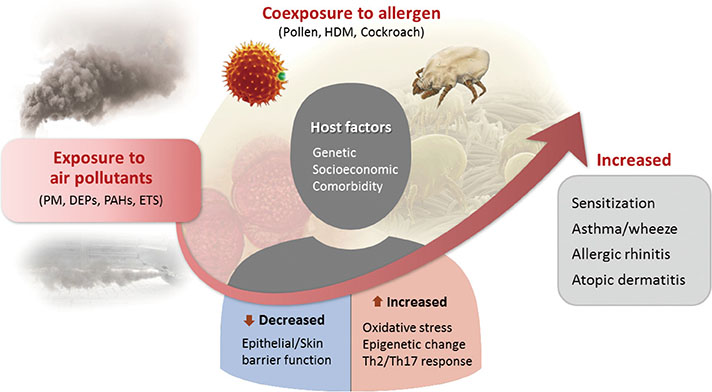
- Epidemiological studies suggest that there is a strong relationship between air pollution and childhood allergic disease. This review will summarize the association between exposure to air pollutants and subsequent development of asthma, allergies, and sensitization. Air pollutants probably induce oxidative stress, epigenetic change, and altered microRNA expression in the airway and skin, leading to immune dysregulation. This review considers acute and chronic effects of air pollution on the development and aggravation of allergic disease; the adverse health effect of air pollution on susceptible population, particular time period, and coexposure to allergens; and potential mechanisms involving development of allergic disease by exposure to air pollutants.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Allergic sensitization and its association with air pollution in childhood allergic rhinitis
Hyo-Bin Kim
Allergy Asthma Respir Dis. 2018;6(4):189-190. doi: 10.4168/aard.2018.6.4.189.A study on the correlation between outbreak of allergic rhinitis and airborne pollen in September
Jong Seok Kim, ye Joo So, Jeong Hee Kim, Dae Hyun Lim
Allergy Asthma Respir Dis. 2019;7(4):192-198. doi: 10.4168/aard.2019.7.4.192.
Reference
-
1. Jenerowicz D, Silny W, Danczak-Pazdrowska A, Polanska A, Osmola-Mankowska A, Olek-Hrab K. Environmental factors and allergic diseases. Ann Agric Environ Med. 2012; 19:475–481.2. Brandt EB, Myers JM, Ryan PH, Hershey GK. Air pollution and allergic diseases. Curr Opin Pediatr. 2015; 27:724–735.
Article3. Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015; 70:245–256.
Article4. Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011; 378:888–897.
Article5. Nastos PT, Paliatsos AG, Anthracopoulos MB, Roma ES, Priftis KN. Outdoor particulate matter and childhood asthma admissions in Athens, Greece: a time-series study. Environ Health. 2010; 9:45.
Article6. Jang AS, Kim BY, Lee CH, Park JS, Lee JH, Park SW, et al. Hospital visits and admissions in patients with asthma, COPD, and cardiovascular diseases according to air pollutants. Korean J Asthma Allergy Clin Immunol. 2006; 26:233–238.7. Lee JT. Associations between air pollution and asthma-related hospital admissions in children in Seoul, Korea: a case-crossover study. Korean J Prev Med. 2003; 36:47–53.8. Yoo Y, Choung JT, Yu J, Kim DK, Koh YY. Acute effects of Asian dust events on respiratory symptoms and peak expiratory flow in children with mild asthma. J Korean Med Sci. 2008; 23:66–71.
Article9. Lee YL, Su HJ, Sheu HM, Yu HS, Guo YL. Traffic-related air pollution, climate, and prevalence of eczema in Taiwanese school children. J Invest Dermatol. 2008; 128:2412–2420.
Article10. Song S, Lee K, Lee YM, Lee JH, Lee SI, Yu SD, et al. Acute health effects of urban fine and ultrafine particles on children with atopic dermatitis. Environ Res. 2011; 111:394–399.
Article11. Song S, Paek D, Lee K, Lee YM, Lee C, Park C, et al. Effects of ambient fine particles on pulmonary function in children with mild atopic dermatitis. Arch Environ Occup Health. 2013; 68:228–234.
Article12. He R, Kim HY, Yoon J, Oyoshi MK, MacGinnitie A, Goya S, et al. Exaggerated IL-17 response to epicutaneous sensitization mediates airway inflammation in the absence of IL-4 and IL-13. J Allergy Clin Immunol. 2009; 124:761.e1–770.e1.
Article13. Lee YL, Shaw CK, Su HJ, Lai JS, Ko YC, Huang SL, et al. Climate, traffic-related air pollutants and allergic rhinitis prevalence in middle-school children in Taiwan. Eur Respir J. 2003; 21:964–970.
Article14. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Kramer U, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008; 177:1331–1337.
Article15. Jung DY, Leem JH, Kim HC, Kim JH, Hwang SS, Lee JY, et al. Effect of traffic-related air pollution on allergic disease: results of the children's health and environmental research. Allergy Asthma Immunol Res. 2015; 7:359–366.
Article16. Kousha T, Valacchi G. The air quality health index and emergency department visits for urticaria in Windsor, Canada. J Toxicol Environ Health A. 2015; 78:524–533.
Article17. Gehring U, Wijga AH, Brauer M, Fischer P, de Jongste JC, Kerkhof M, et al. Traffic-related air pollution and the development of asthma and allergies during the first 8 years of life. Am J Respir Crit Care Med. 2010; 181:596–603.
Article18. Seo S, Kim D, Min S, Paul C, Yoo Y, Choung JT. GIS-based association between PM10 and allergic diseases in Seoul: Implications for Health and Environmental Policy. Allergy Asthma Immunol Res. 2016; 8:32–40.
Article19. Jung KH, Hsu SI, Yan B, Moors K, Chillrud SN, Ross J, et al. Childhood exposure to fine particulate matter and black carbon and the development of new wheeze between ages 5 and 7 in an urban prospective cohort. Environ Int. 2012; 45:44–50.
Article20. Guo P, Yokoyama K, Suenaga M, Kida H. Mortality and life expectancy of Yokkaichi asthma patients, Japan: late effects of air pollution in 1960-70s. Environ Health. 2008; 7:8.
Article21. Jeong SH, Kim JH, Son BK, Hong SC, Kim SY, Lee GH, et al. Comparison of air pollution and the prevalence of allergy-related diseases in Incheon and Jeju City. Korean J Pediatr. 2011; 54:501–506.
Article22. Matsui EC, Hansel NN, McCormack MC, Rusher R, Breysse PN, Diette GB. Asthma in the inner city and the indoor environment. Immunol Allergy Clin North Am. 2008; 28:665–686.
Article23. US Department of Health and Human Services, Centers for Disease Control and Prevention. The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention;2008.24. Yi O, Kwon HJ, Kim H, Ha M, Hong SJ, Hong YC, et al. Effect of environmental tobacco smoke on atopic dermatitis among children in Korea. Environ Res. 2012; 113:40–45.
Article25. Dietert RR, Zelikoff JT. Early-life environment, developmental immunotoxicology, and the risk of pediatric allergic disease including asthma. Birth Defects Res B Dev Reprod Toxicol. 2008; 83:547–560.
Article26. Patel MM, Quinn JW, Jung KH, Hoepner L, Diaz D, Perzanowski M, et al. Traffic density and stationary sources of air pollution associated with wheeze, asthma, and immunoglobulin E from birth to age 5 years among New York City children. Environ Res. 2011; 111:1222–1229.
Article27. Gauderman WJ, Avol E, Gilliland F, Vora H, Thomas D, Berhane K, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004; 351:1057–1067.
Article28. Park M, Luo S, Kwon J, Stock TH, Delclos G, Kim H, et al. Effects of air pollution on asthma hospitalization rates in different age group in metropolitan cities of Korea. Air Qual Atmos Health. 2013; 6:543–551.
Article29. Silverman RA, Ito K. Age-related association of fine particles and ozone with severe acute asthma in New York City. J Allergy Clin Immunol. 2010; 125:367.e5–373.e5.
Article30. Norris G, YoungPong SN, Koenig JQ, Larson TV, Sheppard L, Stout JW. An association between fine particles and asthma emergency department visits for children in Seattle. Environ Health Perspect. 1999; 107:489–493.
Article31. Rabinovitch N, Strand M, Gelfand EW. Particulate levels are associated with early asthma worsening in children with persistent disease. Am J Respir Crit Care Med. 2006; 173:1098–1105.
Article32. Seo SC, Kang IS, Lim SG, Choung JT, Yoo Y. Indoor air pollutants and atopic dermatitis in socioeconomically disadvantaged children. Allergy Asthma Respir Dis. 2015; 3:206–212.
Article33. Holgate ST, Sandstrom T, Frew AJ, Stenfors N, Nordenhall C, Salvi S, et al. Health effects of acute exposure to air pollution. Part I: Healthy and asthmatic subjects exposed to diesel exhaust. Res Rep Health Eff Inst. 2003; (112):1–30.34. Hansell AL, Rose N, Cowie CT, Belousova EG, Bakolis I, Ng K, et al. Weighted road density and allergic disease in children at high risk of developing asthma. PLoS One. 2014; 9:e98978.
Article35. MacIntyre EA, Brauer M, Melén E, Bauer CP, Bauer M, Berdel D, et al. GSTP1 and TNF gene variants and associations between air pollution and incident childhood asthma: the traffic, asthma and genetics (TAG) study. Environ Health Perspect. 2014; 122:418–424.
Article36. Yoo Y, Perzanowski MS. Allergic sensitization and the environment: latest update. Curr Allergy Asthma Rep. 2014; 14:465.
Article37. Brandt EB, Biagini Myers JM, Acciani TH, Ryan PH, Sivaprasad U, Ruff B, et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J Allergy Clin Immunol. 2015; 136:295.e7–303.e7.
Article38. Cho YS, Moon HB. The role of oxidative stress in the pathogenesis of asthma. Allergy Asthma Immunol Res. 2010; 2:183–187.
Article39. Wang IJ, Tung TH, Tang CS, Zhao ZH. Allergens, air pollutants, and childhood allergic diseases. Int J Hyg Environ Health. 2016; 219:66–71.
Article40. Reddy P, Naidoo RN, Robins TG, Mentz G, Li H, London SJ, et al. GSTM1 and GSTP1 gene variants and the effect of air pollutants on lung function measures in South African children. Am J Ind Med. 2012; 55:1078–1086.
Article41. Niwa Y, Sumi H, Kawahira K, Terashima T, Nakamura T, Akamatsu H. Protein oxidative damage in the stratum corneum: Evidence for a link between environmental oxidants and the changing prevalence and nature of atopic dermatitis in Japan. Br J Dermatol. 2003; 149:248–254.
Article42. Watanabe M, Kurai J, Tomita K, Sano H, Abe S, Saito R, et al. Effects on asthma and induction of interleukin-8 caused by Asian dust particles collected in western Japan. J Asthma. 2014; 51:595–602.
Article43. Saunders V, Breysse P, Clark J, Sproles A, Davila M, Wills-Karp M. Particulate matter-induced airway hyperresponsiveness is lymphocyte dependent. Environ Health Perspect. 2010; 118:640–646.
Article44. Shadie AM, Herbert C, Kumar RK. Ambient particulate matter induces an exacerbation of airway inflammation in experimental asthma: role of interleukin-33. Clin Exp Immunol. 2014; 177:491–499.
Article45. Lambert AL, Trasti FS, Mangum JB, Everitt JI. Effect of preexposure to ultrafine carbon black on respiratory syncytial virus infection in mice. Toxicol Sci. 2003; 72:331–338.
Article46. Diaz-Sanchez D, Tsien A, Casillas A, Dotson AR, Saxon A. Enhanced nasal cytokine production in human beings after in vivo challenge with diesel exhaust particles. J Allergy Clin Immunol. 1996; 98:114–123.
Article47. Kanoh T, Suzuki T, Ishimori M, Ikeda S, Ohasawa M, Ohkuni H, et al. Adjuvant activities of pyrene, anthracene, fluoranthene and benzo(a)pyrene in production of anti-IgE antibody to Japanese cedar pollen allergen in mice. J Clin Lab Immunol. 1996; 48:133–147.48. Perzanowski MS, Chew GL, Divjan A, Jung KH, Ridder R, Tang D, et al. Early-life cockroach allergen and polycyclic aromatic hydrocarbon exposures predict cockroach sensitization among inner-city children. J Allergy Clin Immunol. 2013; 131:886–893.
Article49. Cornell AG, Chillrud SN, Mellins RB, Acosta LM, Miller RL, Quinn JW, et al. Domestic airborne black carbon and exhaled nitric oxide in children in NYC. J Expo Sci Environ Epidemiol. 2012; 22:258–266.
Article50. Perera F, Tang WY, Herbstman J, Tang D, Levin L, Miller R, et al. Relation of DNA methylation of 5'-CpG island of ACSL3 to transplacental exposure to airborne polycyclic aromatic hydrocarbons and childhood asthma. PLoS One. 2009; 4:e4488.
Article51. Gilliland FD, Li YF, Dubeau L, Berhane K, Avol E, McConnell R, et al. Effects of glutathione S-transferase M1, maternal smoking during pregnancy, and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med. 2002; 166:457–463.
Article52. de Planell-Saguer M, Lovinsky-Desir S, Miller RL. Epigenetic regulation: the interface between prenatal and early-life exposure and asthma susceptibility. Environ Mol Mutagen. 2014; 55:231–243.
Article53. Ahn K. The role of air pollutants in atopic dermatitis. J Allergy Clin Immunol. 2014; 134:993–999.
Article54. Yoon WS, Ryu SR, Lee SS, Chae YS, Kim EJ, Choi JH, et al. Suppression of inflammation by recombinant Salmonella typhimurium harboring CCL22 microRNA. DNA Cell Biol. 2012; 31:290–297.
Article55. Herberth G, Bauer M, Gasch M, Hinz D, Roder S, Olek S, et al. Maternal and cord blood miR-223 expression associates with prenatal tobacco smoke exposure and low regulatory T-cell numbers. J Allergy Clin Immunol. 2014; 133:543–550.
Article