Intest Res.
2018 Apr;16(2):306-311. 10.5217/ir.2018.16.2.306.
A case of ulcerative colitis presenting with cerebral venous thrombosis
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. snow903@gmail.com
- 2Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2417684
- DOI: http://doi.org/10.5217/ir.2018.16.2.306
Abstract
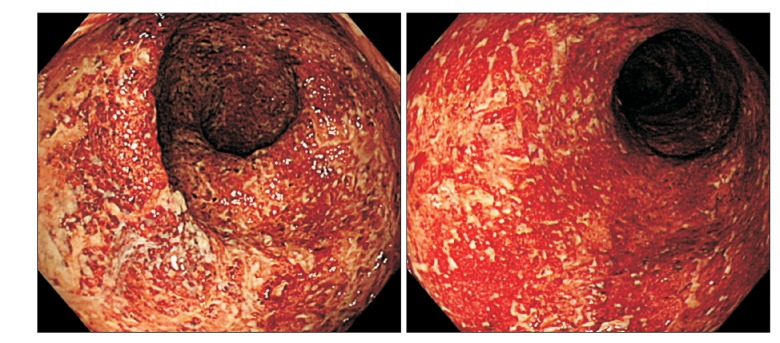
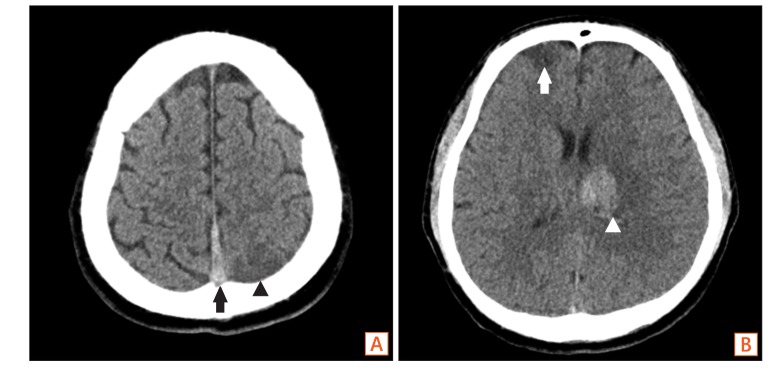
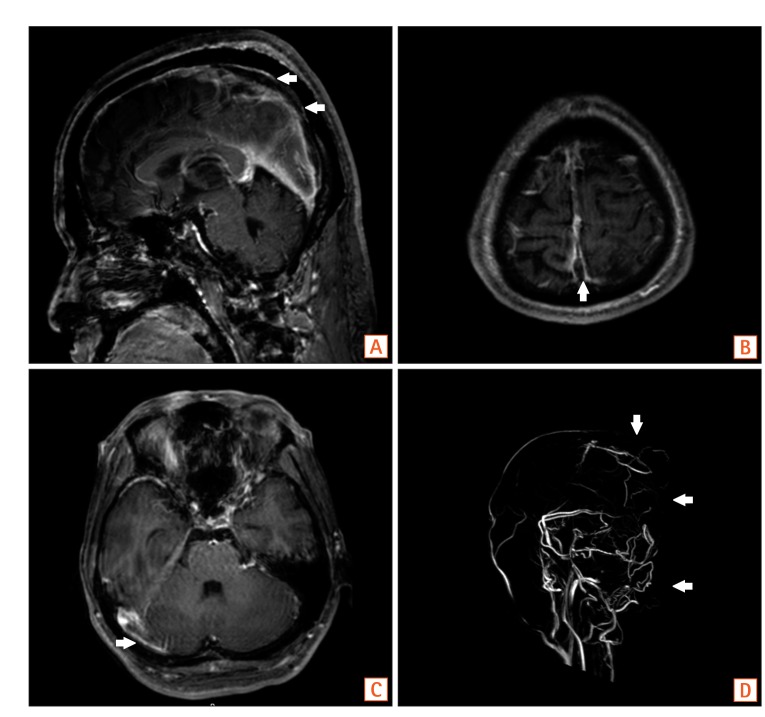
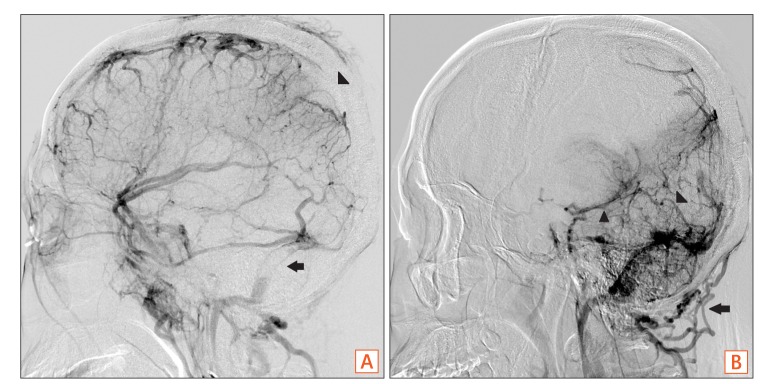
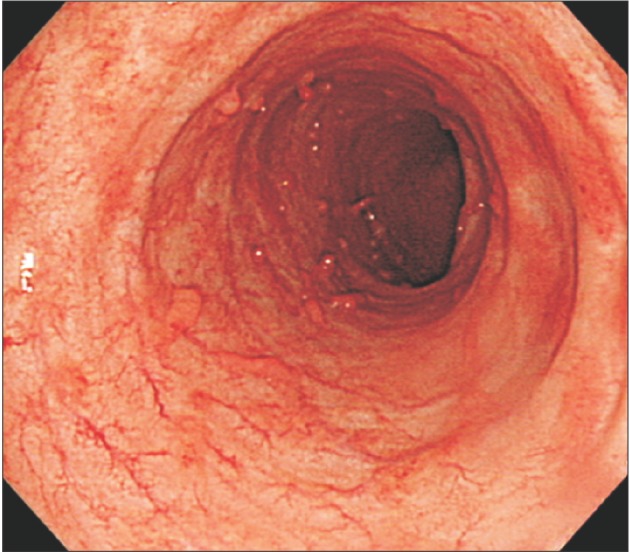
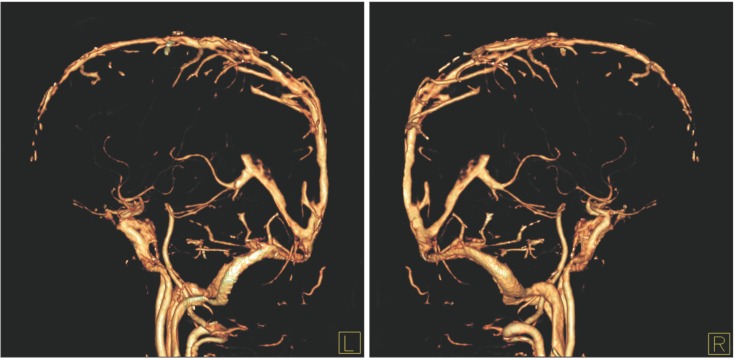
- Patients with inflammatory bowel disease (IBD) have been reported to have an increased risk of thromboembolism. Cerebral venous thrombosis (CVT) is a rare but serious extraintestinal manifestation of IBD. Due to its highly variable manifestation and low incidence, CVT is not usually readily recognized by physicians. Herein, we report a case of a 35-year-old male presenting with CVT associated with ulcerative colitis (UC). The patient was admitted with chief complaints of bloody diarrhea that had started 3 days prior. Sigmoidoscopy showed hyperemic and edematous mucosa, friability, and shallow ulcers from the sigmoid colon to the rectum suggestive of IBD. Three days later, the patient started complaining of a headache, and gradually developed a decreased level of consciousness. Magnetic resonance imaging of the brain revealed CVT with hemorrhagic infarctions. An angiogram was obtained to evaluate the extent of CVT, and anticoagulation therapy was initiated with intravenous heparin. During hospitalization, he was diagnosed with UC and treated with 5-aminosalicylic acid. After discharge, the patient was recovered without neurological deficit, and remission of UC was also obtained. The presence of headache or acute worsening of neurological status in a patient with IBD should alert the health professionals about the possibility of CVT.
Keyword
MeSH Terms
Figure
Reference
-
1. Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001; 85:430–434. PMID: 11307809.
Article2. Cho YH, Chae MK, Cha JM, et al. Cerebral venous thrombosis in a patient with Crohn's disease. Intest Res. 2016; 14:96–101. PMID: 26884741.
Article3. Bushnell C, Saposnik G. Evaluation and management of cerebral venous thrombosis. Continuum (Minneap Minn. 2014; 20:335–351. PMID: 24699485.
Article4. Katsanos AH, Katsanos KH, Kosmidou M, Giannopoulos S, Kyritsis AP, Tsianos EV. Cerebral sinus venous thrombosis in inflammatory bowel diseases. QJM. 2013; 106:401–413. PMID: 23243293.
Article5. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103:2272–2280. PMID: 18684186.
Article6. Danese S, Papa A, Saibeni S, Repici A, Malesci A, Vecchi M. Inflammation and coagulation in inflammatory bowel disease: the clot thickens. Am J Gastroenterol. 2007; 102:174–186. PMID: 17100967.
Article7. Bousser MG, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol. 2007; 6:162–170. PMID: 17239803.
Article8. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004; 35:664–670. PMID: 14976332.
Article9. Chauhan S, Sachdev A, D'Cruz S, Jain K, Singh R. Cerebral venous thrombosis in a patient with ulcerative colitis. Inflamm Bowel Dis. 2007; 13:1588–1589. PMID: 17663421.
Article10. Kawanishi M, Yoshida Y, Sakaguchi I, Nagano F, Kato K, Miyake H. Cerebral venous sinus thrombosis in a patient with ulcerative colitis. J Stroke Cerebrovasc Dis. 2003; 12:271–275. PMID: 17903939.
Article11. Crassard I, Bousser MG. Headache in patients with cerebral venous thrombosis. Rev Neurol (Paris). 2005; 161:706–708. PMID: 16141966.12. Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke. 2011; 42:1158–1192. PMID: 21293023.
Article13. Sipeki N, Davida L, Palyu E, et al. Prevalence, significance and predictive value of antiphospholipid antibodies in Crohn's disease. World J Gastroenterol. 2015; 21:6952–6964. PMID: 26078573.
Article14. Wasay M, Azeemuddin M. Neuroimaging of cerebral venous thrombosis. J Neuroimaging. 2005; 15:118–128. PMID: 15746223.
Article15. Einhäupl K, Stam J, Bousser MG, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010; 17:1229–1235. PMID: 20402748.
Article16. de Bruijn SF, Stam J. Randomized, placebo-controlled trial of anticoagulant treatment with low-molecular-weight heparin for cerebral sinus thrombosis. Stroke. 1999; 30:484–488. PMID: 10066840.
Article17. Nudelman RJ, Rosen DG, Rouah E, Verstovsek G. Cerebral sinus thrombosis: a fatal neurological complication of ulcerative colitis. Patholog Res Int. 2010; 2010:132754. DOI: 10.4061/2010/132754. PMID: 21152173.
Article18. Markowitz RL, Ment LR, Gryboski JD. Cerebral thromboembolic disease in pediatric and adult inflammatory bowel disease: case report and review of the literature. J Pediatr Gastroenterol Nutr. 1989; 8:413–420. PMID: 2651640.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cerebral Venous Thrombosis in Active Ulcerative Colitis
- A Case of Hemorrhagic Cerebral Infarction in Ulcerative Colitis
- Unusual Complication of Crohn's Disease: Portal Hypertension Related with Rapid Progression of Portal Vein and Superior Mesenteric Vein Thrombosis
- A Case of Hepatic Vein Thrombosis Associated with Ulcerative Colitis
- A Case of Pulmonary Thromboembolism in Active Ulcerative Colitis