Ann Pediatr Endocrinol Metab.
2018 Mar;23(1):51-55. 10.6065/apem.2018.23.1.51.
Hepatopulmonary syndrome caused by hypothalamic obesity and nonalcoholic fatty liver disease after surgery for craniopharyngioma: a case report
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. hwyoo@amc.seoul.kr
- KMID: 2409791
- DOI: http://doi.org/10.6065/apem.2018.23.1.51
Abstract
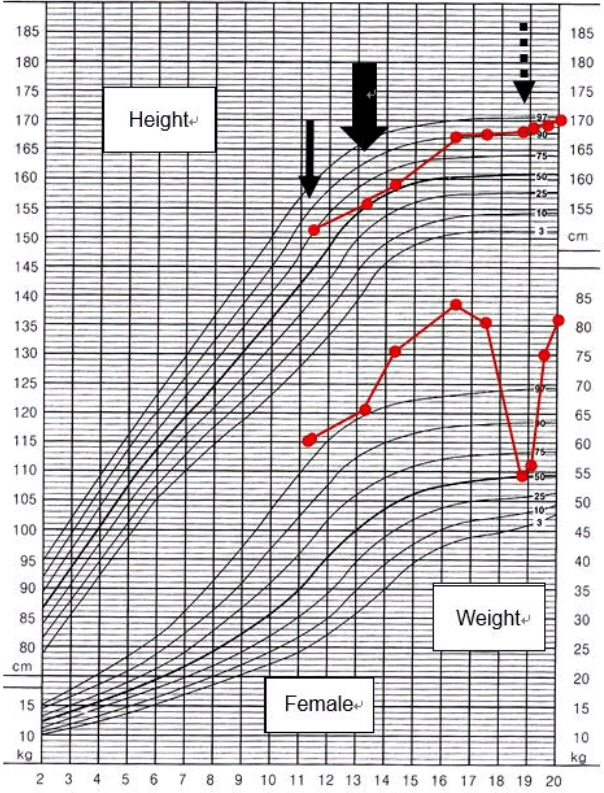
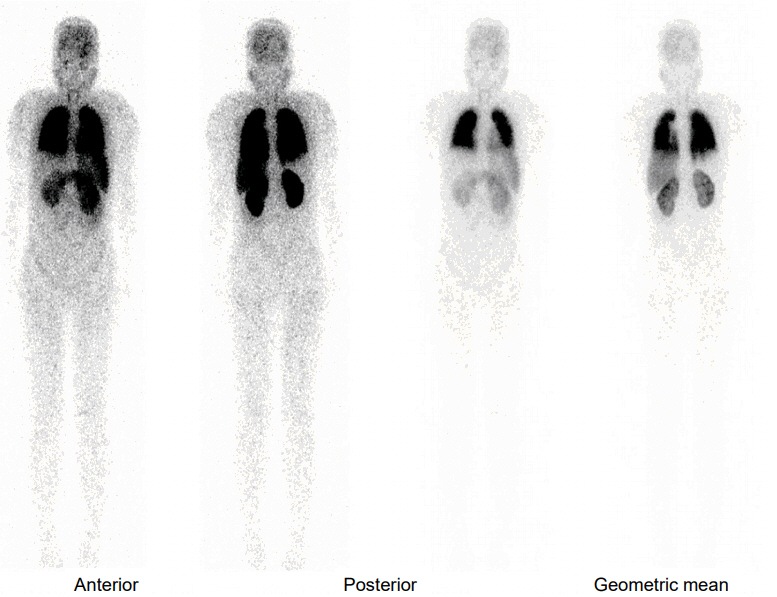
- Hypothalamic obesity is often complicated in patients with craniopharyngioma due to hypothalamic damage by the tumor itself, treatment modalities, and associated multiple pituitary hormone deficiency. Hypothalamic obesity causes secondary diseases such as nonalcoholic fatty liver disease (NAFLD) and diabetes mellitus (DM). We report a 19-year-old female who was diagnosed with craniopharyngioma, developed hypothalamic obesity after tumor resection, and progressed to hepatopulmonary syndrome. She manifested NAFLD 1 year after tumor resection. Two years later, the craniopharyngioma recurred, and she underwent a second resection. Three years after her second operation, she was diagnosed with type 2 DM, after which she did not visit the outpatient clinic for 2 years and then suddenly reappeared with a weight loss of 25.8 kg that had occurred over 21 months. One month later, she presented to the Emergency Department with dyspnea. Laboratory findings revealed liver dysfunction and hypoxia with increased alveolar artery oxygen gradient. Liver biopsy showed portal hypertension and micronodular cirrhosis. Echocardiography and a lung perfusion scan demonstrated a right to left shunt. She was finally diagnosed with hepatopulmonary syndrome and is currently awaiting a donor for liver transplantation. Patients surviving craniopharyngioma need to be followed up carefully to detect signs of hypothalamic obesity and monitored for the development of other comorbidities such as DM, NAFLD, and hepatopulmonary syndrome.
Keyword
MeSH Terms
-
Ambulatory Care Facilities
Anoxia
Arteries
Biopsy
Comorbidity
Craniopharyngioma*
Diabetes Mellitus
Dyspnea
Echocardiography
Emergency Service, Hospital
Female
Fibrosis
Hepatopulmonary Syndrome*
Humans
Hypertension, Portal
Hypothalamus
Liver
Liver Diseases
Liver Transplantation
Lung
Non-alcoholic Fatty Liver Disease*
Obesity*
Oxygen
Perfusion
Tissue Donors
Weight Loss
Young Adult
Oxygen
Figure
Reference
-
References
1. Rodriguez FJ, Scheithauer BW, Tsunoda S, Kovacs K, Vidal S, Piepgras DG. The spectrum of malignancy in craniopharyngioma. Am J Surg Pathol. 2007; 31:1020–8.
Article2. Page-Wilson G, Wardlaw SL, Khandji AG, Korner J. Hypothalamic obesity in patients with craniopharyngioma: treatment approaches and the emerging role of gastric bypass surgery. Pituitary. 2012; 15:84–92.
Article3. Lustig RH. Hypothalamic obesity after craniopharyngioma: mechanisms, diagnosis, and treatment. Front Endocrinol (Lausanne). 2011; 2:60.
Article4. Hoffmann A, Müller HL. Novel perspectives on hypothalamic-pituitary dysfunction as a risk factor for nonalcoholic fatty liver disease. Minerva Endocrinol. 2017; 42:132–44.5. Hoffmann A, Bootsveld K, Gebhardt U, Daubenbüchel AM, Sterkenburg AS, Müller HL. Nonalcoholic fatty liver disease and fatigue in long-term survivors of childhood-onset craniopharyngioma. Eur J Endocrinol. 2015; 173:389–97.
Article6. Adams LA, Feldstein A, Lindor KD, Angulo P. Nonalcoholic fatty liver disease among patients with hypothalamic and pituitary dysfunction. Hepatology. 2004; 39:909–14.
Article7. Bereket A, Kiess W, Lustig RH, Muller HL, Goldstone AP, Weiss R, et al. Hypothalamic obesity in children. Obes Rev. 2012; 13:780–98.
Article8. Fujio A, Kawagishi N, Echizenya T, Tokodai K, Nakanishi C, Miyagi S, et al. Long-term survival with growth hormone replacement after liver transplantation of pediatric nonalcoholic steatohepatitis complicating acquired hypopituitarism. Tohoku J Exp Med. 2015; 235:61–7.
Article9. Lustig RH, Post SR, Srivannaboon K, Rose SR, Danish RK, Burghen GA, et al. Risk factors for the development of obesity in children surviving brain tumors. J Clin Endocrinol Metab. 2003; 88:611–6.
Article10. Khan MJ, Humayun KN, Donaldson M, Ahmed SF, Shaikh MG. Longitudinal changes in body mass index in children with craniopharyngioma. Horm Res Paediatr. 2014; 82:372–9.
Article11. Müller HL, Emser A, Faldum A, Bruhnken G, Etavard-Gorris N, Gebhardt U, et al. Longitudinal study on growth and body mass index before and after diagnosis of childhood craniopharyngioma. J Clin Endocrinol Metab. 2004; 89:3298–305.
Article12. Sterkenburg AS, Hoffmann A, Gebhardt U, Warmuth-Metz M, Daubenbüchel AM, Müller HL. Survival, hypothalamic obesity, and neuropsychological/psychosocial status after childhood-onset craniopharyngioma: newly reported long-term outcomes. Neuro Oncol. 2015; 17:1029–38.
Article13. Simoneau-Roy J, O'Gorman C, Pencharz P, Adeli K, Daneman D, Hamilton J. Insulin sensitivity and secretion in children and adolescents with hypothalamic obesity following treatment for craniopharyngioma. Clin Endocrinol (Oxf). 2010; 72:364–70.
Article14. Roth C, Wilken B, Hanefeld F, Schröter W, Leonhardt U. Hyperphagia in children with craniopharyngioma is associated with hyperleptinaemia and a failure in the downregulation of appetite. Eur J Endocrinol. 1998; 138:89–91.
Article15. Ahlskog JE, Randall PK, Hoebel BG. Hupothalamic hyperphagia: dissociation from hyperphagia following destruction of noradrenergic neurons. Science. 1975; 190:399–401.
Article16. Albert DJ, Petrovic DM, Jonik RH, Walsh ML. Enhanced defensiveness and increased food motivation each contribute to aggression and success in food competition by rats with medial hypothalamic lesions. Physiol Behav. 1991; 49:13–9.
Article17. Fallon MB. Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol. 2005; 39(4 Suppl 2):S138–42.18. Lv Y, Fan D. Hepatopulmonary syndrome. Dig Dis Sci. 2015; 60:1914–23.
Article19. Jankowska I, Socha P, Pawlowska J, Teisseyre M, Gliwicz D, Czubkowski P, et al. Recurrence of non-alcoholic steatohepatitis after liver transplantation in a 13-yr-old boy. Pediatr Transplant. 2007; 11:796–8.
Article20. Jonas MM, Krawczuk LE, Kim HB, Lillehei C, Perez-Atayde A. Rapid recurrence of nonalcoholic fatty liver disease after transplantation in a child with hypopituitarism and hepatopulmonary syndrome. Liver Transpl. 2005; 11:108–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of hepatopulmonary syndrome in a child with fatty liver disease secondary to hypopituitarism after craniopharyngioma resection
- Prevalence of the Nonalcoholic Fatty Liver Disease in Obese Children
- Gut Microbiota and Clinical Disease: Obesity and Nonalcoholic Fatty Liver Disease
- Nonalcoholic fatty liver disease in long-term survivors of childhood-onset craniopharyngioma
- Comorbid diseases in nonalcoholic fatty liver disease