Brain Tumor Res Treat.
2017 Oct;5(2):87-93. 10.14791/btrt.2017.5.2.87.
Outcomes in 20 Gynecologic Cancer Patient with Brain Metastasis: A Single Institution Retrospective Study
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea. chaeyong@snu.ac.kr
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2396452
- DOI: http://doi.org/10.14791/btrt.2017.5.2.87
Abstract
- BACKGROUND
The incidence of brain metastasis (BM) in gynecologic cancers has risen recently, due to prolonged survival times and an early diagnosis. We analyzed treatment outcomes of patients with BM from gynecologic cancers.
METHODS
Among 951 patients with BM who were treated in neurosurgical department from July 2003 to February 2016, a total of 20 (2%) patients were from gynecologic cancers. The patients' clinical characteristics were collected by using medical records. There were 14 (66.7%) ovarian cancers, 4 (19.0%) uterine cancers, and 2 (9.5%) cervical cancers. As a primary treatment modality, 11 patients were treated with Gamma Knife surgery (GKS), 6 with surgical resection followed by whole brain radiation therapy (WBRT), and 3 with WBRT only. Overall and progression-free survival according to the primary origin and the primary treatment were analyzed.
RESULTS
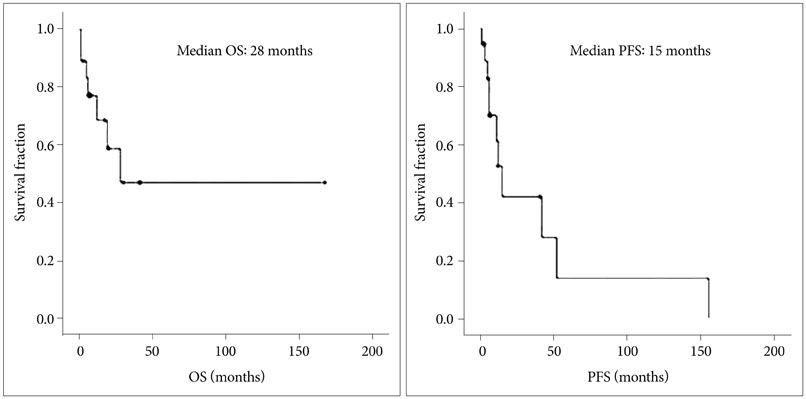
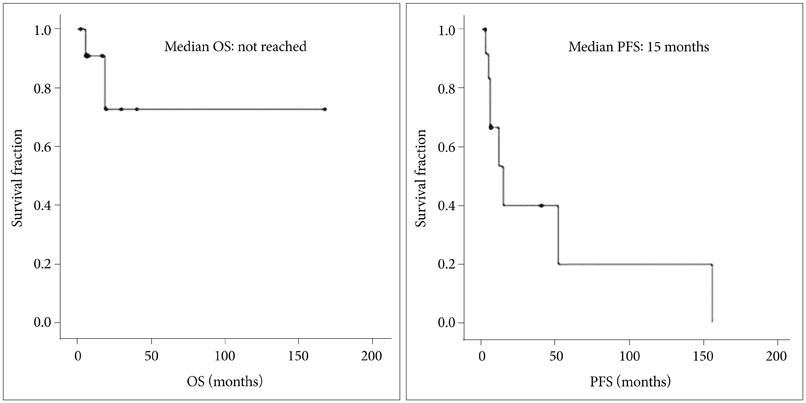
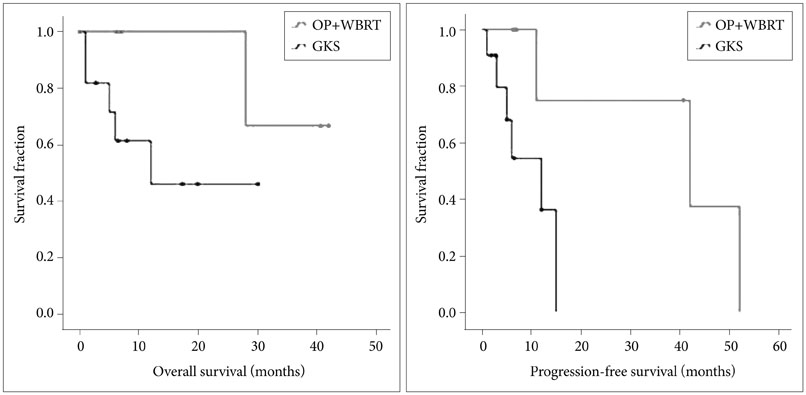
Median overall survival time was 28 months, and progression-free survival was 15 months. In patients with ovarian cancer, median overall survival did not reach during the follow-up periods and progression-free survival time was 15 months. Median overall survival time in patients who received GKS as the primary treatment was 17 months and that in patients who underwent surgical resection followed by WBRT was 37.3 months (p=0.16). The median value of progression-free survival time in patients who received GKS as the primary treatment was 12 months and that in patients who underwent surgical resection with WBRT was 42 months (p=0.042). Median follow up period of over all patients was 13 months.
CONCLUSION
BM from gynecologic cancer is rare (2%), but our findings suggest that the prognosis might not always be poor. In our small series, surgical resection with WBRT was a treatment modality significantly associated with a longer progression-free survival. Additional studies with more cases and multi-institutional cooperation are needed to determine which treatment modality leads to better outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim YZ, Kwon JH, Lim S. A clinical analysis of brain metastasis in gynecologic cancer: a retrospective multi-institute analysis. J Korean Med Sci. 2015; 30:66–73.
Article2. Nasu K, Satoh T, Nishio S, et al. Clinicopathologic features of brain metastases from gynecologic malignancies: a retrospective study of 139 cases (KCOG-G1001s trial). Gynecol Oncol. 2013; 128:198–203.
Article3. Ogawa K, Yoshii Y, Aoki Y, et al. Treatment and prognosis of brain metastases from gynecological cancers. Neurol Med Chir (Tokyo). 2008; 48:57–62. discussion 62-3.
Article4. Tangjitgamol S, Levenback CF, Beller U, Kavanagh JJ. Role of surgical resection for lung, liver, and central nervous system metastases in patients with gynecological cancer: a literature review. Int J Gynecol Cancer. 2004; 14:399–422.
Article5. Monaco E 3rd, Kondziolka D, Mongia S, Niranjan A, Flickinger JC, Lunsford LD. Management of brain metastases from ovarian and endometrial carcinoma with stereotactic radiosurgery. Cancer. 2008; 113:2610–2614.
Article6. Pakneshan S, Safarpour D, Tavassoli F, Jabbari B. Brain metastasis from ovarian cancer: a systematic review. J Neurooncol. 2014; 119:1–6.
Article7. Cormio G, Loizzi V, Falagario M, Lissoni AA, Resta L, Selvaggi LE. Changes in the management and outcome of central nervous system involvement from ovarian cancer since 1994. Int J Gynaecol Obstet. 2011; 114:133–136.
Article8. Anupol N, Ghamande S, Odunsi K, Driscoll D, Lele S. Evaluation of prognostic factors and treatment modalities in ovarian cancer patients with brain metastases. Gynecol Oncol. 2002; 85:487–492.
Article9. Clark TG, Stewart ME, Altman DG, Gabra H, Smyth JF. A prognostic model for ovarian cancer. Br J Cancer. 2001; 85:944–952.
Article10. Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2000; 70:209–262.11. Gilani MA, Williams NL, Giordano C, et al. Brain metastases in patients with gynecologic cancers: a single institution experience and review of the literature. Open J Obstet Gynecol. 2016; 6:544–552.
Article12. Cohen ZR, Suki D, Weinberg JS, et al. Brain metastases in patients with ovarian carcinoma: prognostic factors and outcome. J Neurooncol. 2004; 66:313–325.
Article13. Gadducci A, Tana R, Teti G, et al. Brain recurrences in patients with ovarian cancer: report of 12 cases and review of the literature. Anticancer Res. 2007; 27:4403–4409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Outcomes of Hemorrhagic Metastatic Brain Tumors
- Clinical Outcomes of Gamma Knife Radiosurgery for Metastatic Brain Tumors from Gynecologic Cancer : Prognostic Factors in Local Treatment Failure and Survival
- Metastsectomy a Feasible Treatment in Selected Patients with Gynecologic Malignancy
- Cutaneous Metastasis from Lung Cancer: A Single-Institution Retrospective Analysis
- A Clinical Analysis of Brain Metastasis in Gynecologic Cancer: A Retrospective Multi-institute Analysis