Proenkephalin, Neutrophil Gelatinase-Associated Lipocalin, and Estimated Glomerular Filtration Rates in Patients With Sepsis
- Affiliations
-
- 1Department of Laboratory Medicine, Konkuk University School of Medicine, Seoul, Korea. dearmina@hanmail.net
- 2School of Public Health, Seoul National University, Seoul, Korea.
- 3Department of Medical-Surgery Sciences and Translational Medicine, School of Medicine and Psychology, ‘Sapienza' University, Sant'Andrea Hospital, Rome, Italy. salvatore.disomma@uniroma1.it
- 4Department of Clinical Molecular Medicine, School of Medicine and Psychology, ‘Sapienza' University, Sant'Andrea Hospital, Rome, Italy.
- 5Sphingotec GmbH, Hennigsdorf, Germany.
- KMID: 2383914
- DOI: http://doi.org/10.3343/alm.2017.37.5.388
Abstract
- BACKGROUND
Proenkephalin (PENK) has been suggested as a novel biomarker for kidney function. We investigated the diagnostic and prognostic utility of plasma PENK in comparison with neutrophil gelatinase-associated lipocalin (NGAL) and estimated glomerular filtration rates (eGFR) in septic patients.
METHODS
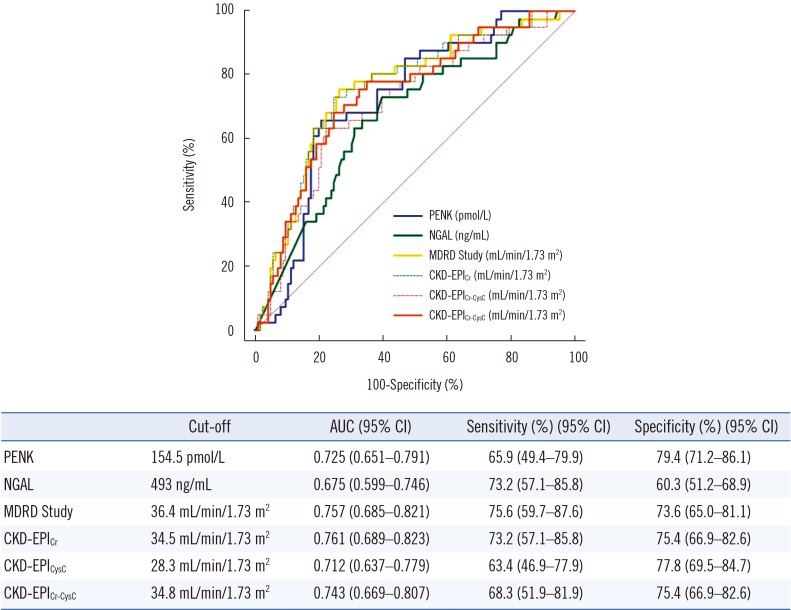
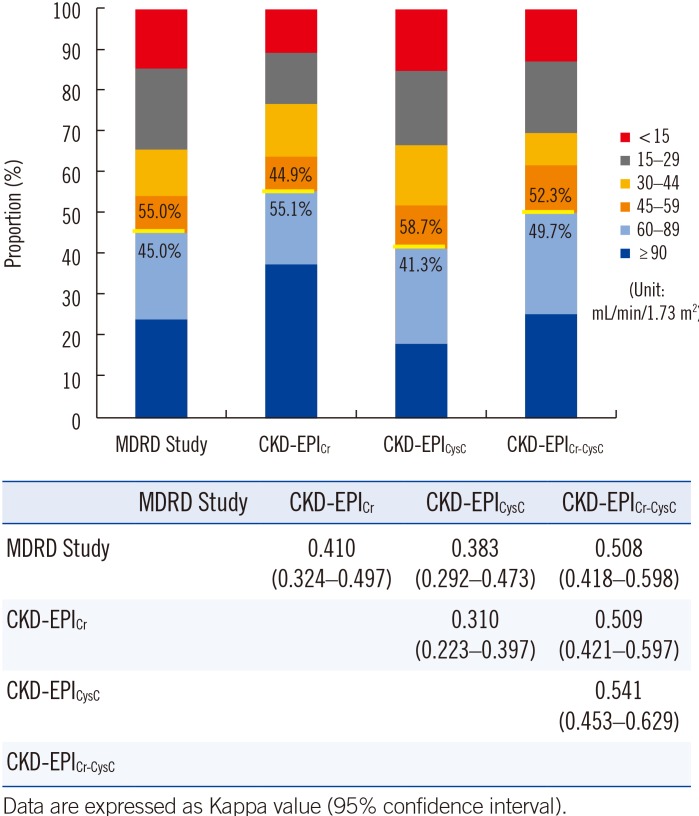
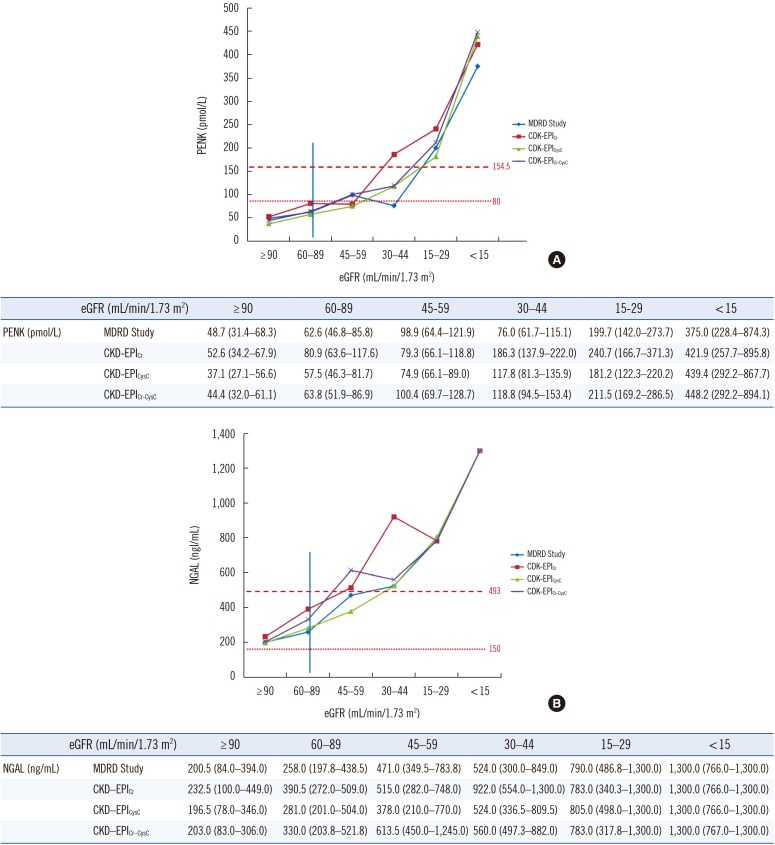
A total of 167 septic patients were enrolled: 99 with sepsis, 37 with septic shock, and 31 with suspected sepsis. PENK and NGAL concentrations were measured and GFR was estimated by using the isotope dilution mass spectrometry traceable-Modification of Diet in Renal Disease (MDRD) Study and three Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations: CKD-EPI(Cr), CDK-EPI(CysC), and CKD-EPI(Cr-CysC). The PENK, NGAL, and eGFR results were compared according to sepsis severity, presence or absence of acute kidney injury (AKI), and clinical outcomes.
RESULTS
The PENK, NGAL, and eGFR results were significantly associated with sepsis severity and differed significantly between patients with and without AKI only in the sepsis group (all P<0.05). PENK was superior to NGAL in predicting AKI (P=0.022) and renal replacement therapy (RRT) (P=0.0085). Regardless of the variable GFR category by the different eGFR equations, PENK showed constant and significant associations with all eGFR equations. Unlike NGAL, PENK was not influenced by inflammation and predicted the 30-day mortality.
CONCLUSIONS
PENK is a highly sensitive and objective biomarker of AKI and RRT and is useful for prognosis prediction in septic patients. With its diagnostic robustness and predictive power for survival, PENK constitutes a promising biomarker in critical care settings including sepsis.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Proenkephalin Predicts Organ Failure, Renal Replacement Therapy, and Mortality in Patients With Sepsis
Hanah Kim, Mina Hur, Joachim Struck, Andreas Bergmann, Salvatore Di Somma
Ann Lab Med. 2020;40(6):466-473. doi: 10.3343/alm.2020.40.6.466.Biomarker-Guided Risk Assessment for Acute Kidney Injury: Time for Clinical Implementation?
Christian Albert, Michael Haase, Annemarie Albert, Antonia Zapf, Rüdiger Christian Braun-Dullaeus, Anja Haase-Fielitz
Ann Lab Med. 2021;41(1):1-15. doi: 10.3343/alm.2021.41.1.1.Predictive Value of Plasma NGAL:Hepcidin-25 for Major Adverse Kidney Events After Cardiac Surgery with Cardiopulmonary Bypass: A Pilot Study
Christian Albert, Michael Haase, Annemarie Albert, Martin Ernst, Siegfried Kropf, Rinaldo Bellomo, Sabine Westphal, Rüdiger C. Braun-Dullaeus, Anja Haase-Fielitz, Saban Elitok
Ann Lab Med. 2021;41(4):357-365. doi: 10.3343/alm.2021.41.4.357.Plasma Neutrophil Gelatinase-Associated Lipocalin as a Marker of Tubular Damage in Diabetic Nephropathy
So Young Kim, Tae-Dong Jeong, Woochang Lee, Sail Chun, Sung Sunwoo, Soon Bae Kim, Won-Ki Min
Ann Lab Med. 2018;38(6):524-529. doi: 10.3343/alm.2018.38.6.524.Hepcidin and Neutrophil Gelatinase-Associated Lipocalin as a Biomarker for Acute Kidney Injury Linked Iron Metabolism
Sun Young Cho, Mina Hur
Ann Lab Med. 2020;40(2):97-98. doi: 10.3343/alm.2020.40.2.97.
Reference
-
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–810. PMID: 26903338.2. Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, et al. Acute kidney injury: an increasing global concern. Lancet. 2013; 382:170–179. PMID: 23727171.3. Rewa O, Bagshaw SM. Acute kidney injury-epidemiology, outcomes and economics. Nat Rev Nephrol. 2014; 10:193–207. PMID: 24445744.4. Honore PM, Jacobs R, Hendrickx I, Bagshaw SM, Joannes-Boyau O, Boer W, et al. Prevention and treatment of sepsis-induced acute kidney injury: an update. Ann Intensive Care. 2015; 5:51–60.5. Alobaidi R, Basu RK, Goldstein SL, Bagshaw SM. Sepsis-associated acute kidney injury. Semin Nephrol. 2015; 35:2–11. PMID: 25795495.6. Ichai C, Vinsonneau C, Souweine B, Armando F, Canet E, Clec'h C, et al. Acute kidney injury in the perioperative period and in intensive care units (excluding renal replacement therapies). Ann Intensive Care. 2016; 6:48. PMID: 27230984.7. Ronco C, Legrand M, Goldstein SL, Hur M, Tran N, Howell EC, et al. Neutrophil gelatinase-associated lipocalin: ready for routine clinical use? An international perspective. Blood Purif. 2014; 37:271–285. PMID: 25012891.8. Zhang A, Cai Y, Wang PF, Qu JN, Luo ZC, Chen XD, et al. Diagnosis and prognosis of neutrophil gelatinase-associated lipocalin for acute kidney injury with sepsis: a systematic review and meta-analysis. Crit Care. 2016; 20:41. PMID: 26880194.9. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130:461–470. PMID: 10075613.10. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–612. PMID: 19414839.11. Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012; 367:20–29. PMID: 22762315.12. Hoste EA, Damen J, Vanholder RC, Lameire NH, Delanghe JR, Van den, et al. Assessment of renal function in recently admitted critically ill patients with normal serum creatinine. Nephrol Dial Transplant. 2005; 20:747–753. PMID: 15701668.13. Shah KS, Taub P, Patel M, Rehfeldt M, Struck J, Clopton P, et al. Proenkephalin predicts acute kidney injury in cardiac surgery patients. Clin Nephrol. 2015; 83:29–35. PMID: 25512100.14. Marino R, Struck J, Hartmann O, Maisel AS, Rehfeldt M, Magrini L, et al. Diagnostic and short-term prognostic utility of plasma pro-enkephalin (pro-ENK) for acute kidney injury in patients admitted with sepsis in the emergency department. J Nephrol. 2015; 28:717–724. PMID: 25486879.15. Schulz CA, Christensson A, Ericson U, Almgren P, Hindy G, Nilsson PM, et al. High level of fasting plasma proenkephalin-A predicts deterioration of kidney function and incidence of CKD. J Am Soc Nephrol. 2017; 28:291–303. PMID: 27401687.16. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637. PMID: 23353941.17. The Kidney Disease Improving Global Outcomes (KDIGO) Working Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012; 2:1–138.18. Persson M, Berglund G, Nelson JJ, Hedblad B. Lp-PLA2 activity and mass are associated with increased incidence of ischemic stroke: a population-based cohort study from Malmö, Sweden. Atherosclerosis. 2008; 200:191–198. PMID: 18201705.19. Kidney Disease Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3:1–150.20. Muller MP, Tomlinson G, Marrie TJ, Tang P, McGeer A, Low DE, et al. Can routine laboratory tests discriminate between severe acute respiratory syndrome and other causes of community-acquired pneumonia? Clin Infect Dis. 2005; 40:1079–1086. PMID: 15791504.21. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012; 22:276–282. PMID: 23092060.22. Zhu Y, Ye X, Zhu B, Pei X, Wei L, Wu J, et al. Comparisons between the 2012 new CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equations and other four approved equations. PLoS One. 2014; 9:e84688. PMID: 24454737.23. Ronco C. Acute kidney injury: from clinical to molecular diagnosis. Crit Care. 2016; 20:201. PMID: 27384344.24. Romanovsky A, Morgan C, Bagshaw SM. Pathophysiology and management of septic acute kidney injury. Pediatr Nephrol. 2014; 29:1–12. PMID: 23400860.25. Schrier RW, Wang W. Acute renal failure and sepsis. N Engl J Med. 2004; 351:159–169. PMID: 15247356.26. Gomez H, Ince C, De Backer D, Pickkers P, Payen D, Hotchkiss J, et al. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaption to injury. Shock. 2014; 41:3–11.27. Arbit B, Marston N, Shah K, Lee EL, Aramin H, Clopton P, et al. Prognostic usefulness of proenkephalin in stable ambulatory patients with heart failure. Am J Cardiol. 2016; 117:1310–1314. PMID: 26916537.28. Ng LL, Sandhu JK, Narayan H, Quinn PA, Squire IB, Davies JE, et al. Proenkephalin and prognosis after acute myocardial infarction. J Am Coll Cardiol. 2014; 63:280–289. PMID: 24140658.29. Murray PT, Mehta RL, Shaw A, Ronco C, Endre Z, Kellum JA, et al. Potential use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th Acute Dialysis Quality Initiative consensus conference. Kidney Int. 2014; 85:513–521. PMID: 24107851.30. Otto GP, Hurtado-Oliveros J, Chung HY, Knoll K, Neumann T, Müller HJ, et al. Plasma neutrophil gelatinase-associated lipocalin is primarily related to inflammation during sepsis: a translational approach. PLoS One. 2015; 10:e0124429. PMID: 25893429.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urinary Neutrophil Gelatinase-Associated Lipocalin Levels in Comparison with Glomerular Filtration Rate for Evaluation of Renal Function in Patients with Diabetic Chronic Kidney Disease
- Hepcidin and Neutrophil Gelatinase-Associated Lipocalin as a Biomarker for Acute Kidney Injury Linked Iron Metabolism
- Novel Early Predictor of Acute Kidney Injury after Open Heart Surgery under Cadiopulmonary Bypass Using Plasma Neutrophil Gelatinase-Associated Lipocalin
- Evolution of glomerular filtration rates and neutrophil gelatinase-associated lipocalin during treatment with direct acting antivirals
- Plasma Neutrophil Gelatinase-Associated Lipocalin as a Marker of Tubular Damage in Diabetic Nephropathy