Ann Lab Med.
2018 Nov;38(6):524-529. 10.3343/alm.2018.38.6.524.
Plasma Neutrophil Gelatinase-Associated Lipocalin as a Marker of Tubular Damage in Diabetic Nephropathy
- Affiliations
-
- 1Department of Laboratory Medicine, LabGenomics Clinical Laboratory, Seongnam, Korea.
- 2Department of Laboratory Medicine, College of Medicine, Ewha Womans University, Seoul, Korea.
- 3Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. sailchun@amc.seoul.kr
- 4Department of Family Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- 5Department of Internal Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- KMID: 2429117
- DOI: http://doi.org/10.3343/alm.2018.38.6.524
Abstract
- BACKGROUND
An increase in neutrophil gelatinase-associated lipocalin (NGAL) indicates tubular injury. Diabetic nephropathy causes typical changes in the kidney, characterized by glomerulosclerosis and eventual tubular damage. We validated the usefulness of plasma NGAL (pNGAL) as a biomarker of tubular damage in patients with diabetic nephropathy.
METHODS
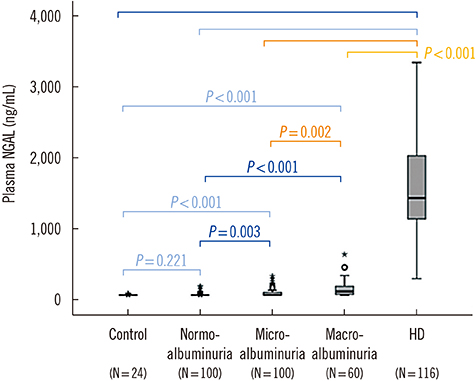
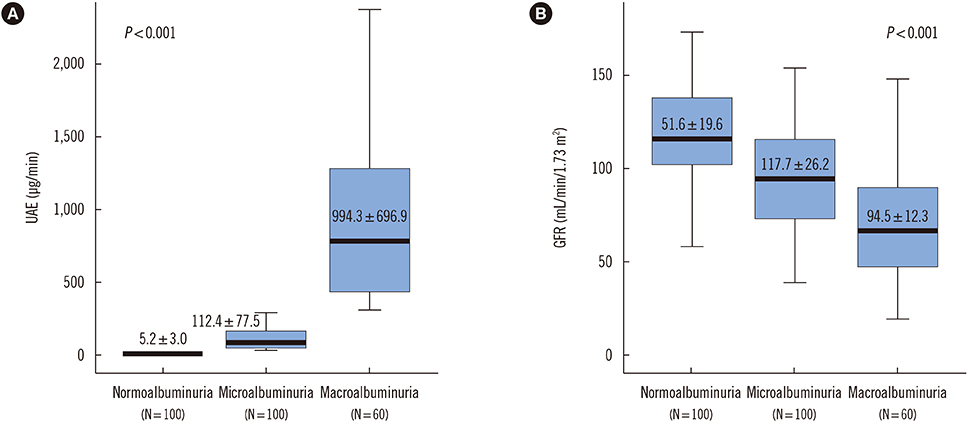
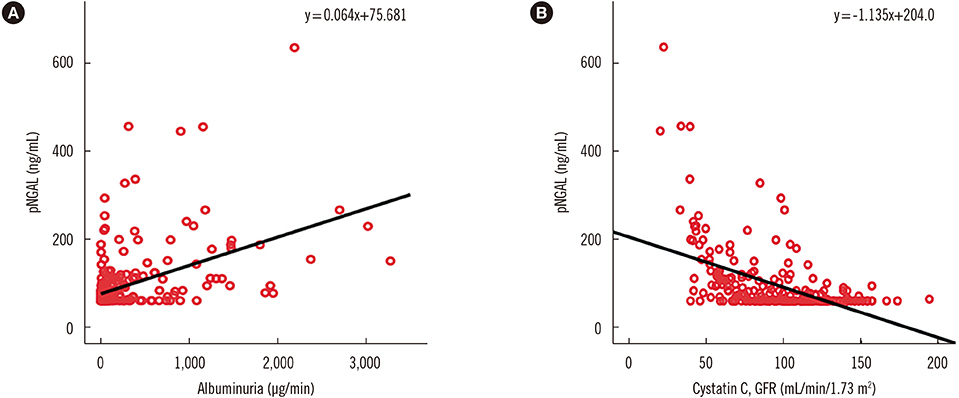
We included 376 patients with diabetes mellitus (260 patients with chronic renal insufficiency who had not received hemodialysis and 116 hemodialyzed due to diabetic nephropathy) and 24 healthy controls. Patients with chronic renal insufficiency were divided into three groups according to urinary albumin excretion (UAE) levels. pNGAL levels were measured using the Triage NGAL test (Alere, San Diego, CA, USA) and were compared between groups. We also examined whether pNGAL level was related to the degree of albuminuria and cystatin C-based glomerular filtration rate (GFR).
RESULTS
Mean pNGAL levels of the healthy controls, chronic renal insufficiency patients with diabetes mellitus, and hemodialyzed patients were 61.9±5.3 ng/mL, 93.4±71.8 ng/mL, and 1,536.9±554.9 ng/mL, respectively. pNGAL level increased significantly in patients with severe albuminuria (P < 0.001) and had a moderate correlation with the degree of albuminuria (r=0.467; P < 0.001) and GFR (r=0.519; P < 0.001). Multivariate regression analysis showed that the pNGAL level was associated with tubular damage independent of patient age, sex, and GFR.
CONCLUSIONS
pNGAL level independently reflects the degree of tubular damage in patients with diabetic nephropathy. Measurement of pNGAL, combined with UAE, would enable simultaneous, highly reliable assessments of tubular damage for such patients.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Effectiveness of Plasma and Urine Neutrophil Gelatinase-Associated Lipocalin for Predicting Acute Kidney Injury in High-Risk Patients
Ahram Yi, Chang-Hoon Lee, Yeo-Min Yun, Hanah Kim, Hee-Won Moon, Mina Hur
Ann Lab Med. 2021;41(1):60-67. doi: 10.3343/alm.2021.41.1.60.Biomarker-Guided Risk Assessment for Acute Kidney Injury: Time for Clinical Implementation?
Christian Albert, Michael Haase, Annemarie Albert, Antonia Zapf, Rüdiger Christian Braun-Dullaeus, Anja Haase-Fielitz
Ann Lab Med. 2021;41(1):1-15. doi: 10.3343/alm.2021.41.1.1.
Reference
-
1. Devarajan P. NGAL in acute kidney injury: from serendipity to utility. Am J Kidney Dis. 2008; 52:395–399.
Article2. Bolignano D, Coppolino G, Romeo A, De Paola L, Buemi A, Lacquaniti A, et al. Neutrophil gelatinase-associated lipocalin (NGAL) reflects iron status in haemodialysis patients. Nephrol Dial Transplant. 2009; 24:3398–3403.
Article3. Gilbert RE, Cooper ME. The tubulointerstitium in progressive diabetic kidney disease: more than an aftermath of glomerular injury? Kidney Int. 1999; 56:1627–1637.
Article4. Nielsen SE, Andersen S, Zdunek D, Hess G, Parving HH, Rossing P. Tubular markers do not predict the decline in glomerular filtration rate in type 1 diabetic patients with overt nephropathy. Kidney Int. 2011; 79:1113–1118.
Article5. Nielsen SE, Schjoedt KJ, Astrup AS, Tarnow L, Lajer M, Hansen PR, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule 1 (KIM1) in patients with diabetic nephropathy: a cross-sectional study and the effects of lisinopril. Diabet Med. 2010; 27:1144–1150.
Article6. Finne P, Reunanen A, Stenman S, Groop PH, Gronhagen-Riska C. Incidence of end-stage renal disease in patients with type 1 diabetes. JAMA. 2005; 294:1782–1787.
Article7. Bolignano D, Lacquaniti A, Coppolino G, Donato V, Fazio MR, Nicocia G, et al. Neutrophil gelatinase-associated lipocalin as an early biomarker of nephropathy in diabetic patients. Kidney Blood Press Res. 2009; 32:91–98.
Article8. Nielsen SE, Hansen HP, Jensen BR, Parving HH, Rossing P. Urinary neutrophil gelatinase-associated lipocalin and progression of diabetic nephropathy in type 1 diabetic patients in a four-year follow-up study. Nephron Clin Pract. 2011; 118:c130–c135.
Article9. Bolignano D, Lacquaniti A, Coppolino G, Donato V, Campo S, Fazio MR, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin J Am Soc Nephrol. 2009; 4:337–344.
Article10. Phillips AO. The role of renal proximal tubular cells in diabetic nephropathy. Curr Diab Rep. 2003; 3:491–496.
Article11. Di Somma S, Magrini L, De Beradinis B, Marino R, Ferri E, Moscatelli P, et al. Additive value of blood neutrophil gelatinase-associated lipocalin to clinical judgement in acute kidney injury diagnosis and mortality prediction in patients hospitalized from the emergency department. Crit Care. 2013; 17:R29.
Article12. Hur M, Kim H, Lee S, Cristofano F, Magrini L, Marino R, et al. Diagnostic and prognostic utilities of multimarkers approach using procalcitonin, B-type natriuretic peptide, and neutrophil gelatinase-associated lipocalin in critically ill patients with suspected sepsis. BMC Infect Dis. 2014; 14:224.
Article13. Kim H, Hur M, Lee S, Marino R, Magrini L, Cardelli P, et al. Proenkephalin, neutrophil gelatinase-associated lipocalin, and estimated glomerular filtration rates in patients with sepsis. Ann Lab Med. 2017; 37:388–397.
Article14. Malyszko J, Malyszko JS, Koc-Zorawska E, Kozminski P, Mysliwiec M. Neutrophil gelatinase-associated lipocalin in dialyzed patients is related to residual renal function, type of renal replacement therapy and inflammation. Kidney Blood Press Res. 2009; 32:464–469.
Article15. Musial K, Zwolinska D. Neutrophil gelatinase-associated lipocalin (NGAL) and matrix metalloproteinases as novel stress markers in children and young adults on chronic dialysis. Cell Stress Chaperones. 2011; 16:163–171.16. Bolignano D, Coppolino G, Romeo A, Lacquaniti A, Buemi M. Neutrophil gelatinase-associated lipocalin levels in chronic haemodialysis patients. Nephrology (Carlton). 2010; 15:23–26.
Article17. Kusaka M, Kuroyanagi Y, Mori T, Nagaoka K, Sasaki H, Maruyama T, et al. Serum neutrophil gelatinase-associated lipocalin as a predictor of organ recovery from delayed graft function after kidney transplantation from donors after cardiac death. Cell Transplant. 2008; 17:129–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Plasma Neutrophil Gelatinase-Associated Lipocalin as a Biomarker for Tubular Damage in Diabetic Nephropathy
- Plasma Neutrophil Gelatinase-associated Lipocalin and Leukocyte Differential Count in Children with Febrile Urinary Tract Infection
- Urinary Neutrophil Gelatinase-Associated Lipocalin Levels in Comparison with Glomerular Filtration Rate for Evaluation of Renal Function in Patients with Diabetic Chronic Kidney Disease
- Hepcidin and Neutrophil Gelatinase-Associated Lipocalin as a Biomarker for Acute Kidney Injury Linked Iron Metabolism
- Plasma Neutrophil Gelatinase-associated Lipocalin is an Early Marker of Acute Kidney Injury