Child Kidney Dis.
2021 Dec;25(2):84-91. 10.3339/jkspn.2021.25.2.84.
Plasma Neutrophil Gelatinase-associated Lipocalin and Leukocyte Differential Count in Children with Febrile Urinary Tract Infection
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- KMID: 2524510
- DOI: http://doi.org/10.3339/jkspn.2021.25.2.84
Abstract
- Purpose
We aimed to study the association of plasma neutrophil gelatinase-associated lipocalin (pNGAL) and leukocyte differential count in children with febrile urinary tract infection (UTI).
Methods
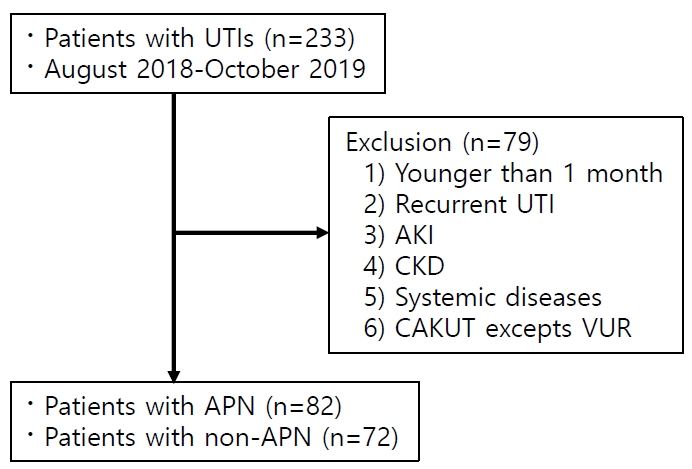
Medical records of 154 children aged 1 month to 13 years with febrile UTI who were hospitalized were retrospectively reviewed. Associations between pNGAL levels and blood leukocyte differential count at admission and after 48 hours of treatment were investigated in children with or without acute pyelonephritis (APN).
Results
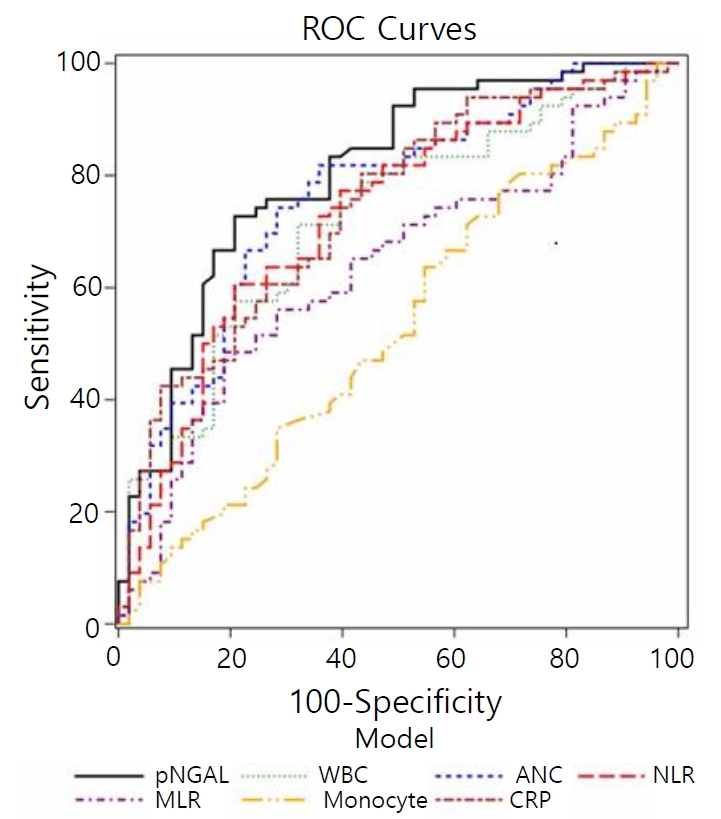
The APN group (n=82) showed higher pNGAL levels, neutrophil count, monocyte count, and neutrophil-to-lymphocyte ratio (NLR), compared to the non-APN group (n=72) (all P<0.05). After adjustment for age and sex, pNGAL showed positive correlations with neutrophil count and NLR in both groups (all P<0.05). Additionally, it was correlated with the monocyte-to-lymphocyte ratio (MLR) only in the APN group (P<0.05). Before and after treatment, pNGAL was positively correlated with neutrophil count, NLR, and MLR in patients with APN while it was related with neutrophil count and NLR in those without APN (all P<0.05). Areas under the receiver operating curve of pNGAL, neutrophil count, NLR, and MLR for predicting APN were 0.804, 0.760, 0.730, and 0.636, respectively (all P<0.05). Only pNGAL was independently associated with the presence of APN in a multivariable logistic regression analysis (P<0.05).
Conclusion
In children with febrile UTIs, pNGAL might be associated with leukocyte differential count and the presence of APN.
Keyword
Figure
Reference
-
References
1. Montini G, Tullus K, Hewitt I. Febrile urinary tract infections in children. N Engl J Med. 2011; 365:239–50.
Article2. Morello W, La Scola C, Alberici I, Montini G. Acute pyelonephritis in children. Pediatr Nephrol. 2016; 31:1253–65.
Article3. Yilmaz A, Sevketoglu E, Gedikbasi A, Karyagar S, Kiyak A, Mulazimoglu M, et al. Early prediction of urinary tract infection with urinary neutrophil gelatinase associated lipocalin. Pediatr Nephrol. 2009; 24:2387–92.
Article4. Yim HE, Yim H, Bae ES, Woo SU, Yoo KH. Predictive value of urinary and serum biomarkers in young children with febrile urinary tract infections. Pediatr Nephrol. 2014; 29:2181–9.
Article5. Kass EJ, Kernen KM, Carey JM. Paediatric urinary tract infection and the necessity of complete urological imaging. BJU Int. 2000; 86:94–6.
Article6. Naess A, Nilssen SS, Mo R, Eide GE, Sjursen H. Role of neutrophil to lymphocyte and monocyte to lymphocyte ratios in the diagnosis of bacterial infection in patients with fever. Infection. 2017; 45:299–307.
Article7. Witter AR, Okunnu BM, Berg RE. The Essential role of neutrophils during infection with the intracellular bacterial pathogen Listeria monocytogenes. J Immunol. 2016; 197:1557–65.8. Ingersoll MA, Platt AM, Potteaux S, Randolph GJ. Monocyte trafficking in acute and chronic inflammation. Trends Immunol. 2011; 32:470–7.
Article9. Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017; 10:12.
Article10. Han SY, Lee IR, Park SJ, Kim JH, Shin JI. Usefulness of neutrophillymphocyte ratio in young children with febrile urinary tract infection. Korean J Pediatr. 2016; 59:139–44.
Article11. Wang JL, Lu XY, Xu XH, Zhang KJ, Gong H, Lv D, et al. Predictive role of monocyte-to-lymphocyte ratio in patients with Klebsiella pneumonia infection: a single-center experience. Medicine (Baltimore). 2019; 98:e17215.12. Ichino M, Kuroyanagi Y, Kusaka M, Mori T, Ishikawa K, Shiroki R, et al. Increased urinary neutrophil gelatinase associated lipocalin levels in a rat model of upper urinary tract infection. J Urol. 2009; 181:2326–31.
Article13. Krzemien G, Panczyk-Tomaszewska M, Adamczuk D, Kotula I, Demkow U, Szmigielska A. Neutrophil gelatinase-associated lipocalin: a biomarker for early diagnosis of urinary tract infections in infants. Adv Exp Med Biol. 2018; 1047:71–80.14. Kim BK, Yim HE, Yoo KH. Plasma neutrophil gelatinase-associated lipocalin: a marker of acute pyelonephritis in children. Pediatr Nephrol. 2017; 32:477–84.
Article15. Jang JW, Yim HE, Yoo KH. Association of neutrophil gelatinase associated lipocalin and leukocyte differential count in children with febrile urinary tract infections. Child Kidney Dis. 2020; 24:83–90.
Article16. Subcommittee on Urinary Tract Infection SCoQI, Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011; 128:595–610.
Article17. Jaksic E, Bogdanovic R, Artiko V, Saranovic DS, Petrasinovic Z, Petrovic M, et al. Diagnostic role of initial renal cortical scintigraphy in children with the first episode of acute pyelonephritis. Ann Nucl Med. 2011; 25:37–43.
Article18. Schmidt-Ott KM, Mori K, Li JY, Kalandadze A, Cohen DJ, Devarajan P, et al. Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 2007; 18:407–13.
Article19. Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat Immunol. 2006; 7:311–7.
Article20. Serbina NV, Hohl TM, Cherny M, Pamer EG. Selective expansion of the monocytic lineage directed by bacterial infection. J Immunol. 2009; 183:1900–10.
Article21. Condron C, Toomey D, Casey RG, Shaffii M, Creagh T, BouchierHayes D. Neutrophil bactericidal function is defective in patients with recurrent urinary tract infections. Urol Res. 2003; 31:329–34.
Article22. de Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010; 14:1–8.
Article23. Xu SY, Carlson M, Engstrom A, Garcia R, Peterson CG, Venge P. Purification and characterization of a human neutrophil lipocalin (HNL) from the secondary granules of human neutrophils. Scand J Clin Lab Invest. 1994; 54:365–76.
Article24. Berger T, Togawa A, Duncan GS, Elia AJ, You-Ten A, Wakeham A, et al. Lipocalin 2-deficient mice exhibit increased sensitivity to Escherichia coli infection but not to ischemia-reperfusion injury. Proc Natl Acad Sci USA. 2006; 103:1834–9.
Article25. Ratledge C, Dover LG. Iron metabolism in pathogenic bacteria. Annu Rev Microbiol. 2000; 54:881–941.
Article26. Faraldo-Gomez JD, Sansom MS. Acquisition of siderophores in gram-negative bacteria. Nat Rev Mol Cell Biol. 2003; 4:105–16.
Article27. Nguyen MT, Devarajan P. Biomarkers for the early detection of acute kidney injury. Pediatr Nephrol. 2008; 23:2151–7.
Article28. Flo TH, Smith KD, Sato S, Rodriguez DJ, Holmes MA, Strong RK, et al. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature. 2004; 432:917–21.
Article29. Nasioudis D, Witkin SS. Neutrophil gelatinase-associated lipocalin and innate immune responses to bacterial infections. Med Microbiol Immunol. 2015; 204:471–9.
Article30. Kim JW, Hong DY, Lee KR, Kim SY, Baek KJ, Park SO. Usefulness of plasma neutrophil gelatinase-associated lipocalin concentration for predicting the severity and mortality of patients with community-acquired pneumonia. Clin Chim Acta. 2016; 462:140–5.
Article31. Guiddir T, Deghmane AE, Giorgini D, Taha MK. Lipocalin 2 in cerebrospinal fluid as a marker of acute bacterial meningitis. BMC Infect Dis. 2014; 14:1–8.
Article32. Sim JH, Yim HE, Choi BM, Lee JH, Yoo KH. Plasma neutrophil gelatinase-associated lipocalin predicts acute pyelonephritis in children with urinary tract infections. Pediatr Res. 2015; 78:48–55.
Article33. Lee JH, Yim HE, Yoo KH. Associations of plasma neutrophil gelatinase-associated lipocalin, anemia, and renal scarring in children with febrile urinary tract infections. J Korean Med Sci. 2020; 35:e65.
Article34. Moon JH, Yoo KH, Yim HE. Urinary neutrophil gelatinase-associated lipocalin: a marker of urinary tract infection among febrile children. Clin Exp Pediatr. 2020.
Article35. Kim B, Myung R, Kim J, Lee MJ, Pai H. Descriptive epidemiology of acute pyelonephritis in Korea, 2010-2014: Population-based Study. J Korean Med Sci. 2018; 33:e310.
Article36. Elkharrat D, Chastang C, Boudiaf M, Le Corre A, Raskine L, Caulin C. Relevance in the emergency department of a decisional algorithm for outpatient care of women with acute pyelonephritis. Eur J Emerg Med. 1999; 6:15–20.37. Tenner SM, Yadven MW, Kimmel PL. Acute pyelonephritis - preventing complications through prompt diagnosis and proper therapy. Postgrad Med. 1992; 91:261–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Neutrophil Gelatinase associated Lipocalin and Leukocyte Differential Count in Children with Febrile Urinary Tract Infections
- Plasma Neutrophil Gelatinase-Associated Lipocalin as a Predictor of Renal Parenchymal Involvement in Infants With Febrile Urinary Tract Infection: A Preliminary Study
- Urinary neutrophil gelatinase-associated lipocalin: a marker of urinary tract infection among febrile children
- Associations of Plasma Neutrophil Gelatinase-associated Lipocalin, Anemia, and Renal Scarring in Children with Febrile Urinary Tract Infections
- Evaluation of the Optimal Neutrophil Gelatinase-Associated Lipocalin Value as a Screening Biomarker for Urinary Tract Infections in Children