World J Mens Health.
2016 Dec;34(3):165-172. 10.5534/wjmh.2016.34.3.165.
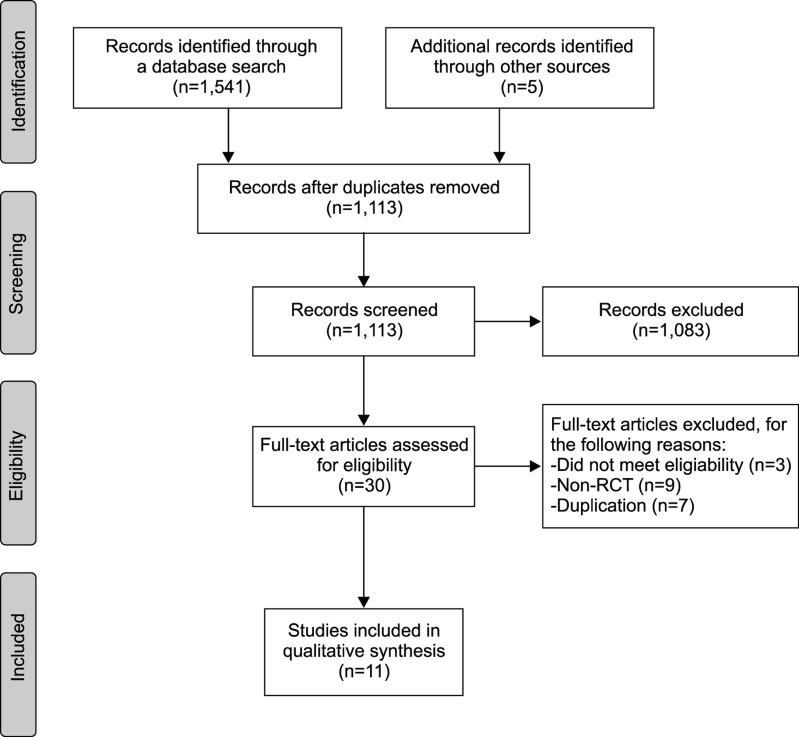
Treatment of Leukocytospermia in Male Infertility: A Systematic Review
- Affiliations
-
- 1Department of Urology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 2Institute of Evidence Based Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Yonsei Wonju Medical Library, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 4Department of Plastic Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Division of Gastroenterology and Hepatology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 6Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 7Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 8Department of Urology, Cheil General Hospital and Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea. jtandro@cgh.co.kr
- KMID: 2364198
- DOI: http://doi.org/10.5534/wjmh.2016.34.3.165
Abstract
- Male factors account for 20% to 50% of infertility cases, and infection in the genitourinary tract may play a contributing role in up to 15% of male infertility. Leukocytospermia is a well-known indicator of infection or inflammation in the male sex glands and the urogenital tract. Although great deal of effort has been expended to elucidate definite management strategies in infertile men with leukocytospermia, the gold standard of treatment remains unclear. Until recently, broad spectrum antibiotics and antioxidants have been used in the treatment of leukocytospermia for male infertility to eliminate infection and reduce reactive oxygen free radicals produced inside cellular mitochondria as a result of inflammation. The present review reveals that antibiotics might improve sperm parameters, the rate of resolution of leukocytospermia, the bacteriologic cure rate, and even the pregnancy rate, although some reports conflict. Antioxidants might also have clinical benefits for sperm function as shown by in vitro studies. However, the data are insufficient to conclude whether antibiotics and antioxidants for the treatment of infertile men with leukocytospermia are effective or not. Better designed investigations into leukocytospermia are needed.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Oxidation-reduction potential as a new marker for oxidative stress: Correlation to male infertility
Ashok Agarwal, Albert Danh Bui
Investig Clin Urol. 2017;58(6):385-399. doi: 10.4111/icu.2017.58.6.385.Review of Guidelines for the Evaluation and Treatment of Leukocytospermia in Male Infertility
Robert J. Brunner, Jonathan H. Demeter, Puneet Sindhwani
World J Mens Health. 2019;37(2):128-137. doi: 10.5534/wjmh.180078.
Reference
-
1. Gnoth C, Godehardt E, Frank-Herrmann P, Friol K, Tigges J, Freundl G. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005; 20:1144–1147. PMID: 15802321.
Article2. Sandoval JS, Raburn D, Muasher S. Leukocytospermia: overview of diagnosis, implications, and management of a controversial finding. Middle East Fertil Soc J. 2013; 18:129–134.
Article3. World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: World Health Organization;2010.4. Aziz N, Agarwal A, Lewis-Jones I, Sharma RK, Thomas AJ Jr. Novel associations between specific sperm morphological defects and leukocytospermia. Fertil Steril. 2004; 82:621–627. PMID: 15374705.
Article5. Lackner JE, Herwig R, Schmidbauer J, Schatzl G, Kratzik C, Marberger M. Correlation of leukocytospermia with clinical infection and the positive effect of antiinflammatory treatment on semen quality. Fertil Steril. 2006; 86:601–605. PMID: 16782098.
Article6. Tomlinson MJ, White A, Barratt CL, Bolton AE, Cooke ID. The removal of morphologically abnormal sperm forms by phagocytes: a positive role for seminal leukocytes? Hum Reprod. 1992; 7:517–522. PMID: 1522196.
Article7. Pentyala S, Lee J, Annam S, Alvarez J, Veerraju A, Yadlapalli N, et al. Current perspectives on pyospermia: a review. Asian J Androl. 2007; 9:593–600. PMID: 17712476.
Article8. Skau PA, Folstad I. Do bacterial infections cause reduced ejaculate quality? A meta-analysis of antibiotic treatment of male infertility. Behav Ecol. 2003; 14:40–47.
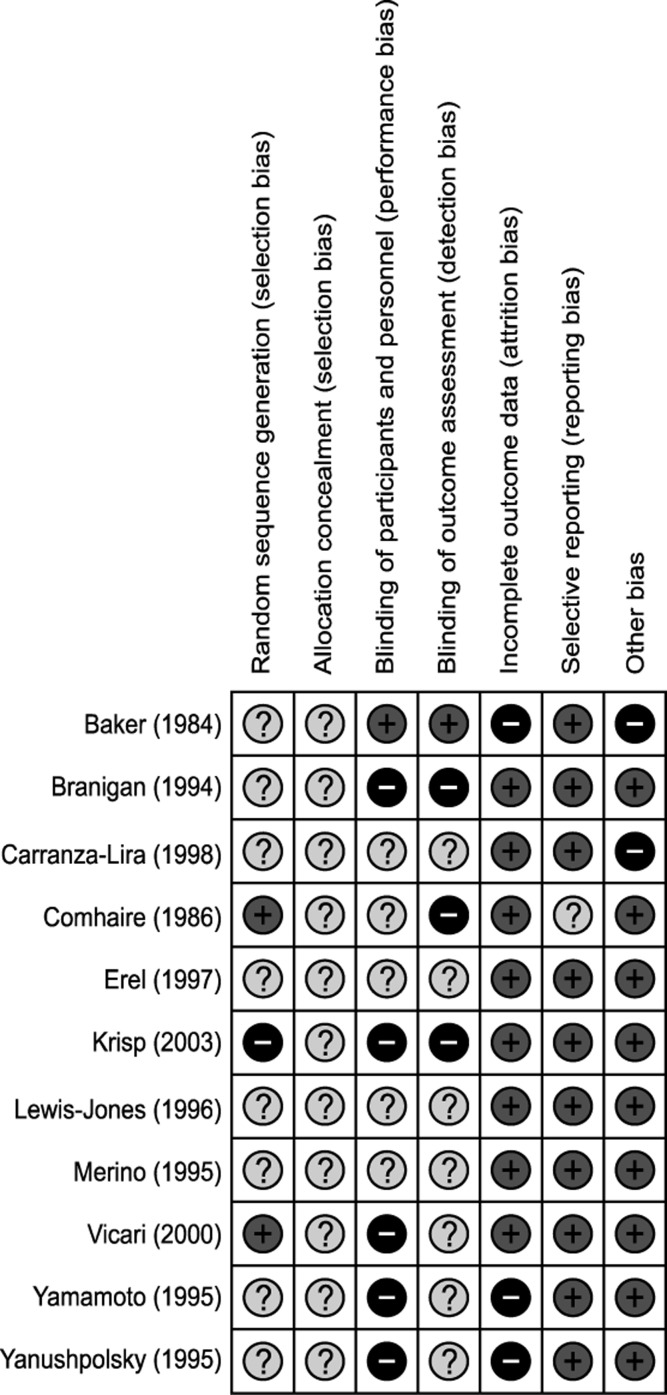
Article9. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. PMID: 22008217.
Article10. Baker HW, Straffon WG, McGowan MP, Burger HG, de Kretser DM, Hudson B. A controlled trial of the use of erythromycin for men with asthenospermia. Int J Androl. 1984; 7:383–388. PMID: 6396236.
Article11. Comhaire FH, Rowe PJ, Farley TM. The effect of doxycycline in infertile couples with male accessory gland infection: a double blind prospective study. Int J Androl. 1986; 9:91–98. PMID: 3539821.
Article12. Branigan EF, Muller CH. Efficacy of treatment and recurrence rate of leukocytospermia in infertile men with prostatitis. Fertil Steril. 1994; 62:580–584. PMID: 7520396.13. Merino G, Carranza-Lira S. Infection and male infertility: effect of different antibiotic regimens on semen quality. Arch Androl. 1995; 35:209–212. PMID: 8585775.
Article14. Yamamoto M, Hibi H, Katsuno S, Miyake K. Antibiotic and ejaculation treatments improve resolution rate of leukocytospermia in infertile men with prostatitis. Nagoya J Med Sci. 1995; 58:41–45. PMID: 7659146.15. Yanushpolsky EH, Politch JA, Hill JA, Anderson DJ. Antibiotic therapy and leukocytospermia: a prospective, randomized, controlled study. Fertil Steril. 1995; 63:142–147. PMID: 7805903.16. Lewis-Jones DI, Kynaston HG, Lynch RV, Desmond AD, Entwistle PA. Antibiotic treatment of leucospermia in subfertile males. Arch STD/HIV Res. 1996; 10:65–72.17. Erel CT, Sentürk LM, Demir F, Irez T, Ertüngealp E. Antibiotic therapy in men with leukocytospermia. Int J Fertil Womens Med. 1997; 42:206–210. PMID: 9222805.18. Carranza-Lira S, Tserotas K, Morán C, Merino G, Barahona E, Bermúdez JA. Effect of antibiotic therapy in asthenozoospermic men associated with increased agglutination and minimal leukospermia. Arch Androl. 1998; 40:159–162. PMID: 9507749.
Article19. Vicari E. Effectiveness and limits of antimicrobial treatment on seminal leukocyte concentration and related reactive oxygen species production in patients with male accessory gland infection. Hum Reprod. 2000; 15:2536–2544. PMID: 11098023.
Article20. Krisp A, Hörster S, Skrzypek J, Krause W. Treatment with levofloxacin does not resolve asymptomatic leucocytospermia: a randomized controlled study. Andrologia. 2003; 35:244–247. PMID: 12950410.21. Endtz AW. A rapid staining method for differentiating granulocytes from “germinal cells” in Papanicolaou-stained semen. Acta Cytol. 1974; 18:2–7. PMID: 4129934.22. Aitken RJ, Clarkson JS. Significance of reactive oxygen species and antioxidants in defining the efficacy of sperm preparation techniques. J Androl. 1988; 9:367–376. PMID: 3215823.
Article23. Lewin A, Lavon H. The effect of coenzyme Q10 on sperm motility and function. Mol Aspects Med. 1997; 18(Suppl):S213–S219. PMID: 9266524.
Article24. Oeda T, Henkel R, Ohmori H, Schill WB. Scavenging effect of N-acetyl-L-cysteine against reactive oxygen species in human semen: a possible therapeutic modality for male factor infertility? Andrologia. 1997; 29:125–131. PMID: 9197915.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of Guidelines for the Evaluation and Treatment of Leukocytospermia in Male Infertility
- Comparision of Conventional IVF and ICSI for Leukocytospermia
- Genetic Causes in Male Infertility and Current Studies on Infertility Genes
- Clinical correlation among male infertility and overall male health: A systematic review of the literature
- Association of triclosan and human infertility: A systematic review