Korean J Radiol.
2015 Dec;16(6):1341-1348. 10.3348/kjr.2015.16.6.1341.
Prediction of Response to Concurrent Chemoradiotherapy with Temozolomide in Glioblastoma: Application of Immediate Post-Operative Dynamic Susceptibility Contrast and Diffusion-Weighted MR Imaging
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul 03080, Korea. verocay@snuh.org
- 2Center for Nanoparticle Research, Institute for Basic Science, and School of Chemical and Biological Engineering, Seoul National University, Seoul 08826, Korea.
- 3Department of Internal Medicine, Cancer Research Institute, Seoul National University College of Medicine, Seoul 03080, Korea.
- 4Department of Neurosurgery, Seoul National University College of Medicine, Seoul 03080, Korea.
- 5Department of Pathology, Seoul National University College of Medicine, Seoul 03080, Korea.
- 6Department of Radiation Oncology, Cancer Research Institute, Seoul National University College of Medicine, Seoul 03080, Korea.
- KMID: 2344290
- DOI: http://doi.org/10.3348/kjr.2015.16.6.1341
Abstract
OBJECTIVE
To determine whether histogram values of the normalized apparent diffusion coefficient (nADC) and normalized cerebral blood volume (nCBV) maps obtained in contrast-enhancing lesions detected on immediate post-operative MR imaging can be used to predict the patient response to concurrent chemoradiotherapy (CCRT) with temozolomide (TMZ).
MATERIALS AND METHODS
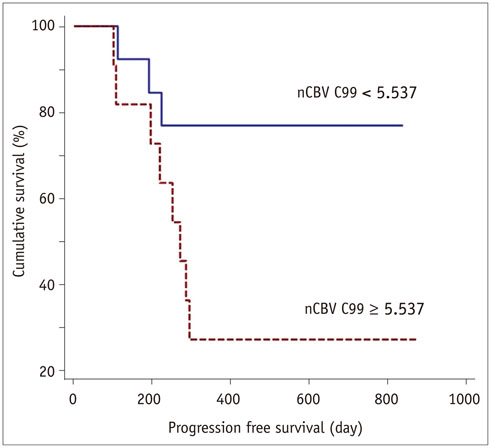
Twenty-four patients with GBM who had shown measurable contrast enhancement on immediate post-operative MR imaging and had subsequently undergone CCRT with TMZ were retrospectively analyzed. The corresponding histogram parameters of nCBV and nADC maps for measurable contrast-enhancing lesions were calculated. Patient groups with progression (n = 11) and non-progression (n = 13) at one year after the operation were identified, and the histogram parameters were compared between the two groups. Receiver operating characteristic (ROC) analysis was used to determine the best cutoff value for predicting progression. Progression-free survival (PFS) was determined with the Kaplan-Meier method and the log-rank test.
RESULTS
The 99th percentile of the cumulative nCBV histogram (nCBV C99) on immediate post-operative MR imaging was a significant predictor of one-year progression (p = 0.033). ROC analysis showed that the best cutoff value for predicting progression after CCRT was 5.537 (sensitivity and specificity were 72.7% and 76.9%, respectively). The patients with an nCBV C99 of < 5.537 had a significantly longer PFS than those with an nCBV C99 of ≥ 5.537 (p = 0.026).
CONCLUSION
The nCBV C99 from the cumulative histogram analysis of the nCBV from immediate post-operative MR imaging may be feasible for predicting glioblastoma response to CCRT with TMZ.
Keyword
MeSH Terms
-
Adult
Aged
Antineoplastic Agents, Alkylating/*therapeutic use
Brain/pathology/radiography
Brain Neoplasms/*drug therapy/mortality/radiography
Chemoradiotherapy
Dacarbazine/*analogs & derivatives/therapeutic use
Diffusion Magnetic Resonance Imaging
Disease Progression
Disease-Free Survival
Female
Glioblastoma/*drug therapy/mortality/radiography
Humans
Kaplan-Meier Estimate
Male
Middle Aged
Proportional Hazards Models
ROC Curve
Retrospective Studies
Antineoplastic Agents, Alkylating
Dacarbazine
Figure
Cited by 2 articles
-
Diffusion Tensor-Derived Properties of Benign Oligemia, True “at Risk” Penumbra, and Infarct Core during the First Three Hours of Stroke Onset: A Rat Model
Fang-Ying Chiu, Duen-Pang Kuo, Yung-Chieh Chen, Yu-Chieh Kao, Hsiao-Wen Chung, Cheng-Yu Chen
Korean J Radiol. 2018;19(6):1161-1171. doi: 10.3348/kjr.2018.19.6.1161.Evaluation of Tumor Blood Flow Using Alternate Ascending/Descending Directional Navigation in Primary Brain Tumors: A Comparison Study with Dynamic Susceptibility Contrast Magnetic Resonance Imaging
Hyeree Park, Joonhyuk Lee, Sung-Hong Park, Seung Hong Choi
Korean J Radiol. 2019;20(2):275-282. doi: 10.3348/kjr.2018.0300.
Reference
-
1. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.2. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352:987–996.3. Ekinci G, Akpinar IN, Baltacioğlu F, Erzen C, Kiliç T, Elmaci I, et al. Early-postoperative magnetic resonance imaging in glial tumors: prediction of tumor regrowth and recurrence. Eur J Radiol. 2003; 45:99–107.4. Forsyth PA, Petrov E, Mahallati H, Cairncross JG, Brasher P, MacRae ME, et al. Prospective study of postoperative magnetic resonance imaging in patients with malignant gliomas. J Clin Oncol. 1997; 15:2076–2081.5. Henegar MM, Moran CJ, Silbergeld DL. Early postoperative magnetic resonance imaging following nonneoplastic cortical resection. J Neurosurg. 1996; 84:174–179.6. Albert FK, Forsting M, Sartor K, Adams HP, Kunze S. Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Neurosurgery. 1994; 34:45–60. discussion 60-617. Vidiri A, Carapella CM, Pace A, Mirri A, Fabi A, Carosi M, et al. Early post-operative MRI: correlation with progression-free survival and overall survival time in malignant gliomas. J Exp Clin Cancer Res. 2006; 25:177–182.8. Smets T, Lawson TM, Grandin C, Jankovski A, Raftopoulos C. Immediate post-operative MRI suggestive of the site and timing of glioblastoma recurrence after gross total resection: a retrospective longitudinal preliminary study. Eur Radiol. 2013; 23:1467–1477.9. Nakamura H, Murakami R, Hirai T, Kitajima M, Yamashita Y. Can MRI-derived factors predict the survival in glioblastoma patients treated with postoperative chemoradiation therapy? Acta Radiol. 2013; 54:214–220.10. Knopp EA, Cha S, Johnson G, Mazumdar A, Golfinos JG, Zagzag D, et al. Glial neoplasms: dynamic contrast-enhanced T2*-weighted MR imaging. Radiology. 1999; 211:791–198.11. Felix R, Schörner W, Laniado M, Niendorf HP, Claussen C, Fiegler W, et al. Brain tumors: MR imaging with gadolinium-DTPA. Radiology. 1985; 156:681–688.12. Law M, Young RJ, Babb JS, Peccerelli N, Chheang S, Gruber ML, et al. Gliomas: predicting time to progression or survival with cerebral blood volume measurements at dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. Radiology. 2008; 247:490–498.13. Charles-Edwards EM, deSouza NM. Diffusion-weighted magnetic resonance imaging and its application to cancer. Cancer Imaging. 2006; 6:135–143.14. Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, et al. Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol. 2010; 28:1963–1972.15. Rosen BR, Belliveau JW, Vevea JM, Brady TJ. Perfusion imaging with NMR contrast agents. Magn Reson Med. 1990; 14:249–265.16. Ostergaard L, Weisskoff RM, Chesler DA, Gyldensted C, Rosen BR. High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part I: Mathematical approach and statistical analysis. Magn Reson Med. 1996; 36:715–725.17. Boxerman JL, Schmainda KM, Weisskoff RM. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol. 2006; 27:859–867.18. Wetzel SG, Cha S, Johnson G, Lee P, Law M, Kasow DL, et al. Relative cerebral blood volume measurements in intracranial mass lesions: interobserver and intraobserver reproducibility study. Radiology. 2002; 224:797–803.19. Bjornerud A. The ICE software package: direct co-registration of anatomical and functional datasets using DICOM image geometry information. Proc Hum Brain Mapping. 2003; 19:1018p.20. Kim H, Choi SH, Kim JH, Ryoo I, Kim SC, Yeom JA, et al. Gliomas: application of cumulative histogram analysis of normalized cerebral blood volume on 3 T MRI to tumor grading. PLoS One. 2013; 8:e63462.21. Kang Y, Choi SH, Kim YJ, Kim KG, Sohn CH, Kim JH, et al. Gliomas: Histogram analysis of apparent diffusion coefficient maps with standard- or high-b-value diffusion-weighted MR imaging--correlation with tumor grade. Radiology. 2011; 261:882–890.22. Song YS, Choi SH, Park CK, Yi KS, Lee WJ, Yun TJ, et al. True progression versus pseudoprogression in the treatment of glioblastomas: a comparison study of normalized cerebral blood volume and apparent diffusion coefficient by histogram analysis. Korean J Radiol. 2013; 14:662–772.23. Chu HH, Choi SH, Ryoo I, Kim SC, Yeom JA, Shin H, et al. Differentiation of true progression from pseudoprogression in glioblastoma treated with radiation therapy and concomitant temozolomide: comparison study of standard and high-b-value diffusion-weighted imaging. Radiology. 2013; 269:831–840.24. Mangla R, Singh G, Ziegelitz D, Milano MT, Korones DN, Zhong J, et al. Changes in relative cerebral blood volume 1 month after radiation-temozolomide therapy can help predict overall survival in patients with glioblastoma. Radiology. 2010; 256:575–584.25. Farace P, Amelio D, Ricciardi GK, Zoccatelli G, Magon S, Pizzini F, et al. Early MRI changes in glioblastoma in the period between surgery and adjuvant therapy. J Neurooncol. 2013; 111:177–185.26. Yamasaki F, Sugiyama K, Ohtaki M, Takeshima Y, Abe N, Akiyama Y, et al. Glioblastoma treated with postoperative radio-chemotherapy: prognostic value of apparent diffusion coefficient at MR imaging. Eur J Radiol. 2010; 73:532–537.27. Huisman TA, Loenneker T, Barta G, Bellemann ME, Hennig J, Fischer JE, et al. Quantitative diffusion tensor MR imaging of the brain: field strength related variance of apparent diffusion coefficient (ADC) and fractional anisotropy (FA) scalars. Eur Radiol. 2006; 16:1651–1658.28. Qin W, Yu CS, Zhang F, Du XY, Jiang H, Yan YX, et al. Effects of echo time on diffusion quantification of brain white matter at 1.5 T and 3.0 T. Magn Reson Med. 2009; 61:755–760.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of the Effectiveness and Safety of Temozolomide during and after Radiotherapy for Newly Diagnosed Glioblastomas: 10-year Experience of a Single Institution
- Added Value of Contrast Leakage Information over the CBV Value of DSC Perfusion MRI to Differentiate between Pseudoprogression and True Progression after Concurrent Chemoradiotherapy in Glioblastoma Patients
- Multidisciplinary Functional MR Imaging for Prostate Cancer
- Emerging Techniques in Brain Tumor Imaging: What Radiologists Need to Know
- Preoperative Prediction of Ductal Carcinoma in situ Underestimation of the Breast using Dynamic Contrast Enhanced and Diffusion-weighted Imaging