Tuberc Respir Dis.
2006 Oct;61(4):330-338.
Relationship between Systemic Inflammatory Marker, Oxidative Stress and Body Mass Index in Stable COPD Patient
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University, Jinju, Korea. hochkim@gshp.gsnu.ac.kr
- 2Department of Pediatrics, College of Medicine, Gyeongsang National University, Jinju, Korea.
- 3Gyeongsang Institute of Health Sciences, Gyeongsang National University, Jinju, Korea.
- 4Department of Anatomy, Medical School of Chungbuk National University, Chungju, Korea.
Abstract
-
BACKGROUND: The main factors associated with weight loss in patients with COPD are not well known. Since chronic inflammation and oxidative stress play a major pathogenic role in COPD, these factors may be responsible for the patients' weight loss. Therefore, this study measured the body mass index (BMI) in COPD patients and evaluated the variables, such as systemic inflammatory marker, oxidative stress and lung function, that correlate with the BMI.
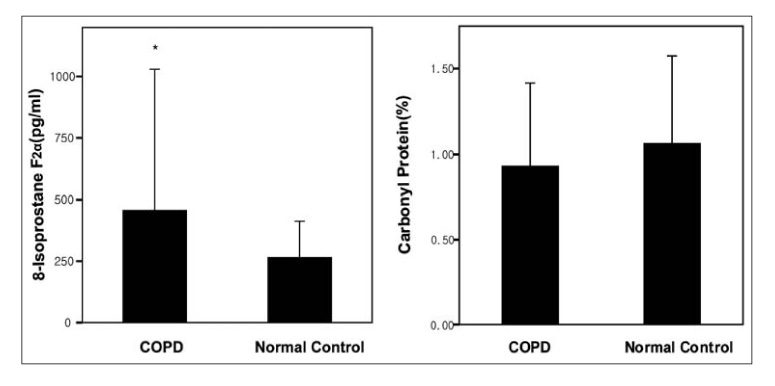
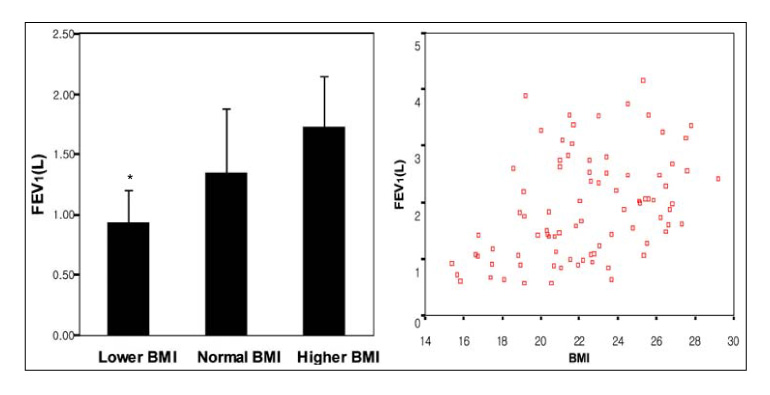
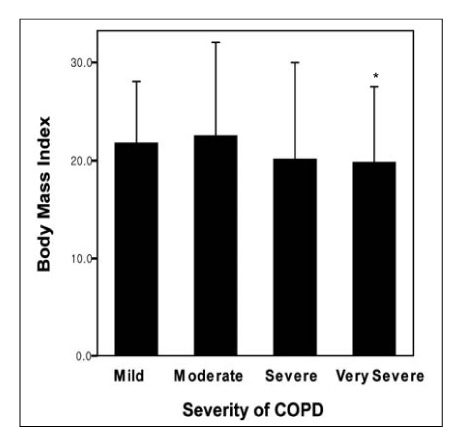
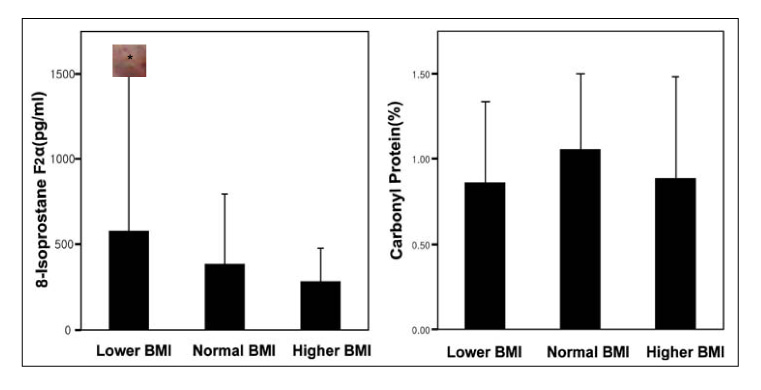
METHOD: The stable COPD patients (M:F=49:4, mean age=68.25+/-6.32) were divided into the lower (<18.5), normal (18.5-25) and higher (>25) BMI group. The severity of the airway obstruction was evaluated by measuring the FEV1. The serum IL-6 and TNF-alpha levels were measured to determine the degree of systemic inflammation, and the carbonyl protein and 8-iso-prostaglandin F2alpha level was measured to determine the level of oxidative stress. Each value in the COPD patients and normal control was compared with the BMI.
RESULTS
1) Serum 8-iso-prostaglandin F2alpha in COPD patients was significantly higher (456.08+/-574.12 pg/ml) than that in normal control (264.74+/-143.15 pg/ml) (p<0.05). However, there were no significant differences in the serum IL-6, TNF-alpha, carbonyl protein between the COPD patients and normal controls. 2). In the COPD patients, the FEV1 of the lower BMI group was significantly lower (0.93+/-0.25L) than that of the normal BMI (1.34+/-0.52L) and higher BMI groups (1.72+/-0.41L) (p<0.05). The lower FEV1 was significantly associated with a lower BMI in COPD patients (p=0.002, r=0.42). The BMI of very severe COPD patients was significantly lower (19.8+/-2.57) than that of the patients with moderate COPD (22.6+/-3.14) (p<0.05). 3). There were no significant differences in the serum IL-6, TNF-alpha, carbonyl protein and 8-iso-prostaglandin F2alpha according to the BMI in the COPD patients.
CONCLUSION
The severity of the airway obstruction, not the systemic inflammatory markers and oxidative stress, might be associated with the BMI in stable COPD patients. Further study will be needed to determine the factors associated with the decrease in the BMI of COPD patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Global Initiative for Chronic Obstructive Lung Disease. National Institutes of Health Publication Number 2701. NHLBI/WHO, Workshop report. 2001.2. MacNee W. Pathogenesis of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:258–266.3. Spurzem JR, Rennard SI. Pathogenesis of COPD. Semin Respir Crit Care Med. 2005. 26:142–153.4. MacNee W. Pulmonary and systemic oxidant/antioxidant imbalance in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:50–60.5. Agusti AG, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003. 21:347–360.6. Couillard A, Prefaut C. From muscle disuse to myopathy in COPD: potential contribution of oxidative stress. Eur Respir J. 2005. 26:703–719.7. Agust AG, Gari PG, Sauleda J, Busquets X. Weight loss in chronic obstructive pulmonary disease: mechanisms and implications. Pulm Pharmacol Ther. 2002. 15:425–432.8. Dolan S, Varkey B. Prognostic factors in chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2005. 11:149–152.9. Celli BR, Cote CG, Martin JM, Casanova C, Montes de, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004. 350:1005–1012.10. Schols AM, Soeters PB, Dingemans AM, Mostert R, Frantzen PJ, Wouters EF. Prevalence and characteristics of nutritional depletion in patients with stable COPD; eligible for pulmonary rehabilitation. Am Rev Respir Dis. 1993. 147:1151–1156.11. di Francia M, Barbier D, Mege JL, Orehek J. Tumor necrosis factor-alpha levels and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994. 150:1453–1455.12. de Godoy I, Donahoe M, Calhoun WJ, Mancino J, Rogers RM. Elevated TNF-a production by peripheral blood monocytes of weight-losing COPD patients. Am J Respir Crit Care Med. 1996. 153:633–637.13. Song W, Zhao Z, Li Z. Interleukin-6 in bronchoalveolar lavage fluid from patients with COPD. Chin Med J. 2001. 114:1140–1142.14. Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, et al. Relationship of interleukin-6 and tumor necrosis factor-α with muscle mass and muscle strength in elderly men and women. J Gerontol A Biol Sci Med Sci. 2002. 57:M326–M332.15. Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J Suppl. 2003. 41:46s–53s.16. Expert Panel on the Identification, Evaluation and Treatment of Overweight in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Am J Clin Nutr. 1998. 68:899–917.17. Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R. Protein carbonyl groups as biomarkers of oxidative stress. Clin Chim Acta. 2003. 329:23–38.18. Janssen LJ. Isoprostanes: an overview and putative roles in pulmonary pathophysiology. Am J Physiol Lung Cell Mol Physiol. 2001. 280:L1067–L1082.19. Biernacki WA, Kharitonov SA, Barnes PJ. Increased leukotriene B4 and 8-isoprostane in exhaled breath condensate of patients with exacerbations of COPD. Thorax. 2003. 58:294–298.20. Praticò D, Basili S, Vieri M, Cordova C, Violi F, Fitzgerald GA. Chronic obstructive pulmonary disease is associated with an increase in urinary levels of isoprostane F 2a-III, an index of oxidant stress. Am J Respir Crit Care Med. 1998. 158:1709–1714.21. Wouters EF. Local and systemic inflammation in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:26–33.22. Malo O, Sauleda J, Busquets X, Miralles C, Agusti AG, Noguera A. Systemic inflammation during exacerbations of chronic obstructive pulmonary disease. Arch Bronconeumol. 2002. 38:172–176.23. Takabatake N, Nakamura H, Abe S, Inoue S, Hino T, Saito H, et al. The relationship between chronic hypoxemia and activation of the tumor necrosis factor-α system in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000. 161:1179–1184.24. Petrovsky N, Harrison LC. The chronobiology of human cytokine production. Int Rev Immunol. 1998. 16:635–649.25. Dalle-Donne I, Giustarini D, Colombo R, Rossi R, Milzani A. Protein carbonylation in human diseases. Trends Mol Med. 2003. 9:169–176.26. Barreiro E, de la Puente B, Minguella J, Corominas JM, Serrano S, Hussain SN, et al. Oxidative stress and respiratory muscle dysfunction in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005. 171:1116–1124.27. Barreiro E, Gea J, Corominas JM, Hussain SN. Nitric oxide synthases and protein oxidation in the quadriceps femoris of patients with chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2003. 29:771–778.28. Karadag F, Karul AB, Cildag O, Altun C, Gurgey O. Determinants of BMI in patients with COPD. Respirology. 2004. 9:70–75.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Increased Proportion of Apoptosis in CD4⺠T Lymphocytes Isolated from the Peripheral Blood in Patients with Stable Chronic Obstructive Pulmonary Disease
- Plasma Adropin as a Potential Marker Predicting Obesity and Obesity-associated Cancer in Korean Patients With Type 2 Diabetes Mellitus
- Relationships among Oxidative Stress Markers, Life Style Factors and Biochemical Findings
- Usefulness of neutrophil to lymphocyte ratio in patients with chronic obstructive pulmonary disease: a prospective observational study
- Role of Nuclear Factor Erythroid 2-Related Factor 2 in Chronic Obstructive Pulmonary Disease