Pediatr Allergy Respir Dis.
2012 Dec;22(4):422-427.
A Case of Pulmonary Hemosiderosis that was Dissolved by an Oral Prednisolone and the Milk Avoidance
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. dongings0@snu.ac.kr
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
Abstract
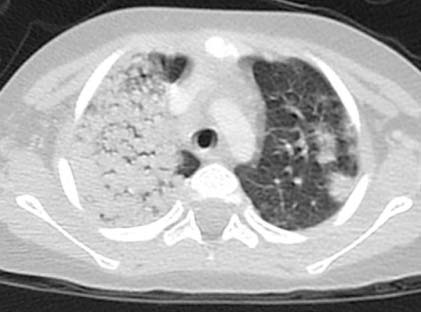
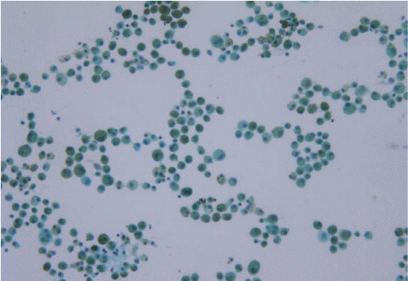
- A 29-month-old boy presented with fever, dyspnea, and paleness. He was initially diagnosed with pneumonia and severe sepsis. Although he was treated with intravenous antibiotics and high dose methylprednisolone, dyspnea and paleness recurred two times. Under suspicion of pulmonary hemosiderosis, we performed video-assisted thoracoscopic lung biopsy and bronchoalveolar lavage on him and found hemosiderin-laden macrophages in both specimens. Despite thorough history and laboratory examination, we could not find any pathologic or serologic evidence for primary and secondary causes of pulmonary hemosiderosis except for one that indicating Heiner's syndrome. After taking oral prednisolone he showed improvement of anemia and dyspnea, which was maintained by milk avoidance. Based on the history and the existence of immunoglobulin G antibodies against milk components, we are considering it as the case of Heiner's syndrome.
MeSH Terms
-
Anemia
Anti-Bacterial Agents
Antibodies
Biopsy
Bronchoalveolar Lavage
Dyspnea
Fever
Hemosiderosis
Immunoglobulin G
Lung
Lung Diseases
Macrophages
Methylprednisolone
Milk
Milk Hypersensitivity
Pneumonia
Prednisolone
Sepsis
Anti-Bacterial Agents
Antibodies
Hemosiderosis
Immunoglobulin G
Lung Diseases
Methylprednisolone
Prednisolone
Figure
Reference
-
1. You SK, Kim KS, Kim YJ, Koh YY. Two cases of idiopathic pulmonary hemosiderosis. J Korean Pediatr Soc. 1988. 31:1209–1216.2. Kjellman B, Elinder G, Garwicz S, Svan H. Idiopathic pulmonary haemosiderosis in Swedish children. Acta Paediatr Scand. 1984. 73:584–588.
Article3. Ohga S, Takahashi K, Miyazaki S, Kato H, Ueda K. Idiopathic pulmonary haemosiderosis in Japan: 39 possible cases from a survey questionnaire. Eur J Pediatr. 1995. 154:994–995.
Article4. Lim CS, Park SK, Park W, Lee SJ, Jung CZ. A case of idiopathic pulmonary hemosiderosis. J Korean Pediatr Soc. 1996. 39:136–141.5. Kwon YS, Kim JH, Lim DH, Kim SK, Chung SW, Son BK. A case of idiopathic pulmonary hemosiderosis improved with steroid inhalation. J Korean Pediatr Soc. 1998. 41:1153–1156.6. Park JS, Pyun BY, Kim YT. A case of idiopathic pulmonary hemosiderosis: long term follow-up. Pediatr Allergy Respir Dis. 1999. 9:226–232.7. Kwak GY, Lee NY, Lee MH, Lee SY, Chung SY, Kang JH, et al. A case of idiopathic pulmonary hemosiderosis with seasonal recurrence. Korean J Pediatr. 2009. 52:256–260.
Article8. Kiper N, Gocmen A, Ozcelik U, Dilber E, Anadol D. Long-term clinical course of patients with idiopathic pulmonary hemosiderosis (1979-1994): prolonged survival with low-dose corticosteroid therapy. Pediatr Pulmonol. 1999. 27:180–184.
Article9. Nuesslein TG, Teig N, Rieger CH. Pulmonary haemosiderosis in infants and children. Paediatr Respir Rev. 2006. 7:45–48.
Article10. Kabra SK, Bhargava S, Lodha R, Satyavani A, Walia M. Idiopathic pulmonary hemosiderosis: clinical profile and follow up of 26 children. Indian Pediatr. 2007. 44:333–338.11. Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: diagnosing it and finding the cause. Cleve Clin J Med. 2008. 75:258–280.
Article12. Moissidis I, Chaidaroon D, Vichyanond P, Bahna SL. Milk-induced pulmonary disease in infants (Heiner syndrome). Pediatr Allergy Immunol. 2005. 16:545–552.
Article13. Mansoor DK, Sharma HP. Clinical presentations of food allergy. Pediatr Clin North Am. 2011. 58:315–326.
Article14. Fiocchi A, Brozek J, Schünemann H, Bahna SL, von Berg A, Beyer K, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines. World Allergy Organ J. 2010. 3:57–161.
Article15. Torres MJ, Giron MD, Corzo JL, Rodriguez F, Moreno F, Perez E, et al. Release of inflammatory mediators after cow's milk intake in a newborn with idiopathic pulmonary hemosiderosis. J Allergy Clin Immunol. 1996. 98:1120–1123.
Article16. Sethi GR, Singhal KK. Pulmonary diseases and corticosteroids. Indian J Pediatr. 2008. 75:1045–1056.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Idiopathic Pulmonary Hemosiderosis
- A Case of Idiopathic Pulmonary Hemosiderosis Improved with Steroid Inhalation
- Three Cases of Pulmonary Hemosiderosis with Long-term Treatment of Deflazacort in Children
- A case of idiopathic pulmonary hemosiderosis with seasonal recurrence
- Two Cases of Idiopathic pulmonary Hemosiderosis