J Dent Anesth Pain Med.
2016 Mar;16(1):25-29. 10.17245/jdapm.2016.16.1.25.
Intranasal administration of dexmedetomidine (DEX) as a premedication for pediatric patients undergoing general anesthesia for dental treatment
- Affiliations
-
- 1Department of Pediatric Dentistry, School of Dentistry, Dankook University, Cheonan, Korea. jbkim0222@dankook.ac.kr
- 2Department of Anesthesiology, School of Dentistry, Dankook University, Cheonan, Korea.
- KMID: 2308762
- DOI: http://doi.org/10.17245/jdapm.2016.16.1.25
Abstract
- BACKGROUND
The most important reason for pre-operative administration of medication is to reduce anxiety. Alleviation of fear and anxiety about surgery enables patients to remain comfortable during treatment. Dexmedetomidine (DEX) is a fast-acting drug that is used as a premedication in different circumstances because it has sedative and anti-anxiolytic effects, and stable hemodynamics. It also has the advantage of intranasal administration. The aim of this study was to investigate the effects and hemodynamic stability of DEX by retrospectively analyzing cases in which DEX was administered nasally as a premedication.
METHODS
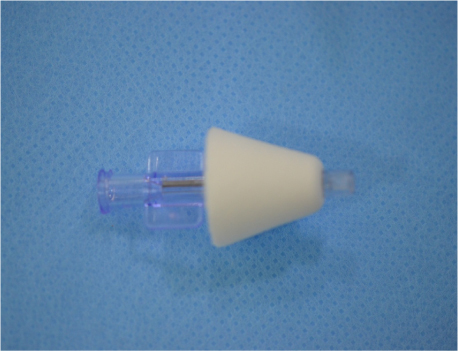
Ten patients treated at Dankook University Dental Hospital, recruited between February and April 2015, received intranasal delivery of 2 µg/kg DEX, 30 minutes prior to general anesthesia. Anesthesia records of anxiety, blood pressure, respiration, pulse, estimated arterial oxygen saturation (SpO2), and partial pressure, or maximum concentration, of carbon dioxide (ETCO2) were analyzed.
RESULTS
Administration of DEX prior to a general anesthetic effectively relieved anxiety. Respiratory depression, the most severe adverse effect of other sedatives, was not observed. Hemodynamic stability under general anesthesia was maintained during treatment and a reduction in emergence delirium was observed upon completion of treatment.
CONCLUSIONS
Premedication administration of DEX is safe for pediatric patients undergoing dental treatment under general anesthesia.
Keyword
MeSH Terms
-
Administration, Intranasal*
Anesthesia
Anesthesia, General*
Anesthetics
Anxiety
Blood Pressure
Carbon Dioxide
Delirium
Dexmedetomidine*
Hemodynamics
Humans
Hypnotics and Sedatives
Oxygen
Partial Pressure
Premedication*
Respiration
Respiratory Insufficiency
Retrospective Studies
Anesthetics
Carbon Dioxide
Dexmedetomidine
Hypnotics and Sedatives
Oxygen
Figure
Cited by 1 articles
-
Analysis of the effect of oral midazolam and triazolam premedication before general anesthesia in patients with disabilities with difficulty in cooperation
Seon Woo Lim, Eunsun So, Hye Joo Yun, Myong-Hwan Karm, Juhea Chang, Hanbin Lee, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2018;18(4):245-254. doi: 10.17245/jdapm.2018.18.4.245.
Reference
-
1. Linares Segovia B, García Cuevas MA, Ramírez Casillas IL, Guerrero Romero JF, Botello Buenrostro I, Monroy Torres R, Ramírez Gómez XS, et al. Pre-anaesthetic medication with intranasal dexmedetomidine and oral midazolam as an anxiolytic. A clinical trial. An Pediatr (Barc). 2014; 81:226–231.
Article2. Mahmoud M, Mason K. Dexmedetomidine: review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br J Anaesth. 2015; 115:171–182.
Article3. Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001; 14:13.4. Jayaraman L, Sinha A, Punhani D. A comparative study to evaluate the effect of intranasal dexmedetomidine versus oral alprazolam as a premedication agent in morbidly obese patients undergoing bariatric surgery. J Anaesthesiol Clin Pharmacol. 2013; 29:179.5. Korean Academy of Pediatric Dentistry. Pediatric Dentistry. 5th ed. Seoul: Dental Wisdom;2014.6. Kim J, Kim S, Lee DW, Ryu DS. The alternative of oral sedation for pediatric dental care. J Dent Anesth Pain Med. 2015; 15:1–4.7. Ambi US, Joshi C, Ganeshnavar A, Adarsh E. Intranasal dexmedetomidine for paediatric sedation for diagnostic magnetic resonance imaging studies. Indian J Anaesth. 2012; 56:587.8. Liu Y, Kang DL, Na HY, Li BL, Xu YY, Ni J, et al. Consequence of dexmedetomidine on emergence delirium following sevoflurane anesthesia in children with cerebral palsy. Int J Clin Exp Med. 2015; 8:16238.9. Hussain AA. Mechanism of nasal absorption of drugs. Prog Clin Biol Res. 1988; 292:261–272.10. Kupietzky A, Houpt MI. Midazolam: A review of its use for conscious sedation in children. Pediatr Dent. 1993; 15:237. 241.11. Hartgraves PM, Primosch RE. An evaluation of oral and nasal midazolam for pediatric dental sedation. ASDC J Dent Child. 1993; 61:175–181.
Article12. Song YG, Lee SY, Kim S. Use of midazolam intranasal spray for dental treatment of autism patients. J Korean Dent Soc Anesthesiol. 2012; 12:223–227.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intranasally Administered Adjunctive Dexmedetomidine Reduces Perioperative Anesthetic Requirements in General Anesthesia
- The alternative of oral sedation for pediatric dental care
- Sedation with dexmedetomidine in elderly patients during dental surgery: a retrospective case series
- Intravenous versus perineural dexmedetomidine as adjuvant in adductor canal block for total knee arthroplasty
- Efficacy of intranasal sedation for pediatric dental procedures: a systematic review and meta-analysis