Blood Res.
2013 Sep;48(3):222-225. 10.5045/br.2013.48.3.222.
A case of myelodysplastic syndrome with marked eosinophilia showing favorable prognosis
- Affiliations
-
- 1Department of Laboratory Medicine, Daegu Catholic University School of Medicine, Daegu, Korea. sgkim@cu.ac.kr
- KMID: 2270710
- DOI: http://doi.org/10.5045/br.2013.48.3.222
Abstract
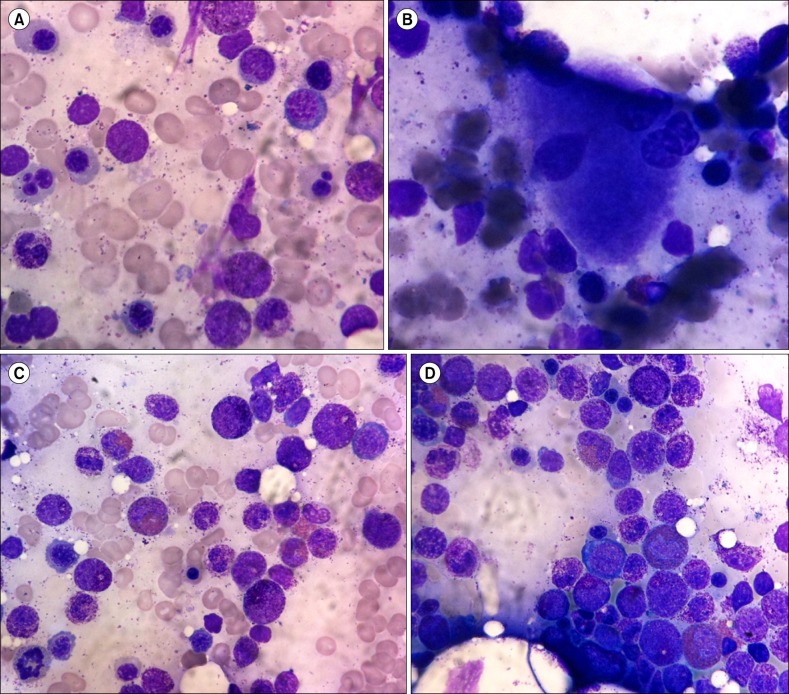
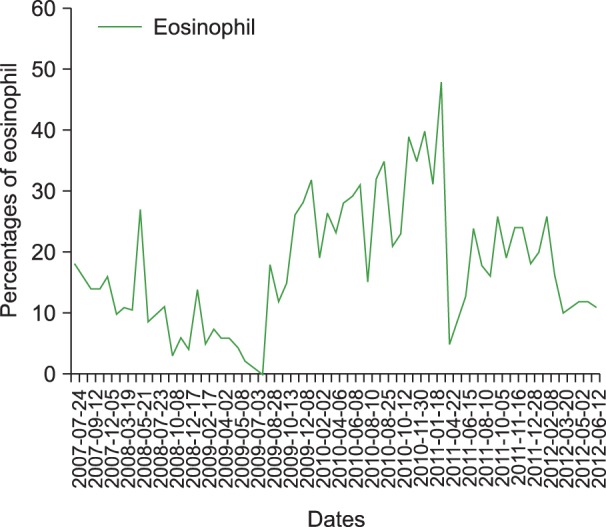
- Myelodysplastic syndrome (MDS) with eosinophilia is a rare condition and has yet to be classified under the 2008 World Health Organization classification. However, reports have described the prognostic significance of chronic persistent eosinophilia in MDS. Here, we report a case of a 67-year-old woman who was admitted to the hospital in July 2007 with generalized weakness, dizziness, and dyspnea on exertion persisting for 5 years. In the initial investigation, eosinophilia (22.1%) in peripheral blood and an increased proportion of eosinophils (5.6%) in normocellular bone marrow with dysplastic megakaryocytes and erythroid cells were noted. Eosinophilia was continuously detected during follow-up over 3 years. In a second bone marrow examination in August 2010, hypercellular bone marrow with similar features was observed. These findings led to the diagnosis of MDS with chronic persistent eosinophilia. To increase awareness of the prognostic significance of MDS with chronic eosinophilia, here we report a slow-progressing case of MDS with chronic persistent eosinophilia lasting over 6 years.
Keyword
MeSH Terms
Figure
Reference
-
1. Yang DW. Myelodysplastic syndrome. In : Park CJ, editor. Laboratory medicine. 4th ed. Seoul, Korea: E-public;2009. p. 185–189.2. Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982; 51:189–199. PMID: 6952920.
Article3. Bennett JM, Komrokji RS. The myelodysplastic syndromes: diagnosis, molecular biology and risk assessment. Hematology. 2005; 10(Suppl 1):258–269. PMID: 16188686.
Article4. Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997; 89:2079–2088. PMID: 9058730.
Article5. Verburgh E, Achten R, Louw VJ, et al. A new disease categorization of low-grade myelodysplastic syndromes based on the expression of cytopenia and dysplasia in one versus more than one lineage improves on the WHO classification. Leukemia. 2007; 21:668–677. PMID: 17301818.
Article6. Sanz GF, Sanz MA, Greenberg PL. Prognostic factors and scoring systems in myelodysplastic syndromes. Haematologica. 1998; 83:358–368. PMID: 9592987.7. Matsushima T, Handa H, Yokohama A, et al. Prevalence and clinical characteristics of myelodysplastic syndrome with bone marrow eosinophilia or basophilia. Blood. 2003; 101:3386–3390. PMID: 12506028.
Article8. Wimazal F, Germing U, Kundi M, et al. Evaluation of the prognostic significance of eosinophilia and basophilia in a larger cohort of patients with myelodysplastic syndromes. Cancer. 2010; 116:2372–2381. PMID: 20209617.
Article9. Wimazal F, Baumgartner C, Sonneck K, et al. Mixed-lineage eosinophil/basophil crisis in MDS: a rare form of progression. Eur J Clin Invest. 2008; 38:447–455. PMID: 18445043.
Article10. Bakotic BW, Poniecka AW, Dominguez CJ, Benigno A, Donahue RP, Cabello-Inchausti B. Myelodysplastic syndrome with atypical eosinophilia in association with ring chromosome 7. A case report. Cancer Genet Cytogenet. 1999; 115:19–22. PMID: 10565294.11. The Korean Society of Hematology. Hematology. 2nd ed. Seoul, Korea: E-public;2011. p. 304–315.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myelodysplastic syndrome that progressed to acute myelomonocytic leukemia with eosinophilia showing peculiar chromosomal abnormality: a case report
- Sweet's Syndrome with Myelodysplastic Syndrome Progressing to Acute Myelogenous Leukemia
- A Case of Idiopathic Hypereosinophihc Syndrome Assoclated with Pulmonary Infiltration
- A Case of Subcutaneous Sweet's Syndrome in MYelodysplastic Syndrome Showing Nuelear Segmentation Anomalies of Neutrophils
- Two different cases of episodic angioedema with eosinophilia