Korean Diabetes J.
2009 Jun;33(3):185-197. 10.4093/kdj.2009.33.3.185.
Effects of Anti-Vascular Endothelial Growth Factor (VEGF) on Pancreatic Islets in Mouse Model of Type 2 Diabetes Mellitus
- Affiliations
-
- 1Division of Endocrinology & Metabolism, Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea. kosh@catholic.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Physiology, The Catholic University of Korea, Seoul, Korea.
- 4Division of Endocrinology & Metabolism, Department of Internal Medicine, Kyung-Hee Uiversity, Seoul, Korea.
- KMID: 2222418
- DOI: http://doi.org/10.4093/kdj.2009.33.3.185
Abstract
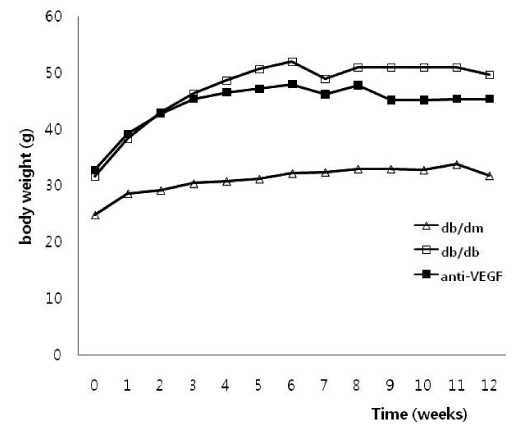
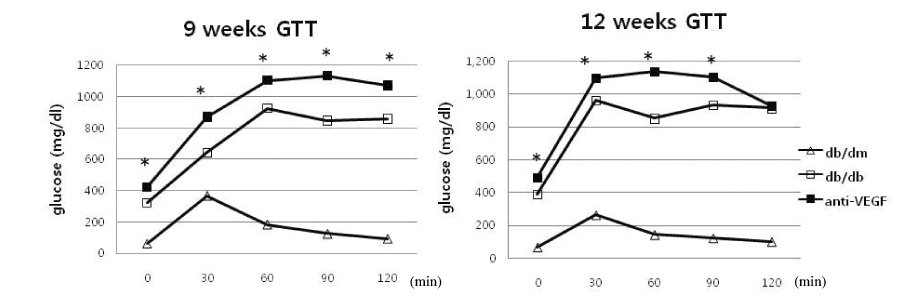
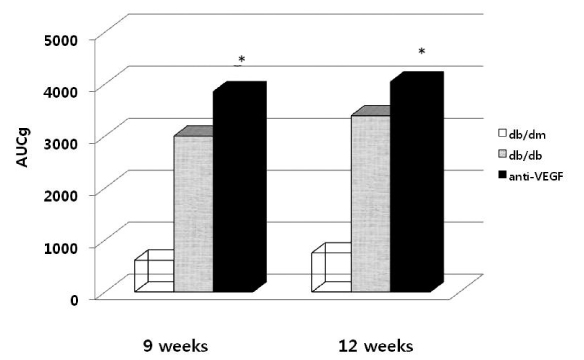
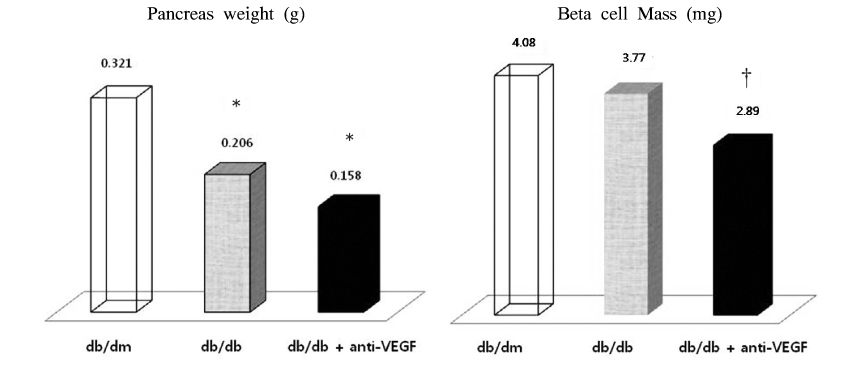
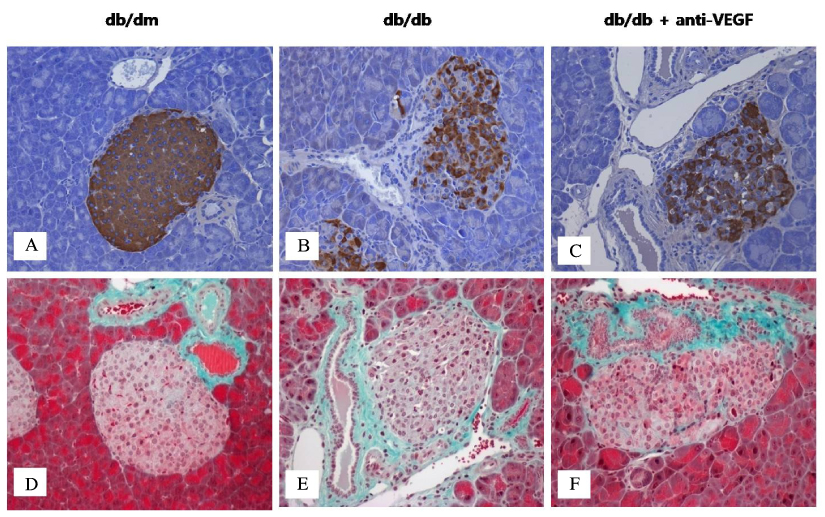
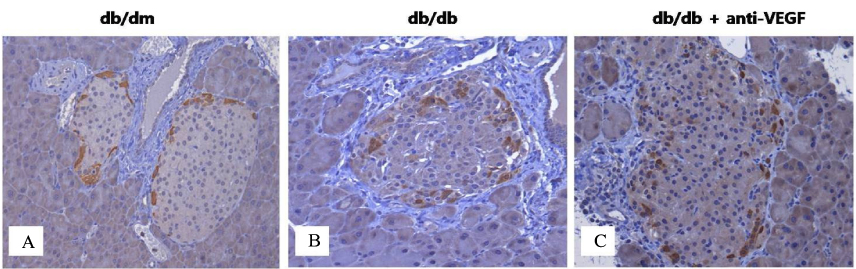
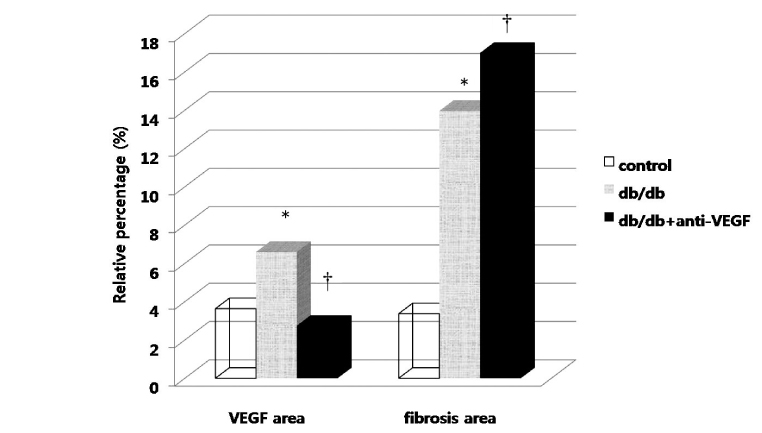
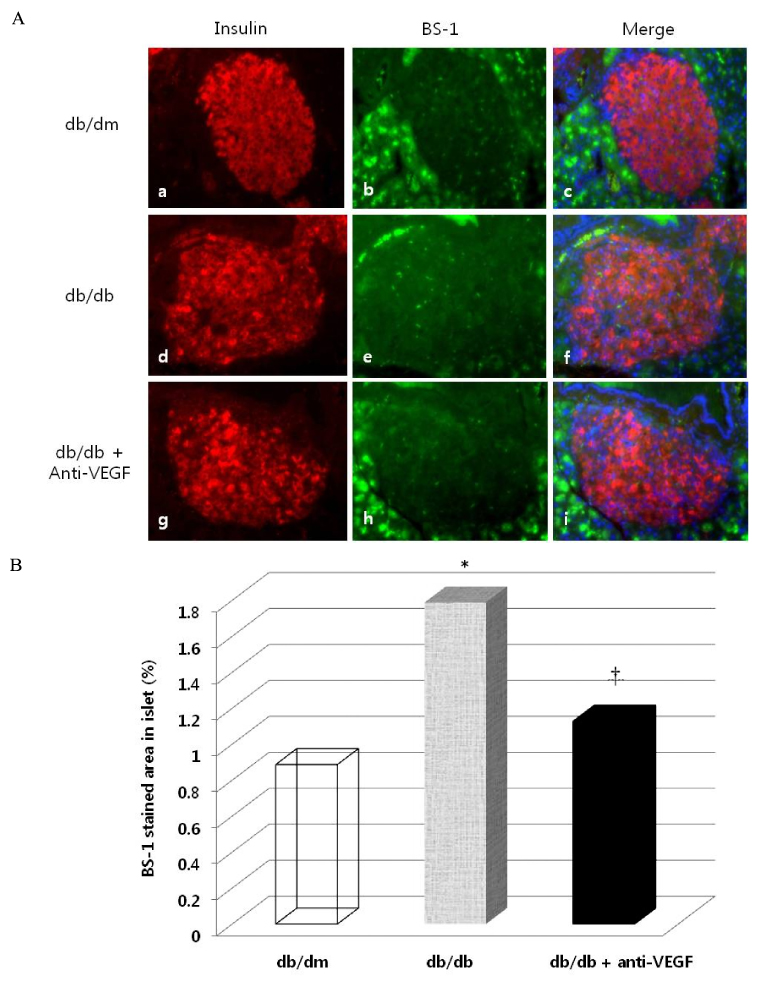
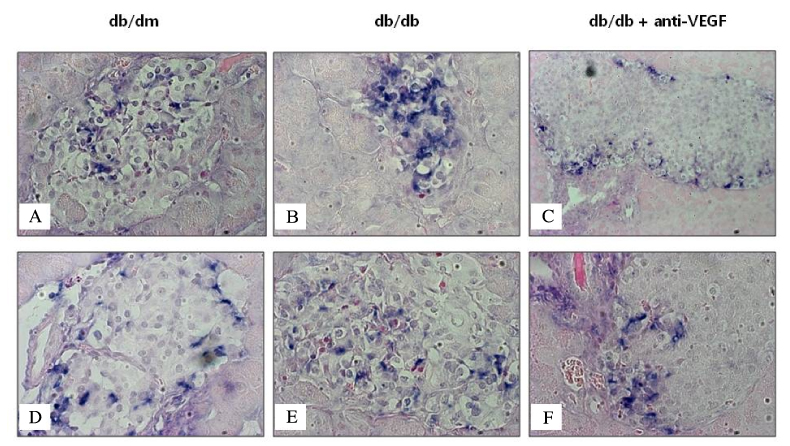
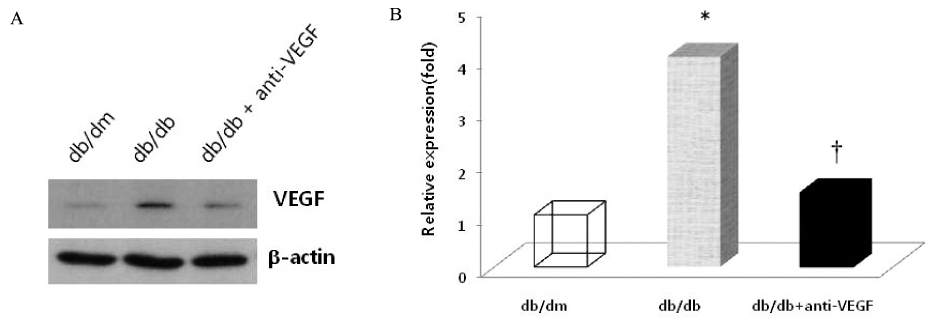
- BACKGROUND
Vascular endothelial growth factor (VEGF) is associated with the development of diabetic complications. However, it is unknown whether systemic VEGF treatment has any effects on the pancreatic islets in an animal model of type 2 diabetes mellitus. METHODS: Anti-VEGF peptide (synthetic ATWLPPR, VEGF receptor type 2 antagonist) was injected into db/db mice for 12 weeks. We analyzed pancreatic islet morphology and quantified beta-cell mass. Endothelial cell proliferation and the severity of islet fibrosis were also measured. VEGF expression in isolated islets was determined using Western blot analysis. RESULTS: When anti-VEGF was administered, db/db mice exhibited more severe hyperglycemia and associated delayed weight gain than non-treated db/db mice. Pancreas weight and pancreatic beta-cell mass were also significantly decreased in the anti-VEGF-treated group. VEGF and VEGF receptor proteins (types 1 and 2) were expressed in the pancreatic islets, and their expression was significantly increased in the db/db group compared with the db/dm group. However, the elevated VEGF expression was significantly reduced by anti-VEGF treatment compared with the db/db group. The anti-VEGF-treated group had more prominent islet fibrosis and islet destruction than db/db mice. Intra-islet endothelial cell proliferation was also remarkably reduced by the anti-VEGF peptide. CONCLUSION: Inhibition of VEGF action by the VEGF receptor 2 antagonist not only suppressed the proliferation of intra-islet endothelial cells but also accelerated pancreatic islet destruction and aggravated hyperglycemia in a type 2 diabetes mouse model. Therefore, the potential effects of anti-VEGF treatment on pancreatic beta cell damage should be considered.
MeSH Terms
-
Animals
Blotting, Western
Diabetes Complications
Diabetes Mellitus, Type 2
Endothelial Cells
Endothelial Growth Factors
Fibrosis
Hyperglycemia
Insulin-Secreting Cells
Islets of Langerhans
Mice
Models, Animal
Pancreas
Proteins
Receptors, Vascular Endothelial Growth Factor
Vascular Endothelial Growth Factor A
Weight Gain
Endothelial Growth Factors
Proteins
Receptors, Vascular Endothelial Growth Factor
Vascular Endothelial Growth Factor A
Figure
Reference
-
1. Flyvbjerg A, Dagnaes-Hansen F, De Vriese AS, Schrijvers BF, Tilton RG, Rasch R. Amelioration of long-term renal changes in obese type 2 diabetic mice by a neutralizing vascular endothelial growth factor antibody. Diabetes. 2002. 51:3090–3094.2. de Vriese AS, Tilton RG, Elger M, Stephan CC, Kriz W, Lameire NH. Antibodies against vascular endothelial growth factor improve early renal dysfunction in experimental diabetes. J Am Soc Nephrol. 2001. 12:993–1000.3. Simorre-Pinatel V, Guerrin M, Chollet P, Penary M, Clamens S, Malecaze F, Plouet J. Vasculotropin-VEGF stimulates retinal capillary endothelial cells through an autocrine pathway. Invest Ophthalmol Vis Sci. 1994. 35:3393–3400.4. Vasir B, Jonas JC, Steil GM, Hollister-Lock J, Hasenkamp W, Sharma A, Bonner-Weir S, Weir GC. Gene expression of VEGF and its receptors Flk-1/KDR and Flt-1 in cultured and transplanted rat islets. Transplantation. 2001. 71:924–935.5. Zhang N, Richter A, Suriawinata J, Harbaran S, Altomonte J, Cong L, Zhang H, Song K, Meseck M, Bromberg J, Dong H. Elevated vascular endothelial growth factor production in islets improves islet graft vascularization. Diabetes. 2004. 53:963–970.6. Stagner J, Mokshagundam S, Wyler K, Samols E, Rilo H, Stagner M, Parthasarathy L, Parthasarathy R. Beta-cell sparing in transplanted islets by vascular endothelial growth factor. Transplant Proc. 2004. 36:1178–1180.7. Byrne AM, Bouchier-Hayes DJ, Harmey JH. Angiogenic and cell survival functions of vascular endothelial growth factor (VEGF). J Cell Mol Med. 2005. 9:777–794.8. Konstantinova I, Lammert E. Microvascular development: learning from pancreatic islets. Bioessays. 2004. 26:1069–1075.9. Kamba T, Tam BY, Hashizume H, Haskell A, Sennino B, Mancuso MR, Norberg SM, O'Brien SM, Davis RB, Gowen LC, Anderson KD, Thurston G, Joho S, Springer ML, Kuo CJ, McDonald DM. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am J Physiol Heart Circ Physiol. 2006. 290:H560–H576.10. Tammela T, Enholm B, Alitalo K, Paavonen K. The biology of vascular endothelial growth factors. Cardiovasc Res. 2005. 65:550–563.11. Lammert E, Gu G, McLaughlin M, Brown D, Brekken R, Murtaugh LC, Gerber HP, Ferrara N, Melton DA. Role of VEGF-A in vascularization of pancreatic islets. Curr Biol. 2000. 13:1070–1074.12. Nikolova G, Jabs N, Konstantinova I, Domogatskaya A, Tryggvason K, Sorokin L, Fässler R, Gu G, Gerber HP, Ferrara N, Melton DA, Lammert E. The vascular basement membrane: a niche for insulin gene expression and Beta cell proliferation. Dev Cell. 2006. 10:397–405.13. Christofori G, Naik P, Hanahan D. Vascular endothelial growth factor and its receptors, flt-1 and flk-1, are expressed in normal pancreatic islets and throughout islet cell tumorigenesis. Mol Endocrinol. 1995. 9:1760–1770.14. Binétruy-Tournaire R, Demangel C, Malavaud B, Vassy R, Rouyre S, Kraemer M, Plouët J, Derbin C, Perret G, Mazié JC. Identification of a peptide blocking vascular endothelial growth Factor (VEGF)-mediated angiogenesis. EMBO J. 2000. 19:1525–1533.15. Zilberberg L, Shinkaruk S, Lequin O, Rousseau B, Hagedorn M, Costa F, Caronzolo D, Balke M, Canron X, Convert O, Laïn G, Gionnet K, Goncalvès M, Bayle M, Bello L, Chassaing G, Deleris G, Bikfalvi A. Structure and inhibitory effects on angiogenesis and tumor development of a new vascular endothelial growth inhibitor. J Biol Chem. 2003. 278:35564–35573.16. Weibel ER. Stereologic methods. Practical Methods for Biologic Morphometry. 1978. Vol. 1. London: Academic Press;101–161.17. Mattsson G. The endothelial cells in islets of langerhans. Ups J Med Sci. 2005. 110:1–15.18. Lacy PE, Kostianovsky M. Method for the isolation of intact islets of Langerhans from the rat pancreas. Diabetes. 1967. 16:35–39.19. Gotoh M, Maki T, Satomi S, Porter J, Bonner-Weir S, O'Hara CJ, Monaco AP. Reproducible high yield of rat islets by stationary in vitro digestion following pancreatic ductal or portal venous collagenase injection. Transplantation. 1987. 43:725–730.20. Iwashita N, Uchida T, Choi JB, Azuma K, Ogihara T, Ferrara N, Gerber H, Kawamori R, Inoue M, Watada H. Impaired insulin secretion in vivo but enhanced insulin secretion from isolated islets in pancreatic beta cell-specific vascular endothelial growth factor-A knock-out mice. Diabetologia. 2007. 50:380–389.21. Xie K, Wei D, Shi Q, Huang S. Constitutive and inducible expression and regulation of vascular endothelial growth factor. Cytokine Growth Factor Rev. 2004. 15:297–324.22. Cross MJ, Dixelius J, Matsumoto T, Claesson-Welsh L. VEGF-receptor signal transduction. Trends Biochem Sci. 2003. 28:488–494.23. Ferrara N, Davis-Smyth T. The biology of vascular endothelial growth factor. Endocr Rev. 1997. 18:4–25.24. Neufeld G, Cohen T, Gengrinovitch S, Poltorak Z. Vascular endothelial growth factor (VEGF) and its receptors. FASEB J. 1999. 13:9–22.25. Li X, Zhang L, Meshinchi S, Dias-Leme C, Raffin D, Johnson JD, Treutelaar MK, Burant CF. Islet microvasculature in islet hyperplasia and failure in a model of type 2 diabetes. Diabetes. 2006. 55:2965–2973.26. Johansson M, Mattsson G, Andersson A, Jansson L, Carlsson PO. Islet endothelial cells and pancreatic beta-cell proliferation: studies in vitro and during pregnancy in adult rats. Endocrinology. 2006. 147:2315–2324.27. Kakizawa H, Itoh M, Itoh Y, Imamura S, Ishiwata Y, Matsumoto T, Yamamoto K, Kato T, Ono Y, Nagata M, Hayakawa N, Suzuki A, Goto Y, Oda N. The relationship between glycemic control and plasma vascular endothelial growth factor and endothelin-1 concentration in diabetic patients. Metabolism. 2004. 53:550–555.28. Linn T, Schneider K, Hammes HP, Preissner KT, Brandhorst H, Morgenstern E, Kiefer F, Bretzel RG. Angiogenic capacity of endothelial cells in islets of Langerhans. FASEB J. 2003. 17:881–883.29. Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G. Upregulation of the vascular endothelial growth factor/vascular endothelial growth factor receptor system in experimental background diabetic retinopathy of the rat. Diabetes. 1998. 47:401–406.30. Lu M, Kuroki M, Amano S, Tolentino M, Keough K, Kim I, Bucala R, Adamis AP. Advanced glycation end products increase retinal vascular endothelial growth factor expression. J Clin Invest. 1998. 1:1219–1224.31. Kuroki M, Voest EE, Amano S, Beerepoot LV, Takashima S, Tolentino M, Kim RY, Rohan RM, Colby KA, Yeo KT, Adamis AP. Reactive oxygen intermediates increase vascular endothelial growth factor expression in vitro and in vivo. J Clin Invest. 1996. 98:1667–1675.32. Ishii H, Jirousek MR, Koya D, Takagi C, Xia P, Clermont A, Bursell SE, Kern TS, Ballas LM, Heath WF, Stramm LE, Feener EP, King GL. Amelioration of vascular dysfunctions in diabetic rats by an oral PKC-b inhibitor. Science. 1996. 272:728–731.33. Pieramici DJ, Rabena MD. Anti-VEGF therapy: comparison of current and future agents. Eye. 2008. 22:1330–1336.34. Nagpal M, Nagpal K, Nagpal PN. A comparative debate on the various anti-vascular endothelial growth factor drugs: pegaptanib sodium (Macugen), ranibizumab (Lucentis) and bevacizumab (Avastin). Indian J Ophthalmol. 2007. 55:437–439.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study for the Improvement of Early Implantation and Long Term Graft Survival in Pancreatic Islet Cell Transplantation by Induction of Angiogenesis with Gene Transfection of Vascuar Endothelial Growth Factor
- Penile Expression of Hypoxia-inducible Factor-1alpha, Vascular Endothelial Growth Factor, and Nitric Oxide Synthase in the Type II Diabetic Rat
- Intravitreal anti-vascular endothelial growth factor treatment for retinal diseases
- Intravitreal injection of anti-vascular endothelial growth factor for patients with various retinal diseases
- Immunohistochemical Study of Transforming Growth Factor-beta2(TGF-beta2) and Vascular Endothelial Growth Factor(VEGF) after Laser Photocoagulation in the Ocular Tissues of White Rats