Infect Chemother.
2013 Dec;45(4):431-434. 10.3947/ic.2013.45.4.431.
High In Vitro Infectivity of a Doxycycline-Insensitive Strain of Orientia tsutsugamushi
- Affiliations
-
- 1Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea. mhchungid@daum.net ljinsoo@inha.ac.kr
- 2Translation Research Center, Inha University School of Medicine, Incheon, Korea.
- 3Department of Microbiology, Inha University School of Medicine, Incheon, Korea.
- KMID: 2170447
- DOI: http://doi.org/10.3947/ic.2013.45.4.431
Abstract
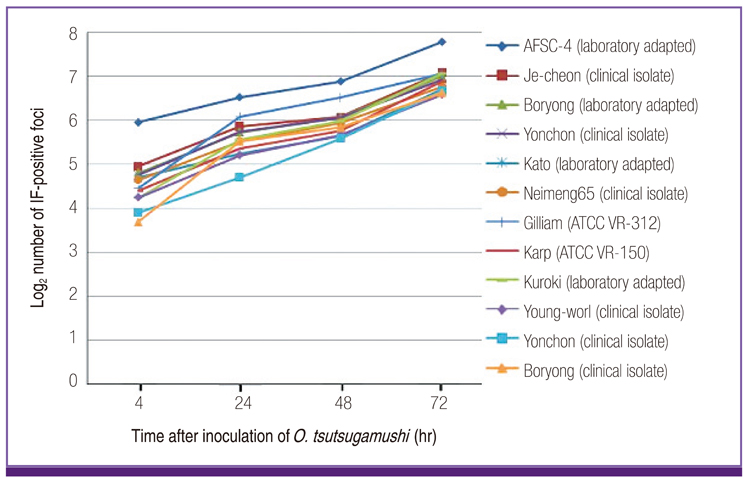
- We compared the infectivity and growth rates of 12 strains of Orientia tsutsugamushi in a cell culture system. ECV304 cells were infected with O. tsutsugamushi strains for 4 hr, and the culture was maintained for 72 hr. Immunofluorescence (IF) staining was performed at 4, 24, 48, and 72 hr after inoculation (hpi), and IF-positive foci were enumerated. The AFSC-4 strain, which is known to be insensitive to doxycycline, showed higher numbers of IF-positive foci than the other 11 strains at 4, 24, 48, and 72 hpi, which may explain its apparent insensitivity to antibiotics.
MeSH Terms
Figure
Cited by 3 articles
-
In vitro Synergism between Chloroquine and Antibiotics against Orientia tsutsugamushi
Dongwook Son, Moon-Hyun Chung
Infect Chemother. 2014;46(3):182-188. doi: 10.3947/ic.2014.46.3.182.In vitro Antagonism between Cefotaxime and Anti-Rickettsial Antibiotics against Orientia tsutsugamushi
Oh Hyun Lee, Ji Hyeon Baek, Jin-Soo Lee, Moon-Hyun Chung, Sun Myoung Lee, Jae-Seung Kang
Infect Chemother. 2014;46(3):189-193. doi: 10.3947/ic.2014.46.3.189.History of Tsutsugamushi Disease in Korea
Moon-Hyun Chung, Jae-Seung Kang
Infect Chemother. 2019;51(2):196-209. doi: 10.3947/ic.2019.51.2.196.
Reference
-
1. Chung MH, Lee JS, Baek JH, Kim M, Kang JS. Persistence of Orientia tsutsugamushi in humans. J Korean Med Sci. 2012; 27:231–235.2. Rajapakse S, Rodrigo C, Fernando SD. Drug treatment of scrub typhus. Trop Doct. 2011; 41:1–4.
Article3. Watt G, Chouriyagune C, Ruangweerayud R, Watcharapichat P, Phulsuksombati D, Jongsakul K, Teja-Isavadharm P, Bhodhidatta D, Corcoran KD, Dasch GA, Strickman D. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet. 1996; 348:86–89.
Article4. Watt G, Kantipong P, Jongsakul K, Watcharapichat P, Phulsuksombati D. Azithromycin activities against Orientia tsutsugamushi strains isolated in cases of scrub typhus in Northern Thailand. Antimicrob Agents Chemother. 1999; 43:2817–2818.
Article5. Strickman D, Sheer T, Salata K, Hershey J, Dasch G, Kelly D, Kuschner R. In vitro effectiveness of azithromycin against doxycycline-resistant and -susceptible strains of Rickettsia tsutsugamushi, etiologic agent of scrub typhus. Antimicrob Agents Chemother. 1995; 39:2406–2410.
Article6. Kelly DJ, Fuerst PA, Ching WM, Richards AL. Scrub typhus: the geographic distribution of phenotypic and genotypic variants of Orientia tsutsugamushi. Clin Infect Dis. 2009; 48:Suppl 3. S203–S230.7. Kim MJ, Kim MK, Kang JS. Improved antibiotic susceptibility test of Orientia tsutsugamushi by flow cytometry using monoclonal antibody. J Korean Med Sci. 2007; 22:1–6.
Article8. Kelly DJ, Salata KF, Strickman D, Hershey JN. Rickettsia tsutsugamushi infection in cell culture: antibiotic susceptibility determined by flow cytometry. Am J Trop Med Hyg. 1995; 53:602–606.
Article9. Groves MG, Kelly DJ. Characterization of factors determining Rickettsia tsutsugamushi pathogenicity for mice. Infect Immun. 1989; 57:1476–1482.
Article10. Kim ES, Kim MK, Lee HM, Kil SH, Chung MH, Lee JS, Kang JS. Doxycycline resistance in Orientia tsutsugamushi isolated from Korean patients. Infect Chemother. 2008; 40:259–265.
Article11. Jeong HW, Choi YK, Baek YH, Seong MH. Phylogenetic analysis of the 56-kDa type-specific protein genes of Orientia tsutsugamushi in central Korea. J Korean Med Sci. 2012; 27:1315–1319.
Article12. Watt G, Kantipong P, Jongsakul K, Watcharapichat P, Phulsuksombati D, Strickman D. Doxycycline and rifampicin for mild scrub-typhus infections in northern Thailand: a randomised trial. Lancet. 2000; 356:1057–1061.
Article13. Kim YS. Controlled trial of doxycycline versus rifampin for treatment of mild to moderate scrub typhus. Gwangju: Chosun University;2010. Master's Thesis.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In vitro Synergism between Chloroquine and Antibiotics against Orientia tsutsugamushi
- In vitro Antagonism between Cefotaxime and Anti-Rickettsial Antibiotics against Orientia tsutsugamushi
- In vitro Study on the Dose and Duration of Doxycycline Treatment against Orientia tsutsugamushi
- Improved Antibiotic Susceptibility Test of Orientia tsutsugamushi by Flow Cytometry Using Monoclonal Antibody
- A Case of Tsutsugamushi Disease