Tuberc Respir Dis.
2007 Feb;62(2):140-143. 10.4046/trd.2007.62.2.140.
Successful Treatment with High Dose Transdermal Fentanyl Patch for Severe Cancer Pain in a Patient with Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Inha University, Incheon, Korea. jsryu@inha.ac.kr
- KMID: 2114602
- DOI: http://doi.org/10.4046/trd.2007.62.2.140
Abstract
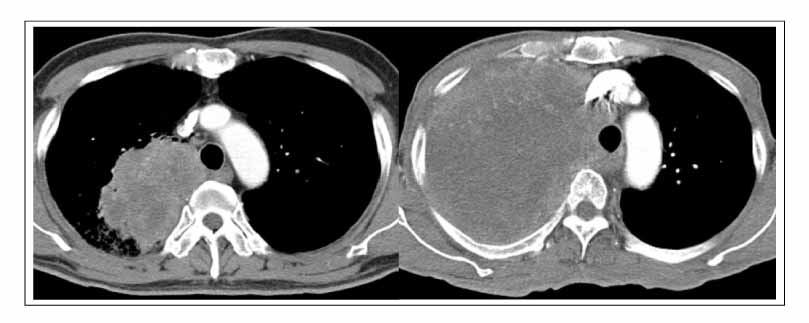
- A 60-year-old man was diagnosed with locally advanced non-small cell lung cancer. He refused treatment with a curative aim and was treated conservatively. Pain had developed on his shoulder and chest wall, which became worse as the cancer progressed. Although his pain initially appeared to be relieved with weak opioids and analgesics, it became more severe Strong opioids (transdermal fentanly patch and oxycodone), antidepressant or epidural block were introduced, However, the background pain became more intense and reached up to 8~9/10 on the visual analog scale (VAS). The dose of the transdermal fentanl patch was gradually increased to 600?g/hr, which resulted in a dramatic improvement in his pain (9/10 of VAS) to 3/10 for most of the time. We described the successful experience with a high dose transdermal fentanyl patch for cancer pain relief, which might be an alternative option for cancer patients suffering from severe pain.
Keyword
MeSH Terms
Figure
Reference
-
1. The World Health Report 1996: fighting disease, fostering development, executive summary. World Health Organization. 1996. Geneva: World Health Organization;Avail from: URL:http://www.who.int/whr/1996/en/.2. Cherny N. New strategies in opioid therapy for cancer pain. J Oncol Manag. 2000. 9:8–15.3. Muijsers RB, Wagstaff AJ. Transdermal fentanyl: an updated review of its pharmacological properties and therapeutic efficacy in chronic cancer pain control. Drugs. 2001. 61:2289–2307.4. Allan L, Hays H, Jensen NH, de Waroux BL, Bolt M, Donald R, et al. Randomised crossover trial of transdermal fentanyl and sustained release oral morphine for treating chronic non-cancer pain. BMJ. 2001. 322:1154–1158.5. Skaer TL. Management of pain in the cancer patient. Clin Ther. 1993. 15:638–649.6. Ahles TA, Ruckdeschel JC, Blanchard EB. Cancer-related pain-II: assessment with visual analogue scales. J Psychosom Res. 1984. 28:121–124.7. Grond S, Zech D, Diefenbach C, Radbruch L, Lehmann KA. Assessment of cancer pain: a prospective evaluation in 2266 cancer patients referred to a pain service. Pain. 1996. 64:107–114.8. Brescia FJ, Adler D, Gray G, Ryan MA, Cimino J, Mamtani R. Hospitalized advanced cancer patients: a profile. J Pain Symptom Manage. 1990. 5:221–227.9. Korean Society for Hospice and Palliative Care, Korean Cancer Study Group. Cancer pain relief guideline. 2001. Seoul: Korean society for hospice and palliative care, Korean cancer study group.10. NCCN clinical pratice guideline: adult cancer pain. National Comprehensive Cancer Network. 2006. Avail from: URL:http://www.nccn.org/professionals/physician_gls/PDF/pain.pdf.11. Potter J, Higginson IJ. Pain experienced by lung cancer patients: a review of prevalence, causes and pathophysiology. Lung Cancer. 2004. 43:247–257.12. Radbruch L, Sabatowski R, Petzke F, Brunsch-Radbruch A, Grond S, Lehmann KA. Transdermal fentanyl for the management of cancer pain: a survey of 1005 patients. Palliat Med. 2001. 15:309–321.13. Menahem S, Shvartzman P. High-dose fentanyl patch for cancer pain. J Am Board Fam Pract. 2004. 17:388–390.14. Portenoy RK, Lesage P. Management of cancer pain. Lancet. 1999. 353:1695–1700.15. Ripamonti C, Zecca E, De Conno F. Pharmacological treatment of cancer pain: alternative routes of opioid administration. Tumori. 1998. 84:289–300.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Transdermal Fentanyl Patch in Cancer Pain Patients
- A Case of Successful Management of Lung Cancer Pain Using Ultrahigh-dose Fentanyl Patch
- High-Dose Fentanyl Patch for Cancer Pain of a Patient with Cholangiocarcinoma
- A Case of Fentanyl Toxicity with Misused Durogesic Transdermal Patch
- Comparison of an Additional Transdermal Fentanyl Patch Compared to Intravenous NSAID and Opioid Analgesics within 24 Hours of an Uterine Artery Embolization for Myoma and Adenomyosis