Tuberc Respir Dis.
2010 May;68(5):286-289.
A Case of Successful Management of Lung Cancer Pain Using Ultrahigh-dose Fentanyl Patch
- Affiliations
-
- 1Department of Internal Medicine, Seonam University Medical School, Gwangju, Korea.
- 2Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. droij@chonnam.ac.kr
- 3Lung and Esophageal Cancer Clinic, Chonnam National University Hwasun Hospital, Hwasun, Korea.
Abstract
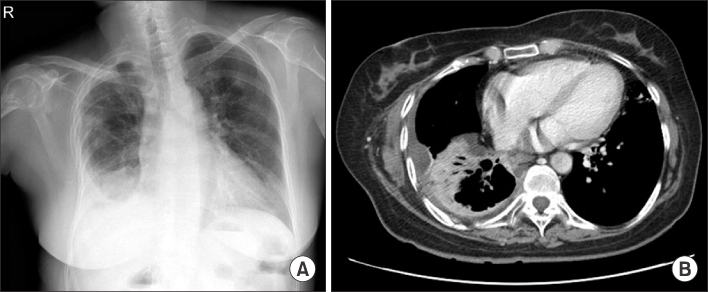
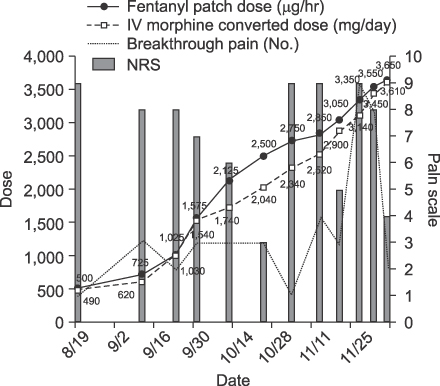
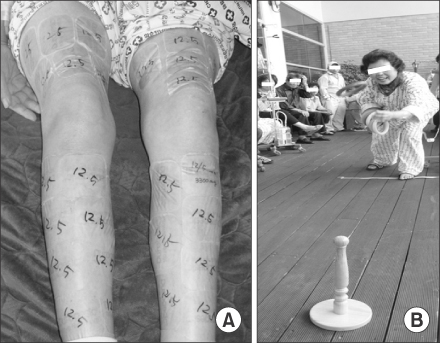
- A 55-year old woman with advanced stage non-small cell lung cancer was admitted to hospital for the management of severe chest pain, which measured 7 out of 10 on a numerical rating scale (NRS). Despite palliative radiation and the application of multiple epidural blocks, she continued to experience severe cancer pain. We gradually increased the dose of transdermal fentanyl patches from 500 microgram/hr to 3,650 microgram/hr, for 3 months without any significant side effects. Concomitantly, adjuvant therapy with antidepressants and anticonvulsants were added, decreasing the patient's pain to NRS 3~4 down from 7. After being transferred to a hospice clinic, her chest pain was well-controlled below NRS 4 by means of strong opioid medications, including the highest dose of transdermal fentanyl 4,050 microgram/hr for more than 16 months.
Keyword
MeSH Terms
Figure
Reference
-
1. NCCN clinical practice guidelines in oncology: adult cancer pain V.1.2009 [Internet]. National Comprehensive Cancer Network. 2009. cited 2010 Feb 16. Fort Washington: National Comprehensive Cancer Network;Available from: http://www.nccn.org/professionals/physician_gls/PDF/pain.pdf.2. Potter J, Higginson IJ. Pain experienced by lung cancer patients: a review of prevalence, causes and pathophysiology. Lung Cancer. 2004. 43:247–257.3. Stjernswärd J, Colleau SM, Ventafridda V. The World Health Organization Cancer Pain and Palliative Care Program: past, present, and future. J Pain Symptom Manage. 1996. 12:65–72.4. Kress HG, Von der Laage D, Hoerauf KH, Nolte T, Heiskanen T, Petersen R, et al. A randomized, open, parallel group, multicenter trial to investigate analgesic efficacy and safety of a new transdermal fentanyl patch compared to standard opioid treatment in cancer pain. J Pain Symptom Manage. 2008. 36:268–279.5. Menahem S, Shvartzman P. High-dose fentanyl patch for cancer pain. J Am Board Fam Pract. 2004. 17:388–390.6. Radbruch L, Elsner F. Clinical experience with transdermal fentanyl for the treatment of cancer pain in Germany. Keio J Med. 2004. 53:23–29.7. Seamans DP, Wong GY, Wilson JL. Interventional pain therapy for intractable abdominal cancer pain. J Clin Oncol. 2000. 18:1598–1600.8. Ryu JS, Kim SH, Um UH, Cho JH, Kwak SM, Lee HL. Successful treatment with high dose transdermal fentanyl patch for severe cancer pain in a patient with lung cancer. Tuberc Respir Dis. 2007. 62:140–143.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treatment with High Dose Transdermal Fentanyl Patch for Severe Cancer Pain in a Patient with Lung Cancer
- The Effectiveness of Transdermal Fentanyl Patch in Cancer Pain Patients
- Clinical Usefulness of Fentanyl Matrix Patch for the Patients with Chronic Low Back Pain
- High-Dose Fentanyl Patch for Cancer Pain of a Patient with Cholangiocarcinoma
- Two Cases of Fentanyl Intoxication Through Overusing Fentanyl Patch