Electrolyte Blood Press.
2014 Dec;12(2):74-79. 10.5049/EBP.2014.12.2.74.
Epidermal Proteinase-Activated Receptor-2 Expression is Increased in End-Stage Renal Disease Patients with Pruritus: A Pilot Study
- Affiliations
-
- 1Department of Internal Medicine, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 2Department of Dermatology/Atopy and Asthma Center & Seoul Medical Research Institute, Seoul Medical Center, Seoul, Korea.
- 3Department of Dermatology and Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. hask1951@yuhs.ac
- KMID: 2052334
- DOI: http://doi.org/10.5049/EBP.2014.12.2.74
Abstract
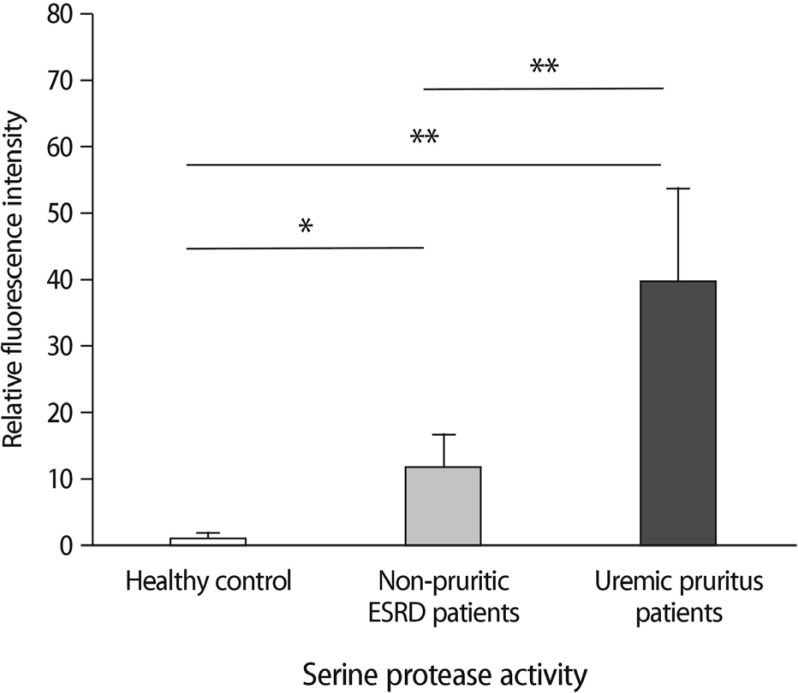
- Uremic pruritus is a common problem in patients with end-stage renal disease (ESRD), but the underlying mechanisms are not yet fully understood. We aimed to investigate the association between severity of uremic pruritus and cutaneous serine protease activity, as well as proteinase-activated receptor-2 (PAR-2) expression. Twelve ESRD patients with pruritus, 4 ESRD patients without pruritus, and 6 healthy controls were enrolled. Skin biopsies were obtained from the abdomen. Protease activity and PAR-2 expression in the epidermis were examined by in situ zymography and confocal laser microscopy, respectively. All ESRD patients presented more pronounced cutaneous protease activity compared with that in healthy controls. The skin samples from the patients with pruritus showed higher protease activity than either nonpruritic ESRD patients or healthy controls. The epidermis in all samples of ESRD patients presented higher immunoreactivity against PAR-2 versus those of healthy controls. In addition, correlation analysis between PAR-2 expression and VAS pruritus scores showed a significant positive correlation. Our data suggests that levels of serine protease and PAR-2 expression could play important roles in the pathogenesis of uremic pruritus.
MeSH Terms
Figure
Reference
-
1. Mistik S, Utas S, Ferahbas A, Tokgoz B, Unsal G, Sahan H, et al. An epidemiology study of patients with uremic pruritus. J Eur Acad Dermatol Venereol. 2006; 20:672–678. PMID: 16836494.
Article2. Pisoni RL, Wikström B, Elder SJ, Akizawa T, Asano Y, Keen ML, et al. Pruritus in haemodialysis patients: International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2006; 21:3495–3505. PMID: 16968725.
Article3. Szepietowski JC, Schwartz RA. Uremic pruritus. Int J Dermatol. 1998; 37:247–353. PMID: 9585892.4. Chen YC, Chiu WT, Wu MS. Therapeutic effect of topical gamma-linolenic acid on refractory uremic pruritus. Am J Kidney Dis. 2006; 48:69–76. PMID: 16797388.
Article5. Patel TS, Freedman BI, Yosipovitch G. An update on pruritus associated with CKD. Am J Kidney Dis. 2007; 50:11–20. PMID: 17591521.
Article6. Steinhoff M, Neisius U, Ikoma A, Fartasch M, Heyer G, Skov PS, et al. Proteinase-activated receptor-2 mediates itch: a novel pathway for pruritus in human skin. J Neurosci. 2003; 23:6176–6180. PMID: 12867500.
Article7. Vergnolle N, Bunnett NW, Sharkey KA, Brussee V, Compton SJ, Grady EF, et al. Proteinase-activated receptor-2 and hyperalgesia: A novel pain pathway. Nat Med. 2001; 7:821–826. PMID: 11433347.
Article8. Akiyama T, Merrill AW, Carstens MI, Carstens E. Activation of superficial dorsal horn neurons in the mouse by a PAR-2 agonist and 5-HT: potential role in itch. J Neurosci. 2009; 29:6691–6699. PMID: 19458238.
Article9. Jeong SK, Kim HJ, Youm JK, Ahn SK, Choi EH, Sohn MH, et al. Mite and cockroach allergens activate protease-activated receptor 2 and delay epidermal permeability barrier recovery. J Invest Dermatol. 2008; 128:1930–1939. PMID: 18305573.
Article10. Déry O, Corvera CU, Steinhoff M, Bunnett NW. Proteinase-activated receptors: novel mechanisms of signaling by serine proteases. Am J Physiol. 1998; 274:C1429–C1452. PMID: 9696685.
Article11. Nystedt S, Ramakrishnan V, Sundelin J. The proteinaseactivated receptor 2 is induced by inflammatory mediators in human endothelial cells. Comparison with the thrombin receptor. J Biol Chem. 1996; 271:14910–14915. PMID: 8663011.12. Rattenholl A, Steinhoff M. Proteinase-activated receptor-2 in the skin: receptor expression, activation and function during health and disease. Drug News Perspect. 2008; 21:369–381. PMID: 19259550.
Article13. Manenti L, Vaglio A, Borgatti PP. Gabapentin as a therapeutic option in uremic pruritus. Kidney Int. 2008; 73:512. PMID: 18235531.
Article14. Wikström B, Gellert R, Ladefoged SD, Danda Y, Akai M, Ide K, et al. Kappa-opioid system in uremic pruritus: multicenter, randomized, double-blind, placebo-controlled clinical studies. J Am Soc Nephrol. 2005; 16:3742–3747. PMID: 16251241.15. Montalto G, Lorello D, Carroccio A, Sparacino V, Li Vecchi M, Soresi M, et al. Serum trypsin in chronic renal failure and transplant patients. Am J Gastroenterol. 1992; 87:1175–1179. PMID: 1381554.16. Hashemi M, Mehrabifar H, Homayooni F, Naderi M, Montazerifar F, Ghavami S. Serum trypsin inhibitory capacity in hemodialysis patients. Saudi J Kidney Dis Transpl. 2009; 20:604–607. PMID: 19587500.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidermal Growth Factor Receptor Expression and Cell Proliferation in Renal Cell Carcinoma
- Effectiveness of Topical Chia Seed Oil on Pruritus of End-stage Renal Disease (ESRD) Patients and Healthy Volunteers
- A Studyof Dermal Mast Cells Number in End Stage of Renal Failure
- Correlation of epidermal growth factor receptor expression with prognostic factors in patients with ovarian neoplasms
- Hemangioma Mistaken for Renal Cell Carcinoma in a Patient With End-Stage Renal Disease: A Case Report