Infect Chemother.
2012 Dec;44(6):526-529. 10.3947/ic.2012.44.6.526.
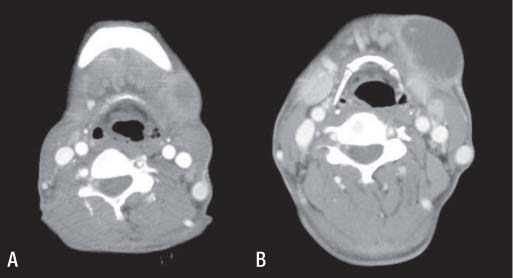
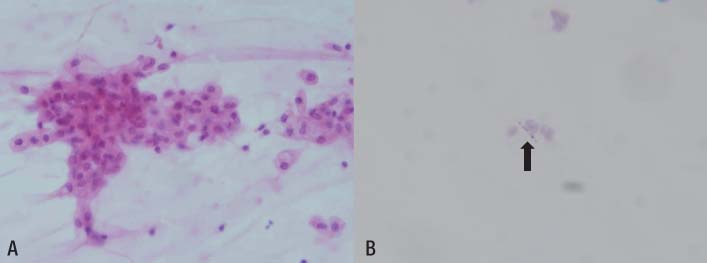
A Case of Mycobacterium kansasii Lymphadenitis in HIV-infected Patient
- Affiliations
-
- 1Department of Internal Medicine, National Medical Center, Seoul, Korea. moberrer@hanmail.net
- KMID: 1806948
- DOI: http://doi.org/10.3947/ic.2012.44.6.526
Abstract
- Nontuberculous mycobacteria (NTM) are widely present in the environment, although they rarely cause infection in humans. However, infection by NTM has been increasingly recognized worldwide in the context of the human immunodeficiency virus (HIV) epidemic and therapeutic immunosuppression. Mycobacterium kansasii is a slow-growing photochromogenic mycobacterium, which mainly causes pulmonary infection in patients with predisposing lung diseases, and, occasionally, disseminated infection with poor outcomes in immunocompromised patients. We report on the first case of lymphadenitis caused by infection with M.kansasii in an HIV-infected patient in Korea. The patient showed significant improvement after receiving antituberculous therapy (isoniazid, rifabutin) in combination with surgical drainage and highly active antiretroviral therapy (abacavir, lamivudine, and lopinavir/ritonavir).
MeSH Terms
Figure
Cited by 1 articles
-
Mycobacterium kansasii Pneumonia with Mediastinal Lymphadenitis in a Patient with Acute Myeloid Leukemia: Successful Treatment to Stem Cell Transplantation
Yeon-Geun Choi, Sung-Yeon Cho, Dong-Gun Lee, Eunjung Yim, Hyonsoo Joo, Seongyul Ryu, Jae-Ki Choi, Hee-Je Kim
Infect Chemother. 2017;49(1):78-83. doi: 10.3947/ic.2017.49.1.78.
Reference
-
1. Koh WJ, Kwon OJ. Treatment of nontuberculous mycobacterial pulmonary diseases. Tuberc Respir Dis. 2004. 56:5–17.
Article2. Koh WJ, Kwon OJ. Diagnosis and treatment of nontuberculous mycobacterial lung disease. Korean J Med. 2008. 74:120–131.
Article3. Kim JH, Suh JT, Park SY, Lee HJ, Lee WI. Clinical evaluation of 10 cases of nontuberculous mycobacteria isolated from sputum. Korean J Lab Med. 2004. 24:49–52.4. Park HJ, Yu H, Choi SH, Sung H, Hong JP, Kim JJ, Lee SO. A case of Mycobacterium kansasii cutaneous infection in a heart transplant recipient. Korean J Med. 2011. 81:121–125.5. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ Jr, Winthrop K. ATS Mycobacterial Diseases Subcommittee. American Thoracic Society. Infectious Disease Society of America. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
Article6. Reddy VC, Prasad CE, Aparna S, Gokhale S, Anjeneyulu . A study of mycobacterial species causing lymphadenitis. Southeast Asian J Trop Med Public Health. 2008. 39:130–135.7. Santin M, Alcaide F. Mycobacterium kansasii disease among patients infected with human immunodeficiency virus type 1: improved prognosis in the era of highly active antiretroviral therapy. Int J Tuberc Lung Dis. 2003. 7:673–677.8. Stellbrink HJ, Koperski K, Albrecht H, Greten H. Mycobacterium kansasii infection limited to skin and lymph node in a patient with AIDS. Clin Exp Dermatol. 1990. 15:457–458.
Article9. Kotb R, Dhote R, Garcia-Ricart F, Permal S, Carlotti A, Arfi C, Christoforov B. Cutaneous and Mediastinal Lymphadenitis due to Mycobacterium kansasii. J Infect. 2001. 42:277–278.10. Saritsiri S, Udomsantisook N, Suankratay C. Nontuberculous mycobacterial infections in King Chulalongkorn Memorial Hospital. J Med Assoc Thai. 2006. 89:2035–2046.11. The Korean Academy of Tuberculosis and Respiratory Diseases. Treatment guidelines for tuberculosis. 2005. 4th ed. 142–143.12. Hung SC, Chang SC. New pulmonary lesions during therapy for extrapulmonary tuberculosis. Chest. 1999. 116:1794–1797.
Article13. Song JY, Cheong HJ. Diagnosis and treatment of cervical lymphadenitis from a standpoint of infectious disease specialists. Infect Chemother. 2008. 40:76–82.
Article14. DeSimone JA, Pomerantz RJ, Babinchak TJ. Inflammatory reactions in HIV-1-infected persons after initiation of highly active antiretroviral therapy. Ann Intern Med. 2000. 133:447–454.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium kansasii Pulmonary Disease Presenting as Endobronchial Lesions in HIV-Infected Patient
- Mycobacterium kansasii Pneumonia with Mediastinal Lymphadenitis in a Patient with Acute Myeloid Leukemia: Successful Treatment to Stem Cell Transplantation
- Mycobacterium Kansasii Disease Presenting As a Lung Mass and Bronchial Anthracofibrosis
- Necrotizing Cervical Lymphadenitis Caused by Mycobacterium simiae in an HIV-Positive Patient: Imaging with 18F-FDG PET/CT
- A Case of Pulmonary Mycobacterium kansasii Disease Complicated with Tension Pneumothorax