Tuberc Respir Dis.
2015 Oct;78(4):356-359. 10.4046/trd.2015.78.4.356.
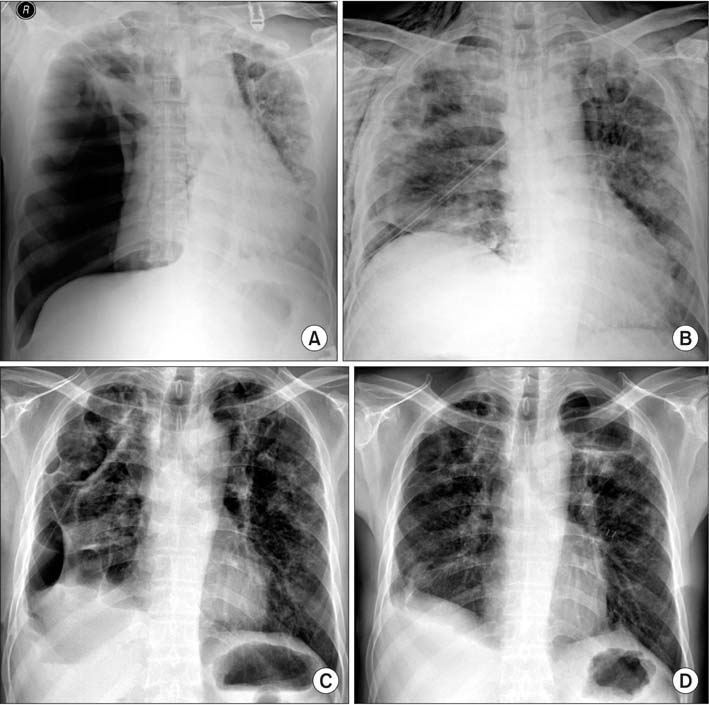
A Case of Pulmonary Mycobacterium kansasii Disease Complicated with Tension Pneumothorax
- Affiliations
-
- 1Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea. lovlet@paran.com
- KMID: 2320705
- DOI: http://doi.org/10.4046/trd.2015.78.4.356
Abstract
- Pneumothorax is an extremely rare complication of non-tuberculous mycobacterial infection. A 52-year-old man presenting with difficulty breathing and chest pain was admitted to our hospital. A right-sided pneumothorax was observed on chest radiography and chest computed tomography showed multiple cavitating and non-cavitating nodules with consolidation in the upper to middle lung zones bilaterally. Serial sputum cultures were positive for Mycobacterium kansasii, and he was diagnosed with pulmonary M. kansasii disease complicated by tension pneumothorax. After initiation of treatment including decortications and pleurodesis, the patient made a full recovery. We herein describe this patient's course in detail and review the current relevant literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Lai CC, Tan CK, Chou CH, Hsu HL, Liao CH, Huang YT, et al. Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000-2008. Emerg Infect Dis. 2010; 16:294–296.2. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.3. Park HK, Koh WJ, Shim TS, Kwon OJ. Clinical characteristics and treatment outcomes of Mycobacterium kansasii lung disease in Korea. Yonsei Med J. 2010; 51:552–556.4. Griffith DE, Brown-Elliott BA, Wallace RJ Jr. Thrice-weekly clarithromycin-containing regimen for treatment of Mycobacterium kansasii lung disease: results of a preliminary study. Clin Infect Dis. 2003; 37:1178–1182.5. Kobashi Y, Mouri K, Obase Y, Kato S, Oka M. Clinical analysis of patients with pulmonary nontuberculous mycobacterial disease complicated by pneumothorax. Intern Med. 2013; 52:2511–2515.6. Hagiwara E, Komatsu S, Nishihira R, Shinohara T, Baba T, Ogura T. Clinical characteristics and prevalence of pneumothorax in patients with pulmonary Mycobacterium avium complex disease. J Infect Chemother. 2013; 19:588–592.7. Shitrit D, Peled N, Bishara J, Priess R, Pitlik S, Samra Z, et al. Clinical and radiological features of Mycobacterium kansasii infection and Mycobacterium simiae infection. Respir Med. 2008; 102:1598–1603.8. Matveychuk A, Fuks L, Priess R, Hahim I, Shitrit D. Clinical and radiological features of Mycobacterium kansasii and other NTM infections. Respir Med. 2012; 106:1472–1477.9. Kobashi Y, Fukuda M, Yoshida K, Miyashita N, Oka M. Pulmonary Mycobacterium intracellulare disease with a solitary pulmonary nodule detected at the onset of pneumothorax. J Infect Chemother. 2006; 12:203–206.10. Asai K, Urabe N. Acute empyema with intractable pneumothorax associated with ruptured lung abscess caused by Mycobacterium avium. Gen Thorac Cardiovasc Surg. 2011; 59:443–446.11. Freixinet JL, Caminero JA, Marchena J, Rodriguez PM, Casimiro JA, Hussein M. Spontaneous pneumothorax and tuberculosis: long-term follow-up. Eur Respir J. 2011; 38:126–131.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium kansasii Pulmonary Disease Presenting as Endobronchial Lesions in HIV-Infected Patient
- A Case Report of Three Patients with Nontuberculous Mycobacterial Pulmonary Disease Caused by Mycobacterium kansasii
- Mycobacterium kansasii Pulmonary Diseases in Korea
- Mycobacterium Kansasii Disease Presenting As a Lung Mass and Bronchial Anthracofibrosis
- A case of Idiopathic CD4+ T-Lymphocytopenia with disseminated Mycobacterium kansasii infection and Pulmonary alveolar proteinosis