Tuberc Respir Dis.
2013 Oct;75(4):157-160.
A Case of Mycobacterium kansasii Pulmonary Disease Presenting as Endobronchial Lesions in HIV-Infected Patient
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. rkdwldud@catholic.ac.kr
Abstract
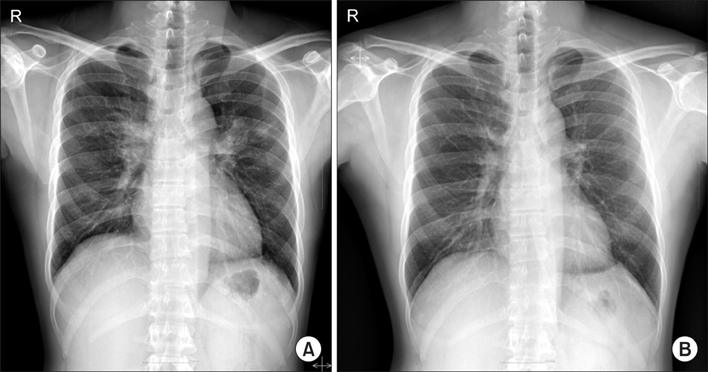
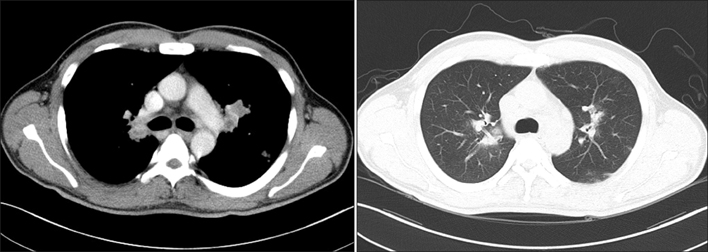
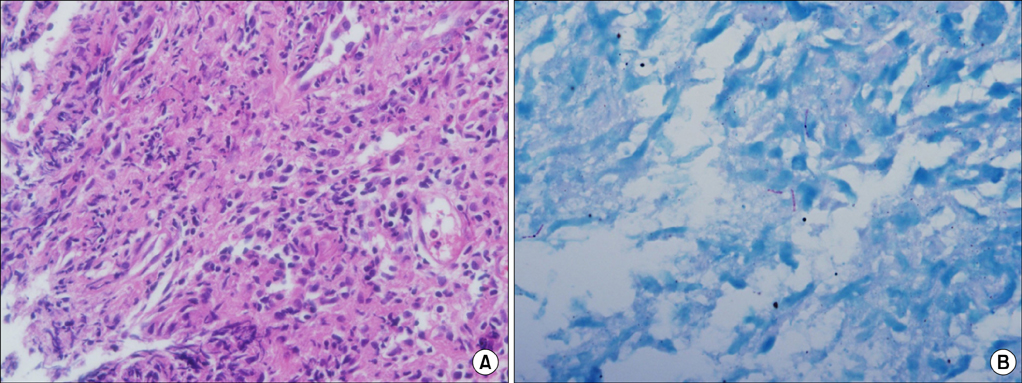
- Incidence of nontuberculous mycobacterium (NTM) pulmonary disease is increasing with the wider recognition and development of diagnostic technology. Mycobacterium kansasii is the second most common pathogen of NTM pulmonary disease in human immunodeficiency virus (HIV)-infected patients. However in Korea, the incidence of M. kansasii pulmonary disease is relatively low, and there has been no report of M. kansasii pulmonary disease with bronchial involvement in HIV patients, to the best of our knowledge. We report a case of M. kansasii pulmonary disease presenting with endobronchial lesions in an HIV-infected patient complaining of chronic cough with bilateral enlargements of hilar lymph nodes on chest X-ray.
Keyword
MeSH Terms
Figure
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.2. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006; 129:341–348.3. Griffith DE. Management of disease due to Mycobacterium kansasii. Clin Chest Med. 2002; 23:613–621.4. Park SY, Park JH, Jegal YJ, Lee JH, Lim CM, Lee SD, et al. A case of idiopathic CD4+ T-lymphocytopenia with disseminated Mycobacterium kansasii infection and pulmonary alveolar proteinosis. Tuberc Respir Dis. 2000; 48:377–382.5. Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, Lee NY, et al. A case report of three patients with nontuberculous mycobacterial pulmonary disease caused by Mycobacterium kansasii. Tuberc Respir Dis. 2003; 54:459–466.6. Maliwan N, Zvetina JR. Clinical features and follow up of 302 patients with Mycobacterium kansasii pulmonary infection: a 50 year experience. Postgrad Med J. 2005; 81:530–533.7. Connolly MG Jr, Baughman RP, Dohn MN. Mycobacterium kansasii presenting as an endobronchial lesion. Am Rev Respir Dis. 1993; 148:1405–1407.8. Manali ED, Tomford WJ, Liao DW, Farver C, Mehta AC. Mycobacterium kansasii endobronchial ulcer in a nonimmunocompromised patient. Respiration. 2005; 72:305–308.9. An JY, Lee JE, Park HW, Lee JH, Yang SA, Jung SS, et al. Clinical and bronchoscopic features in endobronchial tuberculosis. Tuberc Respir Dis. 2006; 60:532–539.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium kansasii Lymphadenitis in HIV-infected Patient
- Mycobacterium Kansasii Disease Presenting As a Lung Mass and Bronchial Anthracofibrosis
- A Case of Pulmonary Mycobacterium kansasii Disease Complicated with Tension Pneumothorax
- A Case of Pulmonary and Endobronchial Mycobacterium avium Infection Presenting as an Acute Pneumonia in an Immunocompetent Patient
- A case of Idiopathic CD4+ T-Lymphocytopenia with disseminated Mycobacterium kansasii infection and Pulmonary alveolar proteinosis