Korean J Pain.
2024 Jul;37(3):233-246. 10.3344/kjp.24042.
Ferroptosis inhibitor ferrostatin-1 attenuates morphine tolerance development in male rats by inhibiting dorsal root ganglion neuronal ferroptosis
- Affiliations
-
- 1Ankara City Hospital, Anesthesia and Intensive Care, Ankara, Turkey
- 2Departments of Physiology, School of Medicine, Cumhuriyet University, Sivas, Turkey
- 3Departments of Pharmacology, School of Medicine, Cumhuriyet University, Sivas, Turkey
- KMID: 2557727
- DOI: http://doi.org/10.3344/kjp.24042
Abstract
- Background
Ferrostatin-1 and liproxstatin-1, both ferroptosis inhibitors, protect cells. Liproxstatin-1 decreases morphine tolerance. Yet, ferrostatin-1's effect on morphine tolerance remains unexplored. This study aimed to evaluate the influence of ferrostatin-1 on the advancement of morphine tolerance and understand the underlying mechanisms in male rats.
Methods
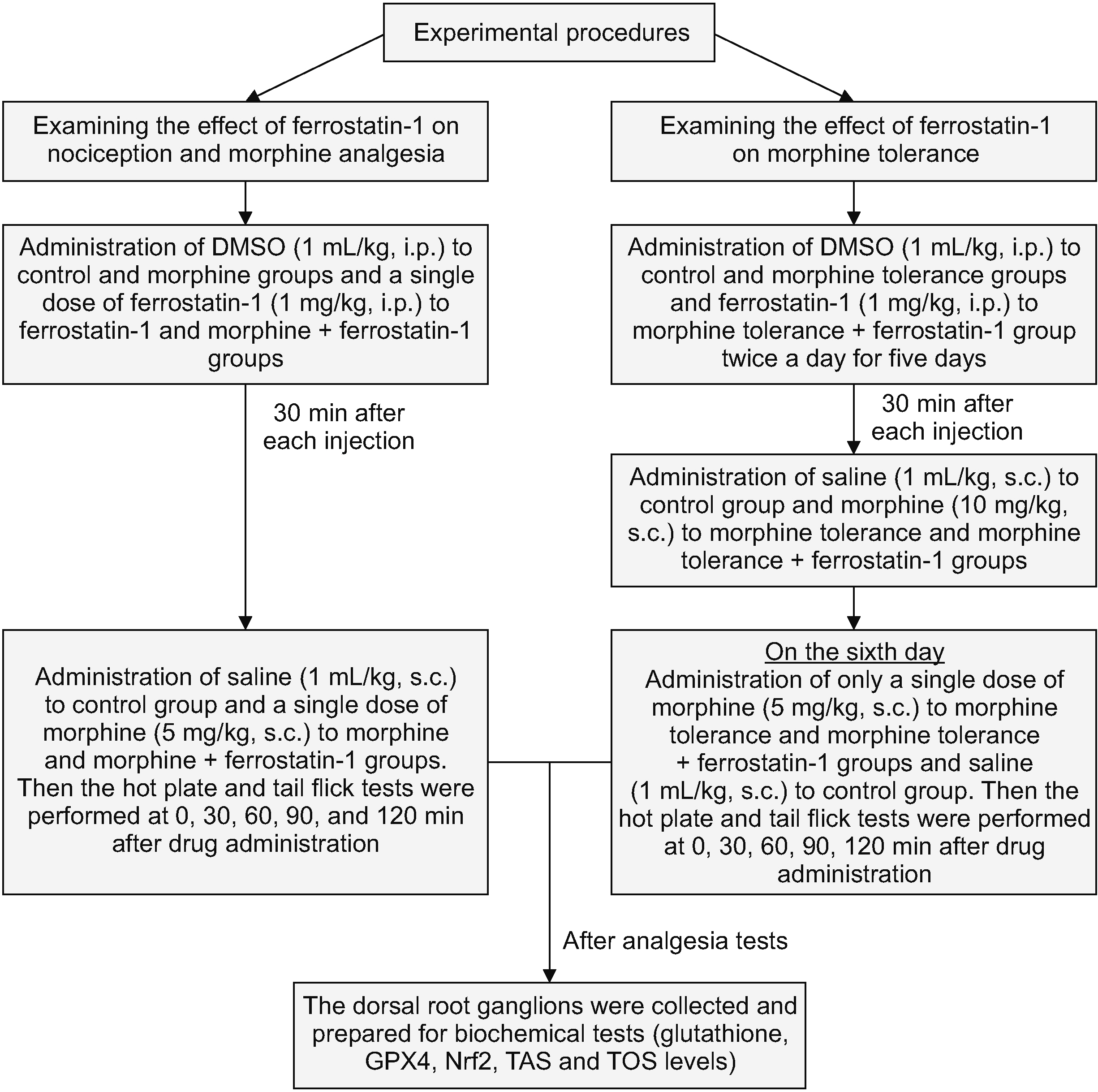
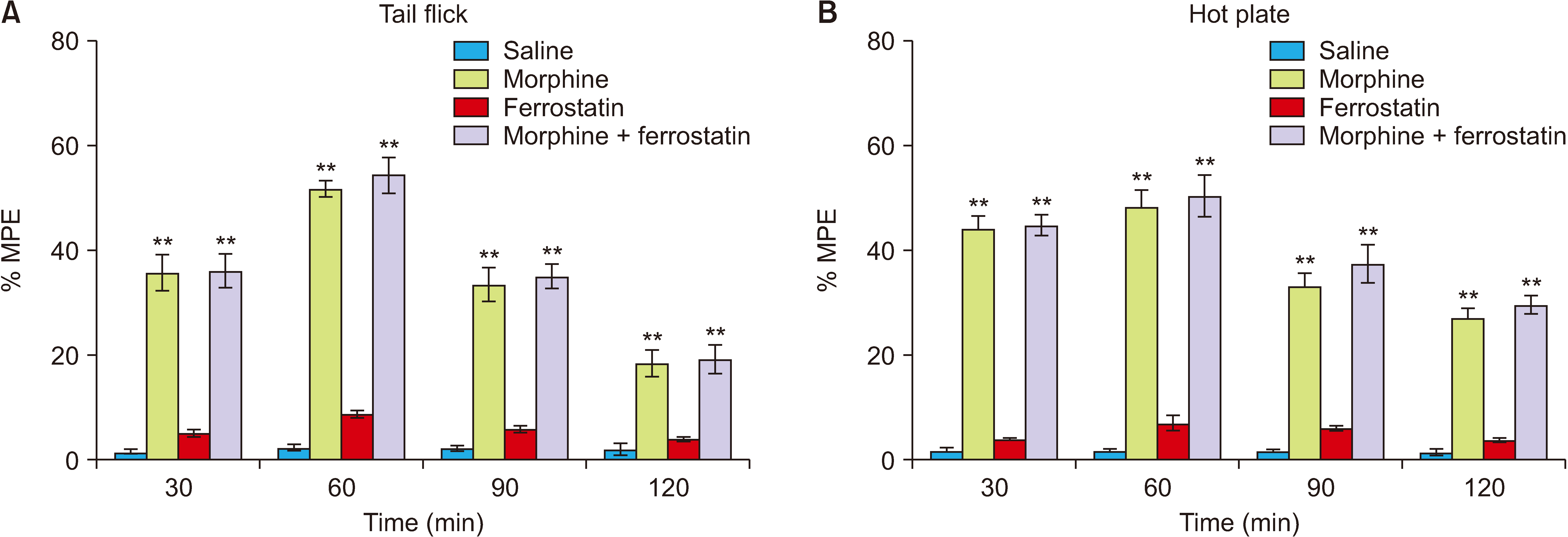
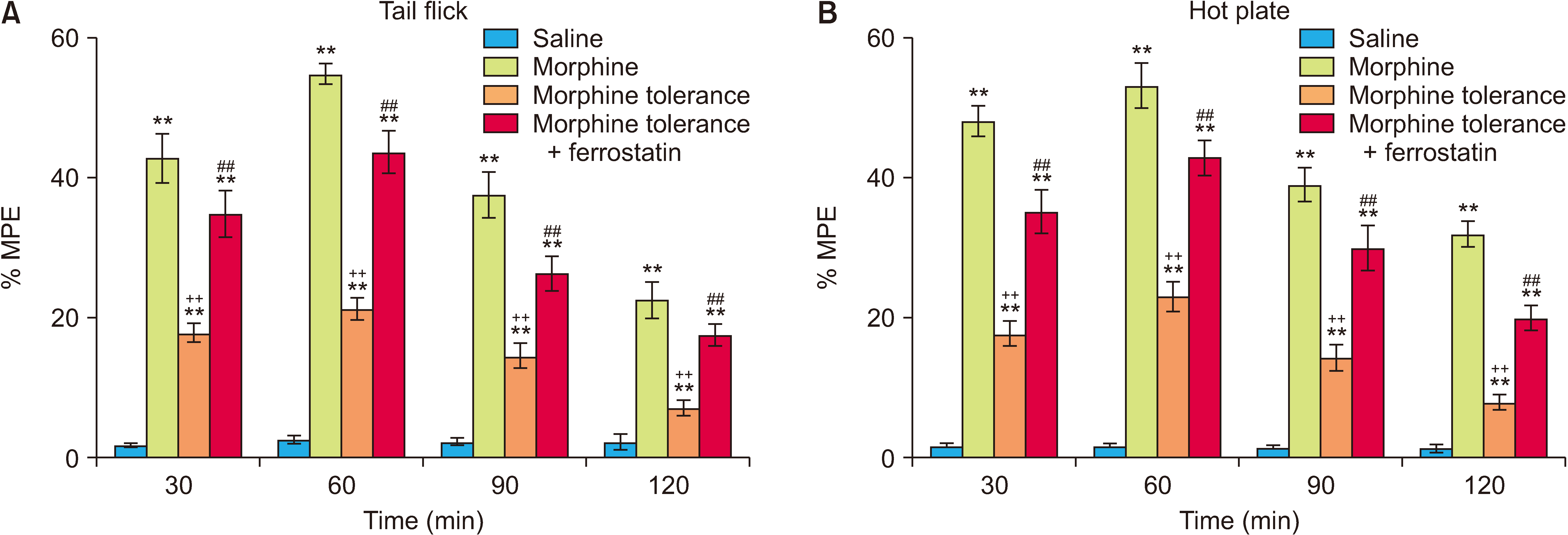
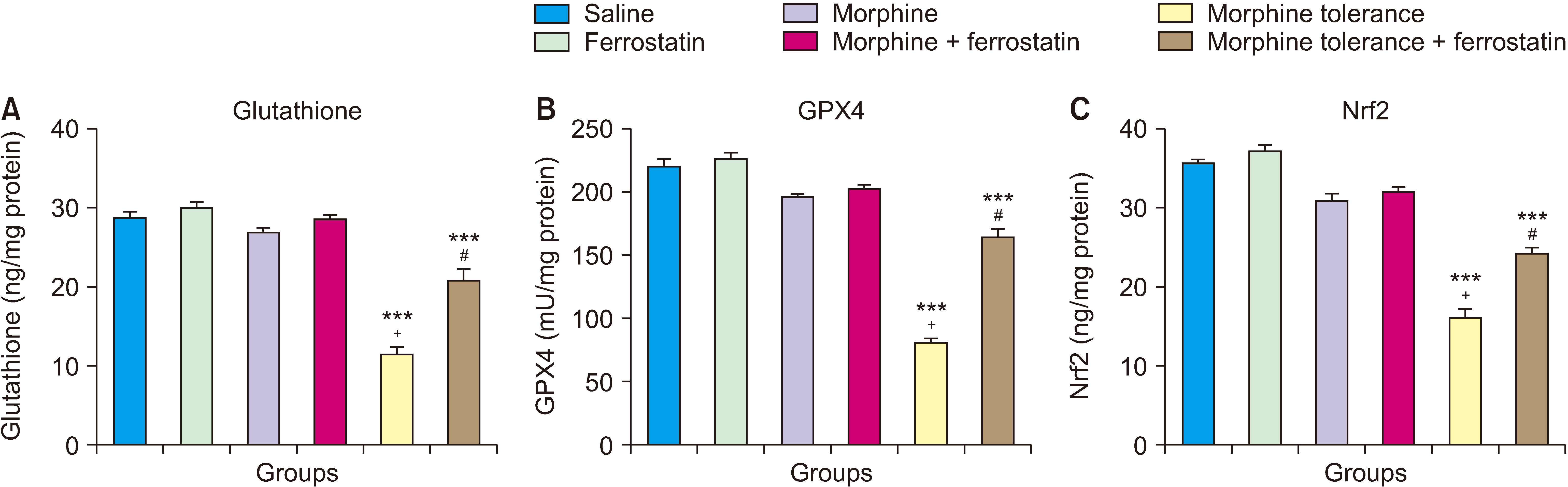
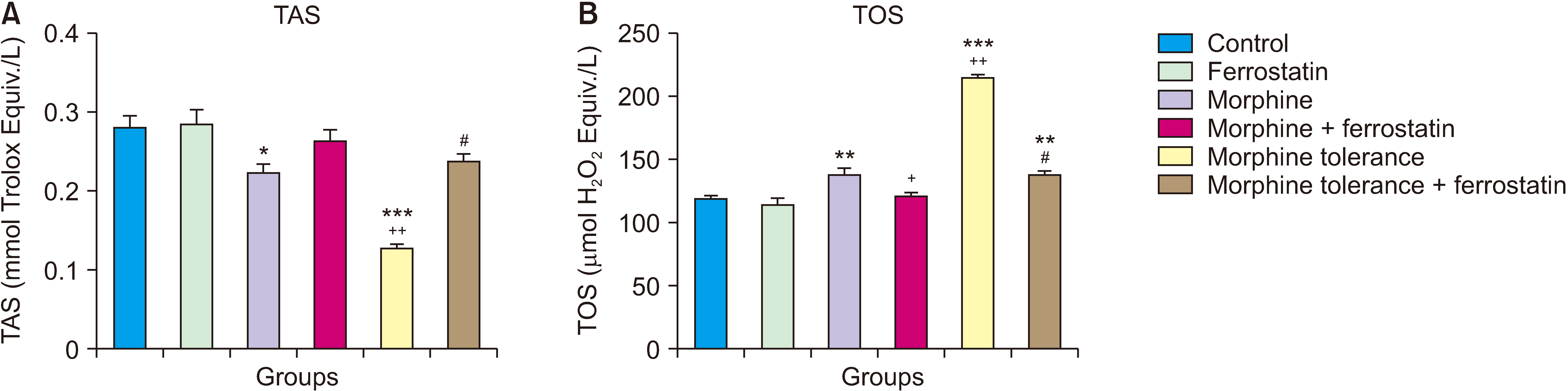
This experiment involved 36 adult male Wistar albino rats with an average weight ranging from 220 to 260 g. These rats were categorized into six groups: Control, single dose ferrostatin-1, single dose morphine, single dose ferrostatin-1 + morphine, morphine tolerance (twice daily for five days), and ferrostatin-1 + morphine tolerance (twice daily for five days). The antinociceptive action was evaluated using both the hot plate and tail-flick tests. After completing the analgesic tests, tissue samples were gathered from the dorsal root ganglia (DRG) for subsequent analysis. The levels of glutathione, glutathione peroxidase 4 (GPX4), and nuclear factor erythroid 2-related factor 2 (Nrf2), along with the measurements of total oxidant status (TOS) and total antioxidant status (TAS), were assessed in the tissues of the DRG.
Results
After tolerance development, the administration of ferrostatin-1 resulted in a significant decrease in morphine tolerance (P < 0.001). Additionally, ferrostatin-1 treatment led to elevated levels of glutathione, GPX4, Nrf2, and TOS (P < 0.001), while simultaneously causing a decrease in TAS levels (P < 0.001).
Conclusions
The study found that ferrostatin-1 can reduce morphine tolerance by suppressing ferroptosis and reducing oxidative stress in DRG neurons, suggesting it as a potential therapy for preventing morphine tolerance.
Keyword
Figure
Reference
-
1. de Guglielmo G, Kallupi M, Scuppa G, Stopponi S, Demopulos G, Gaitanaris G, et al. 2014; Analgesic tolerance to morphine is regulated by PPARγ. Br J Pharmacol. 171:5407–16. DOI: 10.1111/bph.12851. PMID: 25048682. PMCID: PMC4294048.2. Yadlapalli JSK, Dogra N, Walbaum AW, Wessinger WD, Prather PL, Crooks PA, et al. 2017; Evaluation of analgesia, tolerance, and the mechanism of action of morphine-6-O-sulfate across multiple pain modalities in Sprague-Dawley rats. Anesth Analg. 125:1021–31. DOI: 10.1213/ANE.0000000000002006. PMID: 28489639. PMCID: PMC5561516.
Article3. Wilson-Poe AR, Jeong HJ, Vaughan CW. 2017; Chronic morphine reduces the readily releasable pool of GABA, a presynaptic mechanism of opioid tolerance. J Physiol. 595:6541–55. DOI: 10.1113/JP274157. PMID: 28815604. PMCID: PMC5638879.
Article4. Trivedi M, Shah J, Hodgson N, Byun HM, Deth R. 2014; Morphine induces redox-based changes in global DNA methylation and retrotransposon transcription by inhibition of excitatory amino acid transporter type 3-mediated cysteine uptake. Mol Pharmacol. 85:747–57. DOI: 10.1124/mol.114.091728. PMID: 24569088. PMCID: PMC3990020.
Article5. Yang B, Li R, Michael Greenlief C, Fritsche KL, Gu Z, Cui J, et al. 2018; Unveiling anti-oxidative and anti-inflammatory effects of docosahexaenoic acid and its lipid peroxidation product on lipopolysaccharide-stimulated BV-2 microglial cells. J Neuroinflammation. 15:202. DOI: 10.1186/s12974-018-1232-3. PMID: 29986724. PMCID: PMC6038194.6. Ward RJ, Zucca FA, Duyn JH, Crichton RR, Zecca L. 2014; The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol. 13:1045–60. DOI: 10.1016/S1474-4422(14)70117-6. PMID: 25231526.7. Ghadery C, Pirpamer L, Hofer E, Langkammer C, Petrovic K, Loitfelder M, et al. 2015; R2* mapping for brain iron: associations with cognition in normal aging. Neurobiol Aging. 36:925–32. DOI: 10.1016/j.neurobiolaging.2014.09.013. PMID: 25443291.
Article8. Mancardi D, Mezzanotte M, Arrigo E, Barinotti A, Roetto A. 2021; Iron overload, oxidative stress, and ferroptosis in the failing heart and liver. Antioxidants (Basel). 10:1864. DOI: 10.3390/antiox10121864. PMID: 34942967. PMCID: PMC8698778.9. Yang WS, iRamaratnam R Sr, Welsch ME, Shimada K, Skouta R, Viswanathan VS, et al. 2014; Regulation of ferroptotic cancer cell death by GPX4. Cell. 156:317–31. DOI: 10.1016/j.cell.2013.12.010. PMID: 24439385. PMCID: PMC4076414.
Article10. Skouta R, Dixon SJ, Wang J, Dunn DE, Orman M, Shimada K, et al. 2014; Ferrostatins inhibit oxidative lipid damage and cell death in diverse disease models. J Am Chem Soc. 136:4551–6. DOI: 10.1021/ja411006a. PMID: 24592866. PMCID: PMC3985476.
Article11. Chen X, Zhang B, Liu T, Feng M, Zhang Y, Zhang C, et al. 2019; Liproxstatin-1 attenuates morphine tolerance through inhibiting spinal ferroptosis-like cell death. ACS Chem Neurosci. 10:4824–33. DOI: 10.1021/acschemneuro.9b00539. PMID: 31682397.
Article12. Xie Y, Hou W, Song X, Yu Y, Huang J, Sun X, et al. 2016; Ferroptosis: process and function. Cell Death Differ. 23:369–79. DOI: 10.1038/cdd.2015.158. PMID: 26794443. PMCID: PMC5072448.
Article13. Ubellacker JM, Tasdogan A, Ramesh V, Shen B, Mitchell EC, Martin-Sandoval MS, et al. 2020; Lymph protects metastasizing melanoma cells from ferroptosis. Nature. 585:113–8. DOI: 10.1038/s41586-020-2623-z. PMID: 32814895. PMCID: PMC7484468.
Article14. Bai L, Yan F, Deng R, Gu R, Zhang X, Bai J. 2021; Thioredoxin-1 rescues MPP+/MPTP-induced ferroptosis by increasing glutathione peroxidase 4. Mol Neurobiol. 58:3187–97. DOI: 10.1007/s12035-021-02320-1. PMID: 33634378.
Article15. Miotto G, Rossetto M, Di Paolo ML, Orian L, Venerando R, Roveri A, et al. 2020; Insight into the mechanism of ferroptosis inhibition by ferrostatin-1. Redox Biol. 28:101328. DOI: 10.1016/j.redox.2019.101328. PMID: 31574461. PMCID: PMC6812032.16. Ye Q, Zeng C, Luo C, Wu Y. 2020; Ferrostatin-1 mitigates cognitive impairment of epileptic rats by inhibiting P38 MAPK activation. Epilepsy Behav. 103:106670. DOI: 10.1016/j.yebeh.2019.106670. PMID: 31864943.17. Chu J, Liu CX, Song R, Li QL. 2020; Ferrostatin-1 protects HT-22 cells from oxidative toxicity. Neural Regen Res. 15:528–36. DOI: 10.4103/1673-5374.266060. PMID: 31571665. PMCID: PMC6921338.
Article18. Avcı O, Taşkıran AŞ. 2020; Anakinra, an interleukin-1 receptor antagonist, increases the morphine analgesic effect and decreases morphine tolerance development by modulating oxidative stress and endoplasmic reticulum stress in rats. Turk J Med Sci. 50:2048–58. DOI: 10.3906/sag-2005-256. PMID: 32659878. PMCID: PMC7775719.
Article19. Li X, Deng Y, Xiang P, Du J, Liang J. 2021; Ferrostatin-1 attenuates mechanical hypersensitivity in rats with streptozotocin-induced diabetes by inhibiting spinal ferroptosis. Research Square. doi: 10.21203/rs.3.rs-592244/v1. DOI: 10.21203/rs.3.rs-592244/v1.20. Baser T, Ozdemir E, Filiz AK, Taskiran AS, Gursoy S. 2021; Ghrelin receptor agonist hexarelin attenuates antinociceptive tolerance to morphine in rats. Can J Physiol Pharmacol. 99:461–7. DOI: 10.1139/cjpp-2020-0218. PMID: 32893668.
Article21. Taştemur Y, Taşkıran AŞ, Altun A, Filiz AK, Gülmez K, Çimen K, et al. 2020; Role of dopaminergic system in oxytocin analgesia: the missing part in a puzzle. Trop J Pharm Res. 19:1087–92. DOI: 10.4314/tjpr.v19i5.26.
Article22. Modi AD, Parekh A, Pancholi YN. 2023; Evaluating pain behaviours: widely used mechanical and thermal methods in rodents. Behav Brain Res. 446:114417. DOI: 10.1016/j.bbr.2023.114417. PMID: 37003494.
Article23. Taskiran AS, Avci O. 2021; Effect of captopril, an angiotensin-converting enzyme inhibitor, on morphine analgesia and tolerance in rats, and elucidating the inflammation and endoplasmic reticulum stress pathway in this effect. Neurosci Lett. 741:135504. DOI: 10.1016/j.neulet.2020.135504. PMID: 33197521.
Article24. Taskiran AS, Ergul M, Gunes H, Ozturk A, Sahin B, Ozdemir E. 2021; The effects of proton pump inhibitors (pantoprazole) on pentylenetetrazole-induced epileptic seizures in rats and neurotoxicity in the SH-SY5Y human neuroblastoma cell line. Cell Mol Neurobiol. 41:173–83. DOI: 10.1007/s10571-020-00956-6. PMID: 32862257.
Article25. Erel O. 2004; A novel automated method to measure total antioxidant response against potent free radical reactions. Clin Biochem. 37:112–9. DOI: 10.1016/j.clinbiochem.2003.10.014. PMID: 14725941.
Article26. Erel O. 2005; A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 38:1103–11. DOI: 10.1016/j.clinbiochem.2005.08.008. PMID: 16214125.27. Dogan M. 2022; Assessment of mechanism involved in the apoptotic and anti-cancer activity of Quercetin and Quercetin-loaded chitosan nanoparticles. Med Oncol. 39:176. DOI: 10.1007/s12032-022-01820-x. PMID: 35999475.
Article28. Unal M, Gursoy S, Altun A, Duger C, Kol IO, Kaygusuz K, et al. 2013; Ineffective doses of dexmedetomidine potentiates the antinociception induced by morphine and fentanyl in acute pain model. Korean J Physiol Pharmacol. 17:417–22. DOI: 10.4196/kjpp.2013.17.5.417. PMID: 24227942. PMCID: PMC3823954.
Article29. Shen L, Lin D, Li X, Wu H, Lenahan C, Pan Y, et al. 2020; Ferroptosis in acute central nervous system injuries: the future direction? Front Cell Dev Biol. 8:594. DOI: 10.3389/fcell.2020.00594. PMID: 32760721. PMCID: PMC7373735.
Article30. Lee YS, Lee DH, Choudry HA, Bartlett DL, Lee YJ. 2018; Ferroptosis-induced endoplasmic reticulum stress: cross-talk between ferroptosis and apoptosis. Mol Cancer Res. 16:1073–6. DOI: 10.1158/1541-7786.MCR-18-0055. PMID: 29592897. PMCID: PMC6030493.31. Alvarez SW, Sviderskiy VO, Terzi EM, Papagiannakopoulos T, Moreira AL, Adams S, et al. 2017; NFS1 undergoes positive selection in lung tumours and protects cells from ferroptosis. Nature. 551:639–43. Erratum in. DOI: 10.1038/nature24637. PMID: 29168506. PMCID: PMC5808442.32. Doll S, Conrad M. 2017; Iron and ferroptosis: a still ill-defined liaison. IUBMB Life. 69:423–34. DOI: 10.1002/iub.1616. PMID: 28276141.33. Lewerenz J, Ates G, Methner A, Conrad M, Maher P. 2018; Oxytosis/ferroptosis-(Re-) emerging roles for oxidative stress-dependent non-apoptotic cell death in diseases of the central nervous system. Front Neurosci. 12:214. DOI: 10.3389/fnins.2018.00214. PMID: 29731704. PMCID: PMC5920049.
Article34. An S, Shi J, Li Z, Feng M, Cao G. 2022; The effects of acrylamide-mediated dorsal root ganglion neurons injury on ferroptosis. Hum Exp Toxicol. 41:9603271221129786. DOI: 10.1177/09603271221129786. PMID: 36154307.
Article35. Li Q, Han X, Lan X, Gao Y, Wan J, Durham F, et al. 2017; Inhibition of neuronal ferroptosis protects hemorrhagic brain. JCI Insight. 2:e90777. DOI: 10.1172/jci.insight.90777. PMID: 28405617. PMCID: PMC5374066.
Article36. Alim I, Caulfield JT, Chen Y, Swarup V, Geschwind DH, Ivanova E, et al. 2019; Selenium drives a transcriptional adaptive program to block ferroptosis and treat stroke. Cell. 177:1262–79.e25. DOI: 10.1016/j.cell.2019.03.032. PMID: 31056284.37. Hervera A, Negrete R, Leánez S, Martín-Campos JM, Pol O. 2011; Peripheral effects of morphine and expression of μ-opioid receptors in the dorsal root ganglia during neuropathic pain: nitric oxide signaling. Mol Pain. 7:25. DOI: 10.1186/1744-8069-7-25. PMID: 21486477. PMCID: PMC3094254.38. Bannon AW, Malmberg AB. 2007; Models of nociception: hot-plate, tail-flick, and formalin tests in rodents. Curr Protoc Neurosci. Chapter 8:Unit 8.9. DOI: 10.1002/0471142301.ns0809s41. PMID: 18428666.39. Piel MJ, Kroin JS, van Wijnen AJ, Kc R, Im HJ. 2014; Pain assessment in animal models of osteoarthritis. Gene. 537:184–8. DOI: 10.1016/j.gene.2013.11.091. PMID: 24333346. PMCID: PMC3950312.
Article40. Mitrovic I, Margeta-Mitrovic M, Bader S, Stoffel M, Jan LY, Basbaum AI. 2003; Contribution of GIRK2-mediated postsynaptic signaling to opiate and alpha 2-adrenergic analgesia and analgesic sex differences. Proc Natl Acad Sci U S A. 100:271–6. DOI: 10.1073/pnas.0136822100. PMID: 12496346. PMCID: PMC140949.41. Pizzorno J. 2014; Glutathione! Integr Med (Encinitas). 13:8–12.42. Cao JY, Dixon SJ. 2016; Mechanisms of ferroptosis. Cell Mol Life Sci. 73:2195–209. DOI: 10.1007/s00018-016-2194-1. PMID: 27048822. PMCID: PMC4887533.
Article43. Abdel-Zaher AO, Mostafa MG, Farghly HM, Hamdy MM, Omran GA, Al-Shaibani NK. 2013; Inhibition of brain oxidative stress and inducible nitric oxide synthase expression by thymoquinone attenuates the development of morphine tolerance and dependence in mice. Eur J Pharmacol. 702:62–70. DOI: 10.1016/j.ejphar.2013.01.036. PMID: 23376567.44. Ma Q. 2013; Role of nrf2 in oxidative stress and toxicity. Annu Rev Pharmacol Toxicol. 53:401–26. DOI: 10.1146/annurev-pharmtox-011112-140320. PMID: 23294312. PMCID: PMC4680839.
Article45. Song X, Long D. 2020; Nrf2 and ferroptosis: a new research direction for neurodegenerative diseases. Front Neurosci. 14:267. DOI: 10.3389/fnins.2020.00267. PMID: 32372896. PMCID: PMC7186402.
Article46. Reymond S, Vujić T, Schvartz D, Sanchez JC. 2022; Morphine-induced modulation of Nrf2-antioxidant response element signaling pathway in primary human brain microvascular endothelial cells. Sci Rep. 12:4588. DOI: 10.1038/s41598-022-08712-0. PMID: 35301408. PMCID: PMC8931063.
Article47. Skrabalova J, Drastichova Z, Novotny J. 2013; Morphine as a potential oxidative stress-causing agent. Mini Rev Org Chem. 10:367–72. DOI: 10.2174/1570193X113106660031. PMID: 24376392. PMCID: PMC3871421.
Article48. Zöllner C, Mousa SA, Fischer O, Rittner HL, Shaqura M, Brack A, et al. 2008; Chronic morphine use does not induce peripheral tolerance in a rat model of inflammatory pain. J Clin Invest. 118:1065–73. DOI: 10.1172/JCI25911. PMID: 18246198. PMCID: PMC2214843.
Article49. Blomqvist KJ, Dudek KA, Viisanen H, Mätlik K, Ahlström FHG, Laitila J, et al. 2022; Antagonism of peripheral opioid receptors by methylnaltrexone does not prevent morphine tolerance in rats. J Neurosci Res. 100:329–38. DOI: 10.1002/jnr.24638. PMID: 32459013.50. Bartley EJ, Fillingim RB. 2013; Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 111:52–8. DOI: 10.1093/bja/aet127. PMID: 23794645. PMCID: PMC3690315.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Salidroside attenuates sepsis-induced acute lung injury by inhibiting ferroptosis-dependent pathway
- Protaetia brevitarsis larvae extract protects against lipopolysaccharidesinduced ferroptosis and inflammation by inhibiting acid sphingomyelinase
- Inhibition of Fatty Acid β-Oxidation by Fatty Acid Binding Protein 4 Induces Ferroptosis in HK2 Cells Under High Glucose Conditions
- Intrathecal Lamotrigine Attenuates Antinociceptive Morphine Tolerance and Suppresses Spinal Glial Cell Activation in Morphine-Tolerant Rats
- Ferroptosis and its role in gastric and colorectal cancers