J Korean Med Sci.
2021 Aug;36(33):e213. 10.3346/jkms.2021.36.e213.
Pediatric Sedation in the Emergency Department: Trends from a Nationwide Population-based Study in Korea, 2007–2018
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2519353
- DOI: http://doi.org/10.3346/jkms.2021.36.e213
Abstract
- Background
Pediatric sedation in the emergency department (ED) is widely performed in Korea; thus exploring the trends of its use is necessary. This study aimed to investigate the characteristics of patients and sedatives use in the ED and verify their changes over recent years.
Methods
A nationwide population-based retrospective study was conducted including pediatric patients aged ≤ 15 years who received sedative medication in the ED and were discharged during 2007–2018, using the Korean Health Insurance Review and Assessment Service database. Patient characteristics (age, sex, level of ED, and diagnosis) and type of sedative used were analyzed.
Results
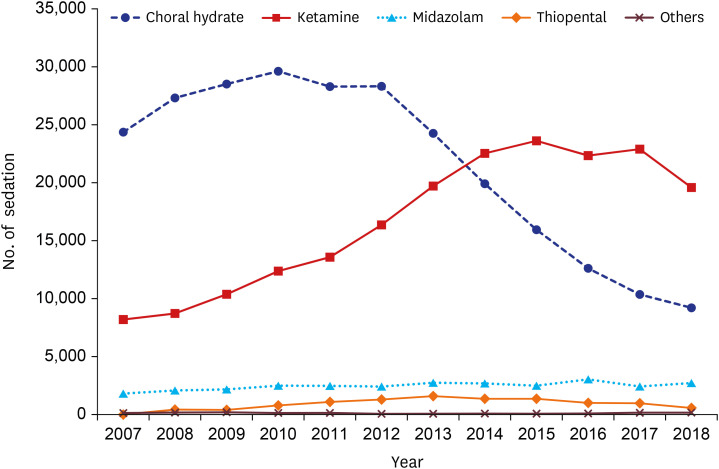
Sedation was performed in total 468,221 visits during 2007–2018 (399,320 visits, at least 3.8% of overall ED visits during 2009–2018). Among these, 71.0% were children aged 1–3 years and 93.5% were sedated to support diagnosis of injury. An increase in total sedation was observed in patients aged 4–6 years during the study period (from 13.8% to 21.8%). A gradual decrease in the use of chloral hydrate (CH) compared with an increase in ketamine use was observed (CH, from 70.6% to 28.6%; ketamine, from 23.8% to 60.7%). Therefore, ketamine was the most used sedative since 2014. The most frequently used sedatives over the study period differed according to age groups (CH in <1 year and 1–3 years; ketamine in 4–6 years and 7–10 years; and midazolam in 11–15 years).
Conclusions
The characteristics of patients related to sedatives use in the ED have changed over time. These changes should be considered in the development of future Korean guidelines regarding pediatric sedation in the ED.
Keyword
Figure
Reference
-
1. Krieser D, Kochar A. Paediatric procedural sedation within the emergency department. J Paediatr Child Health. 2016; 52(2):197–203. PMID: 27062624.
Article2. Bhatt M, Johnson DW, Chan J, Taljaard M, Barrowman N, Farion KJ, et al. Risk factors for adverse events in emergency department procedural sedation for children. JAMA Pediatr. 2017; 171(10):957–964. PMID: 28828486.
Article3. Bellolio MF, Puls HA, Anderson JL, Gilani WI, Murad MH, Barrionuevo P, et al. Incidence of adverse events in paediatric procedural sedation in the emergency department: a systematic review and meta-analysis. BMJ Open. 2016; 6(6):e011384.
Article4. Coté CJ, Wilson S. American Academy of Pediatrics. American Academy of Pediatric Dentistry. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures. Pediatrics. 2019; 143(6):e20191000. PMID: 31138666.
Article5. Sahyoun C, Krauss B. Clinical implications of pharmacokinetics and pharmacodynamics of procedural sedation agents in children. Curr Opin Pediatr. 2012; 24(2):225–232. PMID: 22245909.
Article6. Green SM, Roback MG, Krauss BS, Miner JR, Schneider S, Kivela PD, et al. Unscheduled procedural sedation: a multidisciplinary consensus practice guideline. Ann Emerg Med. 2019; 73(5):e51–e65. PMID: 31029297.
Article7. Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011; 57(5):449–461. PMID: 21256625.
Article8. Bhatt M, Johnson DW, Taljaard M, Chan J, Barrowman N, Farion KJ, et al. Association of preprocedural fasting with outcomes of emergency department sedation in children. JAMA Pediatr. 2018; 172(7):678–685. PMID: 29800944.
Article9. Kamat PP, McCracken CE, Simon HK, Stormorken A, Mallory M, Chumpitazi CE, et al. Trends in outpatient procedural sedation: 2007–2018. Pediatrics. 2020; 145(5):e20193559. PMID: 32332053.
Article10. Seo JS, Kim DK, Kang Y, Kyong YY, Kim JJ, Ahn JY, et al. Current practices for paediatric procedural sedation and analgesia in emergency departments: results of a nationwide survey in Korea. Emerg Med J. 2013; 30(3):e24. PMID: 22518059.
Article11. D’Agostino J, Terndrup TE. Chloral hydrate versus midazolam for sedation of children for neuroimaging: a randomized clinical trial. Pediatr Emerg Care. 2000; 16(1):1–4. PMID: 10698133.
Article12. Finnemore A, Toulmin H, Merchant N, Arichi T, Tusor N, Cox D, et al. Chloral hydrate sedation for magnetic resonance imaging in newborn infants. Paediatr Anaesth. 2014; 24(2):190–195. PMID: 24387147.
Article13. Coté CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics. 2000; 106(4):633–644. PMID: 11015502.
Article14. Ratnapalan S. Chloral hydrate sedation in children. Clin Pediatr (Phila). 2014; 53(10):933–936. PMID: 24198315.
Article15. Nordt SP, Rangan C, Hardmaslani M, Clark RF, Wendler C, Valente M. Pediatric chloral hydrate poisonings and death following outpatient procedural sedation. J Med Toxicol. 2014; 10(2):219–222. PMID: 24532346.
Article16. Jang HY, Jung JH, Kyong YY, Kim KH, Kim DK, Kim MR, et al. Korean guidelines for pediatric procedural sedation and analgesia. J Korean Soc Emerg Med. 2012; 23(3):303–314.17. Miller AF, Monuteaux MC, Bourgeois FT, Fleegler EW. Variation in pediatric procedural sedations across children's hospital emergency departments. Hosp Pediatr. 2018; 8(1):36–43. PMID: 29233853.
Article18. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32(5):718–728. PMID: 28378543.
Article19. Kim DK. Procedural sedation and analgesia in pediatric emergency department. Pediatr Emerg Med J. 2018; 5(2):31–37.
Article20. Burger RK, Figueroa J, McCracken C, Mallory MD, Kamat PP. Sedatives used in children to obtain head CT in the emergency department. Am J Emerg Med. 2021; 44:198–202. PMID: 32107128.
Article21. Kim DK, Kwak YH, Lee SJ, Jung JY, Song BK, Lee JH, et al. A national survey of current practice patterns and preparedness of pediatric emergency care in Korea. J Korean Soc Emerg Med. 2012; 23(1):126–131.22. Kwak YH. Current status and future direction of pediatric emergency medicine in Korea. Pediatr Emerg Med J. 2014; 1(1):1–10.
Article23. Je S, Hong JS, Lee JS. A plan for strengthening pediatric emergency care: establishment of pediatric certified emergency center. Pediatr Emerg Med J. 2017; 4(2):46–50.
Article24. Kwak YH, Park JD. Background and necessity of implementing the subspecialty of pediatric emergency medicine in Korea. Pediatr Emerg Med J. 2020; 7(2):57–60.
Article25. Green SM, Roback MG, Krauss B, Brown L, McGlone RG, Agrawal D, et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009; 54(2):158–168.e1-4. PMID: 19201064.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Procedural sedation and analgesia in pediatric emergency department
- A Single Pediatric Surgeon Working in a Single Center: Was There a Change in the Pediatric Surgeon's Role Following 25 Years of Service in Suwon City?
- Sedation of the Pediatric Dental Patient
- Trends in Dental Sedation of Korean Children and Adolescents
- Trends of conscious sedation in the Department of Pediatric Dentistry at the Dankook University Dental Hospital for 11 Years